Interesting Science Videos
Abstract
