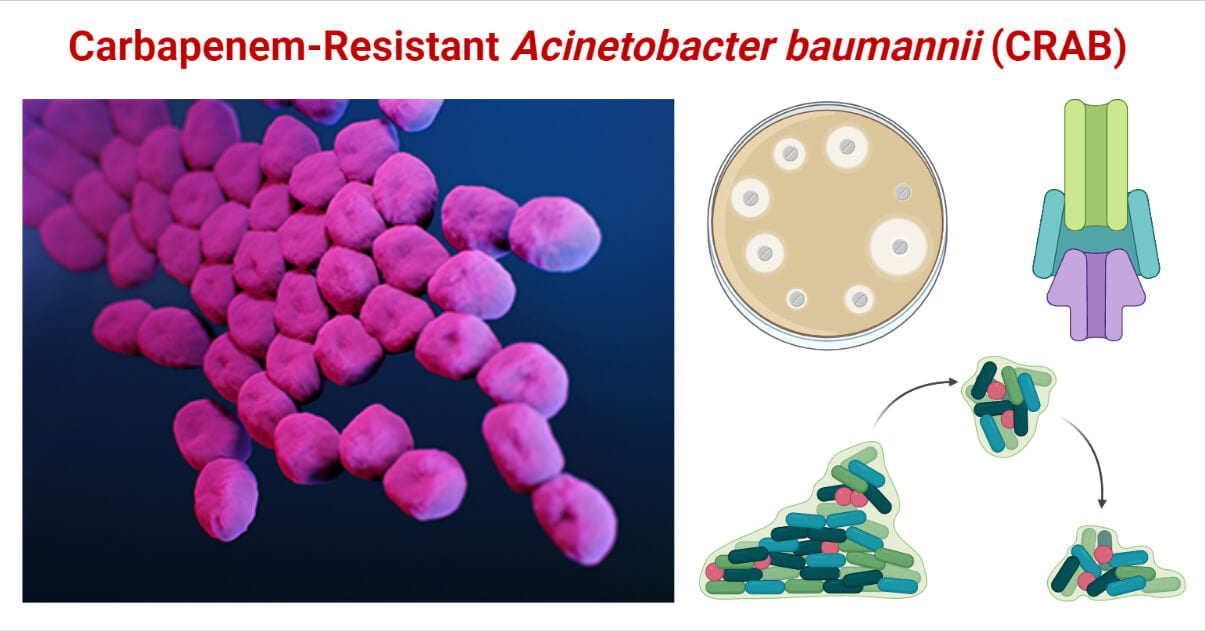
Carbapenem-Resistant Acinetobacter baumannii (CRAB) is a group of A. baumannii which have developed resistance against the carbapenems.
Acinetobacter is a genus of aerobic, glucose non-fermentative, rod-shaped (more precisely, cocco-bacilli), Gram-negative Gammaproteobacteria in the family Moraxellaceae of phylum Pseudomonadota.
Interesting Science Videos
What is Acinetobacter baumannii?
Acinetobacter baumannii is a pathogenic species of this genus included in the Acb complex (Acinetobacter calcoaceticus-baumannii complex). It is responsible mainly for nosocomial (hospital-acquired) infections. A. baumannii is Gram-negative, strictly aerobic, non-fermentative, usually non-motile, oxidase-negative, and cocco-bacilli.
It is also known as “Iraqibacter”. Paul Baumann first discovered it, and the species is named after him.
It is ubiquitous in habitat and mostly found in soil and water. Due to their capacity to form a biofilm, they can survive in a dry habitat, like medical devices, inanimate surfaces, skin, etc., and infect hospitalized patients.
Acinetobacter baumannii Morphology
- Pleomorphic (Short Gram-negative cocco-bacilli; bacilli during a lag phase which eventually becomes coccoid or cocco-bacilli at stationary phase)
- 1.0 – 1.5 micron by 1.5 – 2.5 micron during the lag phase
- 0.6 – 0.9 micron by 1.0 – 1.5 micron during the stationary phase
- Lack flagella but contain fimbria.
- Usually, show twitching motility and surface-associated motility
- Capsulated
- Non-sporing
Acinetobacter baumannii Biochemical Characteristics
- Strict aerobes
- Glucose non-fermentative
- Oxidase negative
- IMViC test = -ve, -ve, -ve, +ve (- – – +)
- Urease, Nitrate, and DNase negative
- TSI test = Alkaline / Alkaline, no gas, no H2S
Acinetobacter baumannii Cultural Characteristics
Aerobic incubation with a temperature range from 20 – 44°C; the optimum temperature of 35 (±2)°C.
Non-fastidious in nutrient requirement.
Nutrient Agar, MacConkey Agar, and Blood Agar are commonly used in laboratories.
- Nutrient Agar = 1-3 mm, Circular, Smooth, Non-mucoid, Greyish-White, Opaque colonies.
- MacConkey Agar = 2-3 mm, Circular, Non-lactose fermentative, Opaque colonies.
- Blood Agar = 2-3 mm, Non-hemolytic, Circular, Grey, Opaque colonies.
CHROMAgar Acinetobacter is a selective media; Acinetobacter baumannii produces “red” colonies while other Gram-negative bacteria produce “blue” colonies.
Acinetobacter baumannii Virulence Factors
Currently, well-studied virulence factors of A. baumannii with their proposed roles are summarized in the following table, viz.:
| S.N. | Virulence Factors | Roles in Pathogenesis |
| 1. | Pili | Helps in biofilm formation, adherence, and bacterial motility, |
| 2. | Porins – They are proteins in an outer membrane that regulate bacterial permeability. – OmpA, Omp 22, Omp 33-36, CarO, and OprD-like are the most important porins. – OmpA is the most abundant and the most important virulence factor. | OmpA is responsible for: – Inducing apoptosis in epithelial cells – Adherence and invasionInhibit complement-mediated killing – Antimicrobial resistance – Facilitates biofilm formation and motility – Biogenesis of OMV (outer membrane vesicles) Omp 33-36 is responsible for: – Cytotoxicity – Invasion of epithelial cells – Induces apoptosis – Confer resistance against Carbapenems Omp 22 is associated with the production of inflammatory cytokines and chemokines. Other roles are still unclear. CarO and OprD-like are antigenic and add to virulence, but their exact roles are unclear. |
| 3. | Capsule (Capsular Polysaccharides and Lipopolysaccharides) – Most pathogenic strains are capsulated. Capsules are formed by polysaccharides and lipopolysaccharides (LPS). | Capsular polysaccharides are responsible for: – Facilitates survival in soft tissues of hosts – Adherence and biofilm formation – Confer resistance against peptide antibiotics – Provide resistance against human serum Capsular LPS are responsible for: – AdherenceEndotoxicity – Induces production of Tumor Necrosis Factor (TNF) and Interleukin 8 – Provide resistance against human serumConfer resistance against Colistin |
| 4. | Phospholipase – It is a lipolytic enzyme that hydrolyzes phospholipids. – Phospholipase C (PLC) and phospholipase D (PLD) are important virulence factors of A. baumannii. | PLC and PLD are responsible for: – Cytotoxic effect on epithelial cells – Resistance against human serum – Cellular invasion |
| 5. | Outer Membrane Vesicles (OMVs) – They are vesicles of 20 – 200 nm secreted by the outer membrane of the bacterium for transportation. – OMVs of A. baumannii contain several virulence factors like OmpA, PLC, PLD, protease, LPS, etc. | OMVs are responsible for: – Delivery of virulence factors to host cells resulting in cytotoxicity – Induces innate immune response – Accumulation of inflammatory cytokines – Horizontal gene transfer of OXA-24 carbapenemase gene. |
| 6. | Metal Acquisition System A. baumannii has 3 types of metal acquisition systems for fulfilling their need for metal ions for cellular metabolisms. Iron acquisition system provides iron in the required form to the bacteria. Acinetobactin, NfuA Fe-S scaffold protein, and iron siderophores are produced by A. baumannii to fulfilling the need for iron. Similarly, Zinc acquisition systems include ZnuABC, ZigA, and ZrlA proteins for meeting the need for zinc. They also provide Zn for the formation of carbapenemase enzymes. Magnesium acquisition system contains MumC and MumT proteins. | Iron acquisition system is responsible for: – Persistence survival within invaded epithelial and alveolar cells – Resistance against Reactive Oxygen Species (ROS) Zinc acquisition system is responsible for: – Persistence survival within epithelial cells – Confer resistance against imipenem Magnesium acquisition system is responsible for: – Persistence survival within epithelial cells – Confer resistance against macrophage proteins and Calprotectin |
| 7. | Protein Secretion System It is molecular machinery that helps in the translocation of proteins and nucleic acids. The secretion system in A. baumannii is of three types; Type II secretory system (T2SS), Type V secretory system (T5SS) and Type VI secretory system (T6SS). | T2SS and T6SS are responsible for: – Secretion of LipA for breaking of lipase – T6SS also aids in colonization and killing other competing bacteria – T5SS aids in biofilm formation and adherence |
| 8. | Penicillin-binding Protein 7/8 and β-Lactamse PER -1 PBPs are the membrane proteins that synthesize peptidoglycans and protect bacterial cells from the action of β-Lactam antibiotics. β-Lactamase is a group of enzymes that hydrolyze β- Lactam rings in β-Lactam antibiotics. PBP 7/8 and β-Lactamase PER-1 in A. baumannii, however, act as important virulence factors. | PBP 7/8 is responsible for: – Provide resistance against human serum – Facilitates survival in soft tissues of the host β-Lactamse PER-1 is responsible for: – Adhesion |
| 9. | CipA It is a protein that binds to plasminogen and inhibits the complement system. | CipA is responsible for: – Degrade fibrinogen and C3b of complement system which protects the bacteria from human serum. |
| 10. | Other virulence factors: Plasminogen binding protein Tuf Surface antigen protein 1 (SurA1) OmpR / EnvZ FhaBC Resistance-nodulation-division-type membrane transporter AbeD | Degrade fibrinogen and C3b Dissemination and serum resistance Cytotoxic effect Adherence and cytotoxic effect Cytotoxic effect |
Acinetobacter baumannii Pathogenesis
Acinetobacter baumannii is an opportunistic pathogen that mainly causes nosocomial infection. They are usually transmitted from inanimate objects in hospital settings, medical devices, and catheters, infected persons (patients) and carriers (hospital staff and their hands or materials), and environmental factors like soil and water. Once they come in contact with musical or epithelial cells, they begin infection.
Once bacteria contact a suitable host surface, they adhere using their adherence factors like pili, porins, surface proteins, LPS, etc. Once attached to the surface, they express virulence factors to colonize and form a biofilm on that site. The bacterial cells then invade and destroy the cells via cytotoxic effects. They escape the host’s immune responses and induce inflammatory responses, apoptosis, cytotoxic effect, and invasion and dissemination to nearby cells.
The pathogenic mechanism and extent of infection vary on the site of infection. Although it is still unclear about the exact mechanism, several models to study bacterial pathogenesis and the host-pathogen relation are established; mammalian model, pneumonia model, sepsis model, non-mammalian models, and in-vitro model.
Acinetobacter baumannii Clinical Manifestations
A. baumannii is mainly associated with a hospital-acquired infection, and community-acquired infections are rare. They had been regarded as low-grade pathogens, but now it is emerging as opportunistic pathogen responsible for several systemic as well as superficial infections. The development of resistance against most of the available antibiotics has made A. baumannii a pathogen of high risk. It is now a member of the ESKAPE group, which includes multi-drug resistant pathogenic bacteria causing most of the hospital-acquired infections.
A. baumannii is frequently associated with the following clinical syndromes:
- Hospital Acquired Pneumonia
Pneumonia is one of the most common infections by A. baumannii in hospitalized patients. It is responsible for Ventilator-associated pneumonia (VAP), and pneumonia in patients in an intensive care unit (ICUs). More than 55% of CRAB infection is associated with respiratory tract, especially pneumonia.
- Blood Stream Infection (BIs) / Bacteremia
A. baumannii is responsible for around 2.5% of nosocomial BIs. A. baumannii Bacteremia is a serious infection with a mortality of 25 to 54%. The infections are common in ICU patients, post-operation patients, patients under immune suppression, venous catheterized patients, patients with burns, and patients with invasive procedures.
- Meningitis
A. baumannii-associated meningitis is infrequent and is mostly reported in patients undergoing neurosurgical procedures, spinal surgery, and immune-suppressed ones.
- Urinary Tract Infections (UTIs)
UTIs by A. baumannii are seen in patients with indwelling urinary catheters and patients with a prolonged hospital stay. It is rarely seen in patients with nephron and urological surgery.
- Skin and Wound Infections
Skin and wound infection is a common manifestation of A. baumannii in prolonged hospitalized patients. Cellulitis, folliculitis, abscess formation, necrotizing fasciitis, rashes and patches and lesions, deep-seated wounds, etc., are common in hospitalized patients with a weak immune system and under antibiotic therapy.
- Cholangitis
Acinetobacter cholangitis (inflammation of the bile duct system) is a rare disease. It is seen in patients with HIV, recent medical procedures involving liver and bile duct areas, and inflammatory bowel diseases.
- Ventriculitis
A. baumannii is associated with catheter-related ventriculitis and ventriculoperitoneal shunt infection. It is commonly seen along with Acinetobacter meningitis, especially in patients undergoing neurosurgical procedures or catheterization, and is life-threatening.
- Infective – endocarditis
A. baumannii infective-endocarditis is a rare but severe and life-threatening infection seen mainly in hospitalized patients undergoing invasive procedures.
- Extensive Soft Tissue Necrosis
Skin and soft tissue infection (SSTI) by A. baumannii were thought uncommon but is frequently reported in patients with wounds and surgical procedures.
- Sinus infection, ocular infection, peritonitis, corneal ulcer, bone infection, etc., are rarely associated with A. baumannii.
What are Carbapenems?
- Carbapenems are the class of beta-lactam antibiotics that can inhibit the beta-lactamase enzymes, resist their action and act against a wide range of bacteria, including beta-lactamase producers. Hence, they possess the broadest spectrum of activity. They are used for treating serious infections or in case of infection by resistant bacteria, so they are also called “antibiotics of last resort”.
- They are the first line of treatment for infections caused by resistant bacterial pathogens like Enterobacteriaceae, A. baumannii, Pseudomonas spp., Streptococcus spp., Mycobacterium tuberculosis complex, Haemophilus influenzae, MRSA, Salmonella serovars, etc.
- Molecularly, carbapenems have a β-lactam ring with a carbon atom replacing sulfur at C-1, and introducing a double bond between C-2 and C-3 of the ring. The side chains are arranged in the trans position, unlike in the cis position like in other β- lactams. Hence, carbapenems are resistant to β- lactamase enzymes like ESBLs, and AmpC β- lactamase. They are, however, susceptible to carbapenemases and Metallo – β- lactamases.
- They act by binding to the penicillin-binding proteins and inhibiting bacterial cell wall synthesis.
- They are classified into two groups; group-1 containing sole member “ERTAPENEM”, and group-2 containing “IMIPENEM”, “MEROPENEM”, and “DORIPENEM”.
What are Carbapenem-Resistant Organisms (CROs)?
- A large group of pathogenic bacteria, whose infections were treated by carbapenems, have now developed several mechanisms to protect themselves from the inhibitory or bactericidal action of carbapenems. Though initially thought to be very effective against a wide range of clinically significant Gram-negative bacteria, carbapenem resistance is rapidly developing in them globally. They are included as organisms of urgent threat requiring urgent countermeasures.
- Some most serious carbapenem-resistant bacteria are:
- Carbapenem resistant Enterobacteriaceae (CRE)
[Carbapenem-resistant Klebsiella pneumoniae is the most important among them]
- Carbapenem resistant Acinetobacter baumannii (CRAB)
- Carbapenem resistant Pseudomonas aeruginosa (CRPA)
What is Carbapenem-Resistant Acinetobacter baumannii (CRAB)?
- CRAB is a group of A. baumannii which have developed resistance against the carbapenems. CRAB has been labeled as “a priority 1 – critical pathogen” by the WHO since 2017. They are responsible for most of the hospital-acquired infections by Acinetobacter spp. Few antimicrobials are effective against CRAB. Hence they pose very high therapeutic challenges. Moreover, they frequently infect patients on ventilators, ICUs, and catheterized patients, increasing the severity of the illness.
- These bacteria are genetically evolved to protect themselves against carbapenems. They are structurally modified, developed virulence factors to confer resistance, and developed enzyme systems to confer resistance against carbapenems.
Mechanisms of Resistance Against Carbapenems by CRAB
A. baumannii is known to have several intrinsic and acquired mechanisms to resist themselves against carbapenems. Some well-studied resistant mechanisms against carbapenems are:
1. Enzymatic modification of antibiotics
Carbapenem-resistant A. baumannii (CRAB) can produce different types of β- lactamases that hydrolyze the β-lactam ring of carbapenems. Such β-lactamases are called carbapenemases. Carbapenemases can hydrolyze carbapenems, making them ineffective against CRAB.
Carbapenemase synthesized by CRAB can be grouped into three groups:
- Oxacillinase (OXA β-lactamases)
These are class – D β- lactamases that can hydrolyze oxacillin. Not all, but some types of oxacillinase (OXAs) can hydrolyze carbapenem.
Carbapenem hydrolyzing OXAs are the major enzymes synthesized by CRAB. OXAs synthesized by CRAB can be grouped as:
OXA-23-like, OXA-24/40-like, OXA-51-like, OXA-58-like, and OXA-143-like.
Among them, the OXA-23 enzyme is most frequently found in CRAB.
- Metallo-β-lactamases (MBLs)
These are class-C β-lactamases that contain one or two Zinc ions in their active site and can hydrolyze carbapenems. CRAB is capable of synthesizing different types of MBLs like;
New Delhi metallo-β-lactamases (NDM) group, Verona integron-related metallo-β-lactamase (VIM) group, and Imipenem resistant Pseudomonas (IMP) metallo-β-lactamase group.
NDM-1 is another commonly found carbapenemase in CRAB after OXA-23.
- K. pneumoniae carbapenemase (KPC) β-lactamases
Only a few isolates of CRAB are found to produce KPC β-lactamases, mainly KPC-2 and KPC-3.
2. Modification in membrane permeability
CRAB has been found to have modified porin channels. Reduced expression of porins like Omp22-36, Omp33-36, Omp37, Omp44, Omp47, and CarO is found in CRAB. This reduced expression prevents carbapenem from entering the bacterial cell, hence, conferring resistance against them.
3. Altered penicillin-binding proteins (PBPs)
Modification in the target sites of antibiotics is a major mechanism adopted by many bacteria to escape the lethal action of any antibiotic. As carbapenems are β- lactams, any alteration in their target, PBPs, can prevent the bacteria against carbapenems.
CRAB show overexpression of altered PBPs which are found to lower the affinity of “Imipenem”.
4. Efflux pumps
A. baumannii have four efflux pumps confer antimicrobial resistance to them; the resistance-nodulation-division superfamily, the multidrug and toxic compound extrusion family, the major facilitator superfamily, and the small multidrug resistance family transporters.
Among these, AbeM efflux pump of the multidrug and toxic compound extrusion family is found to confer resistance against carbapenem, namely “Imipenem”.
The EmrAB-TolC efflux pump is also recently found to confer resistance against “Imipenem” in CRAB.
adeABC efflux pump is another multidrug resistance transporter found to efflux the carbapenems from the cytoplasm of CRAB.
Epidemiology of Carbapenem-Resistant Acinetobacter baumannii (CRAB)
Most of the infections by CRAB are hospital-associated, but community-acquired cases are also emerging lately. Cases are increasing rapidly all around the world, especially in Asian regions. A. baumannii associated nosocomial infection accounts for about 2-3% in the US and about 20-25% in Asia and the Middle East. After listing CRAB as a pathogen of urgent priority, the incidence of CRAB infections is increasing rapidly. Some reports have reported around 50 -70% of isolated A. baumannii to be CRAB in Asian, Latin American, and Middle East regions. The prevalence of CRAB among the isolated A. baumannii in the American region is also around 50%. CRAB is listed as endemic in hospital settings. Since 2011 CRAB has spread dramatically in China and Latin America. During the SARS-CoV-2 pandemic, cases of CRAB infections have risen in hospitals all around the globe.
Identification of Carbapenem-Resistant Acinetobacter baumannii (CRAB)
For identification of CRAB in clinical (or environmental) isolates, the first isolates are identified as A. baumannii using biochemical tests or molecular methods (PCR, gene sequencing, DNA Probe). A biochemical testing algorithm is the most commonly used method.
Biochemical Algorithm For Identification of A. baumannii
- Aerobic, Non-fastidious, Optimum growth at 37°C
- Gram-negative cocco bacilli, Capsulated
- Oxidase –ve, Non-motile
- IMViC = – – – +
- Nitrate and Urease non-reducing
- TSI = R/R, Gas, and H2S –ve
- Glucose and mannitol non-fermentative
- Oxidative utilization of glucose
- Arginine decarboxylase positive
Confirmation of Carbapenem Resistance in A. baumannii (CRAB)
A. Phenotypic Confirmation of CRAB
Phenotypically, CRAB can be confirmed by performing Antimicrobial Sensitivity Test using carbapenems. If the size of the zone of inhibition is less than recommended or in the level of resistance, then we can confirm the isolate to be CRAB.
Zone size interpretative chart for carbapenems against Acinetobacter spp. according to the CLSI is presented below.
| Zone Size (in mm) | Zone Size (in mm) | Zone Size (in mm) | |
| Carbapenem Antibiotics | Sensitive | Intermediate | Resistance |
| Doripenem (DOR 10 mcg) | ≥18 | 15 – 17 | ≤14 |
| Ertapenem (ETP 10 mcg) | Not available | Not available | Not available |
| Imipenem (IMP 10 mcg) | ≥22 | 19 – 21 | ≤18 |
| Meropenem (MRP 10 mcg) | ≥18 | 15 – 17 | ≤14 |
The common methods for phenotypic detection of carbapenemase production in CRAB include:
- Modified Hodge Test
The Modified Hodge Test is a useful, common, and simplest phenotypic method for detecting carbapenemase production. It requires Mueller-Hinton Agar (MHA) and E. coli (ATCC 25922) for testing and sample organisms.
MHA plate is spread with 0.5 McFarland E. coli solution, and a carbapenem disc (10 mcg meropenem or ertapenem) is placed at the center. The test organism is streaked from the edge of the disc to the edge of the plate (up to 4 streaks of the same or different sample for a 10 cm Petri plate).
Following overnight aerobic incubation (16-24 hrs) at 37°C, the plate is examined and reported as:
Positive carbapenemase production: formation of clover leaf–like pattern due to growth of test organism in streaked lines inside the zone of inhibition of E. coli.
Negative carbapenemase production: no clover leaf-like pattern due to no growth of test organism in streaked lines inside the zone of inhibition of E. coli.
However, due to low sensitivity and frequent production of a false positive result by organisms producing ESBLs and AmpC Beta-Lactamase, this method is not recommended nowadays by CLSI.
- Carba NP Test
Carba NP Test is another rapid method of detecting carbapenemase production by monitoring the test organism’s imipenem hydrolyzing capacity. In this method, a test medium containing imipenem and phenol red indicator is inoculated with the test organism and incubated at 37°C for 2 hours. Following incubation, a reduction in pH resulting change in color of the medium from red to yellow (sometimes orange) is considered positive for carbapenemase production. No change in color (retaining red color) indicates no carbapenemase production.
However, it also fails to detect OXA-48-like carbapenemase enzymes.
- Modified Carbapenem Inactivation Method
The Modified Carbapenem Inactivation Method is the most sensitive phenotypic method for carbapenemase detection currently available and in use. For this method, the fresh culture of the test organism is mixed in Tryptic Soy Broth and vortexed to obtain a homogenous suspension. In the suspension, a 10 mcg meropenem disc is inserted, and the suspension is incubated for 2 hours at 37°C. Following the incubation, the disc is picked and placed in the center of an MHA plate pre-inoculated with the suspension of 0.5 McFarland E. coli ATCC 25922. The plate is then aerobically incubated at 37°C for 16 – 24 hours, and the size of the zone of inhibition is measured. If the zone is 15 mm, then the test is positive for carbapenemase production, and if the zone is 19 mm, then the test is negative for carbapenemase production.
B. The use of supplemented CHROMAgar Acinetobacter medium for direct isolation and CRAB identification is also being used but is limited due to cost issues.
C. Molecular Confirmation of CRAB
- PCR is the most widely used tool in laboratories to identify (β-lactamase genes) genes producing carbapenemases and modified porins and efflux pumps.
- Xpert Carba-R molecular test is a common PCR method for detecting carbapenemase production.
- Duplex multiple cross displacement amplification combined with lateral flow biosensor (MCDA-LFB) method is a new and reliable method for quickly identifying CRAB.
- DNA Microarray is another commonly used method.
Prospective Treatment options for Carbapenem-Resistant Acinetobacter baumannii (CRAB) infections
Carbapenems have the broadest antibiotic spectrum and are called “the antibiotic of last resort”, so treating an infection with CRAB is a very task. There is a limited treatment option for CRAB infection. Among these limited ones, sulbactam and polymyxins are the most potent. The Infectious Disease Society of America (IDSA) has released guidelines for the treatment of CRAB, and it includes the following treatment options: (reference: doi: 10.1093/cid/ciab1013.)
- Ampicillin-Sulbactam
A high dose of ampicillin-sulbactam is the most potent treatment option for infections by CRAB. A combination of ampicillin and sulbactam in the ratio of 2:1 is preferred. Sulbactam is a β-lactamase inhibitor and can saturate PBPs1 and 3 when in higher dosage. A dosage of 27 gm of ampicillin-sulbactam is very effective in treating CRAB infections.
Dosage as per ISDA: 3 gm every 4 hours or 9gm every 8 hours or 27 gm continuous infusions over 24 hours
Alternatively, cefoperazone-sulbactam can be administered.
- Polymyxins
Polymyxin A and E are effective against CRAB infections. Polymixin E (Colistin) is used successfully for CRAB-associated pneumonia, meningitis, and bacteremia. Colistin is guided to administer a certain amount, maintaining colistin-plasma concentration to 2 mg/l. Colistin is often recommended to use in combination with other agents like ampicillin-sulbactam.
- Minocycline
Intravenous (IV) minocycline at a dosage of 200 mg every 12 hours is found to be successful in treating CRAB infections. It is often used in combination with colistin, rifampin, or carbapenems.
- Tigecycline
Tigecycline with 200 mg initial IV administration followed by 100 mg every 12 hours is used to treat pulmonary and systemic infection by CRAB. However, resistance is seen in many cases of CRAB infections, so a higher dosage is recommended.
- Eravacycline
Though not used widely for treating CRAB infection, in in-vitro studies, eravacycline has shown potential sensitivity against CRAB. 1 mg/kg/every 12 hours is the estimated dosage.
- Cefiderocol
Cefiderocol has shown sensitivity against CRAB with oxacillinase production. Despite its effectiveness, it has shown lower potential in comparison to polymyxins and sulbactam, so it is rarely used. And when used, it is always recommended to use as part of combination therapy at a dosage of 2 gm every 8 hours infused over 3 hours.
- Fosfomycin
IV fosfomycin as part of combination therapy has shown sensitivity in pneumonia and UTIs caused by CRAB. However, due to the limited supply of IV fosfomycin, it is rarely used.
- Carbapenems
A high dosage of carbapenems in combination with ampicillin-sulbactam and either polymyxin or minocycline is used against CRAB. But, recent studies have questioned the role of carbapenems because a similar result is shown when ampicillin-sulbactam and either polymyxin or minocycline dual therapy is used in place of triple therapy.
- Rifamycin
In-vitro analysis of rifampin in combination with colistin has shown an effect against CRAB. However, limited data, toxic effects, negative drug interaction, and no synergistic effect when used with colistin have limited its use in treating CRAB infections.
- Other Future Prospectives
Several other modes of treatment are under study, like inhalation antibiotics for CRAB-associated pneumonia, Phage therapy (using bacteriophage ØABP-01, Bϕ-C62, and vB_Ab-M-G7) engineered endolysins, gallium nitrate or gallium protoporphyrin IX compounds, probiotics, immunomodulators, herbal extracts, etc.
Prevention and Control Measures from Carbapenem-Resistant Acinetobacter baumannii (CRAB) Infections
- Effective surveillance system in hospital settings and frequent monitoring of microbial diversity in hospitals settings to check for the prevalence of A. baumannii and CRAB in hospitals
- Rigorous environmental cleaning practice in hospitals and patient’s room
- Proper sterilization of medical devices before use
- Sanitization habits in hospital staff and adoption of contact precaution techniques while dealing with potential hosts
- Maintaining a sterile environment in pre- and post-operation wards, operation theater, ICUs, and ventilators
- Antimicrobial therapy stewardship.
Medical Disclaimer
- The information presented on this page is only for academic, study, and general purposes.
- The information presented on this page must not be used for medical advice or diagnosis, or treatment. If you are not feeling well, please consult with your physician or doctor or qualified health care providers.
- Microbe Notes does not guarantee the efficacy or safety of products or treatments described on this page.
- Microbe Notes does not recommend or endorse any specific test, clinical care provider, products, procedures, opinions, services, or other information mentioned on this page.
References
- Nowak P, Paluchowska P. Acinetobacter baumannii: biology and drug resistance – role of carbapenemases. Folia Histochem Cytobiol. 2016;54(2):61-74. doi: 10.5603/FHC.a2016.0009. Epub 2016 Jun 8. PMID: 27270503.
- Bartal C, Rolston KVI, Nesher L. Carbapenem-resistant Acinetobacter baumannii: Colonization, Infection and Current Treatment Options. Infect Dis Ther. 2022 Apr;11(2):683-694. doi: 10.1007/s40121-022-00597-w. Epub 2022 Feb 17. PMID: 35175509; PMCID: PMC8960525.
- Michalopoulos A, Falagas ME. Treatment of Acinetobacter infections. Expert Opin Pharmacother. 2010 Apr;11(5):779-88. doi: 10.1517/14656561003596350. PMID: 20210684.
- Harding CM, Hennon SW, Feldman MF. Uncovering the mechanisms of Acinetobacter baumannii virulence. Nat Rev Microbiol. 2018 Feb;16(2):91-102. doi: 10.1038/nrmicro.2017.148. Epub 2017 Dec 18. PMID: 29249812; PMCID: PMC6571207.
- Mea HJ, Yong PVC, Wong EH. An overview of Acinetobacter baumannii pathogenesis: Motility, adherence and biofilm formation. Microbiol Res. 2021 Jun;247:126722. doi: 10.1016/j.micres.2021.126722. Epub 2021 Feb 4. PMID: 33618061.
- Sabah Jamal, Ahmad Al Atrouni, Rayane Rafei, Fouad Dabboussi, Monzer Hamze, Marwan Osman, Molecular mechanisms of antimicrobial resistance in Acinetobacter baumannii, with a special focus on its epidemiology in Lebanon, Journal of Global Antimicrobial Resistance, Volume 15, 2018, https://doi.org/10.1016/j.jgar.2018.05.022. (https://www.sciencedirect.com/science/article/pii/S2213716518301061)
- Lee CR, Lee JH, Park M, Park KS, Bae IK, Kim YB, Cha CJ, Jeong BC, Lee SH. Biology of Acinetobacter baumannii: Pathogenesis, Antibiotic Resistance Mechanisms, and Prospective Treatment Options. Front Cell Infect Microbiol. 2017 Mar 13;7:55. doi: 10.3389/fcimb.2017.00055. PMID: 28348979; PMCID: PMC5346588.
- Upmanyu K, Haq QMR, Singh R. Factors mediating Acinetobacter baumannii biofilm formation: Opportunities for developing therapeutics. Curr Res Microb Sci. 2022 Mar 28;3:100131. doi: 10.1016/j.crmicr.2022.100131. PMID: 35909621; PMCID: PMC9325880.
- Ramirez MS, Bonomo RA, Tolmasky ME. Carbapenemases: Transforming Acinetobacter baumannii into a Yet More Dangerous Menace. Biomolecules. 2020 May 6;10(5):720. doi: 10.3390/biom10050720. PMID: 32384624; PMCID: PMC7277208.
- Pogue JM, Mann T, Barber KE, Kaye KS. Carbapenem-resistant Acinetobacter baumannii: epidemiology, surveillance and management. Expert Rev Anti Infect Ther. 2013 Apr;11(4):383-93. doi: 10.1586/eri.13.14. PMID: 23566148.
- Abdallah EM, Abdalla RM. Acinetobacter baumannii, a global health-threatening bacterium: a short review. J Mircobiol Exp. 2021;9(6):181-184. DOI: 10.15406/jmen.2021.09.00341
- Acinetobacter baumannii – NICD
- Acinetobacter in Healthcare Settings | HAI | CDC
- Acinetobacter baumannii: Trends in Microbiology (cell.com)
- Textbook of Microbiology and Immunology (2012), 2nd Editions. Subah Chandra Parija. ISBN: 978-81-312-2810-4
- Biswas, Indranil; Rather, Philip N. (2019). [Methods in Molecular Biology] Acinetobacter baumannii Volume 1946 (Methods and Protocols) || . , 10.1007/978-1-4939-9118-1(), –. doi:10.1007/978-1-4939-9118-1
- Abram, Maja & Škrobonja, Ivana & Ambrožić, Damir & repac antić, Davorka & Bubonja-Sonje, Marina. (2018). ESKAPE – bacteria that alert the world. Medicina Fluminensis. 54. 242-253. 10.21860/medflum2018_203547.
- Acinetobacter baumannii: characteristics, morphology, symptoms – science – 2022 (warbletoncouncil.org)
- Acinetobacter: Introduction, Morphology, Pathogenecity, Lab Diagnosis (universe84a.com)
- CHROMagar™ Acinetobacter – Chromagar
- Nicolau, David P (2008). Carbapenems: a potent class of antibiotics. Expert Opinion on Pharmacotherapy, 9(1), 23–37. doi:10.1517/14656566.9.1.23
- Aurilio C, Sansone P, Barbarisi M, Pota V, Giaccari LG, Coppolino F, Barbarisi A, Passavanti MB, Pace MC. Mechanisms of Action of Carbapenem Resistance. Antibiotics (Basel). 2022 Mar 21;11(3):421. doi: 10.3390/antibiotics11030421. PMID: 35326884; PMCID: PMC8944602.
- Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America Guidance on the Treatment of AmpC β-Lactamase-Producing Enterobacterales, Carbapenem-Resistant Acinetobacter baumannii, and Stenotrophomonas maltophilia Infections. Clin Infect Dis. 2022 Jul 6;74(12):2089-2114. doi: 10.1093/cid/ciab1013. PMID: 34864936.
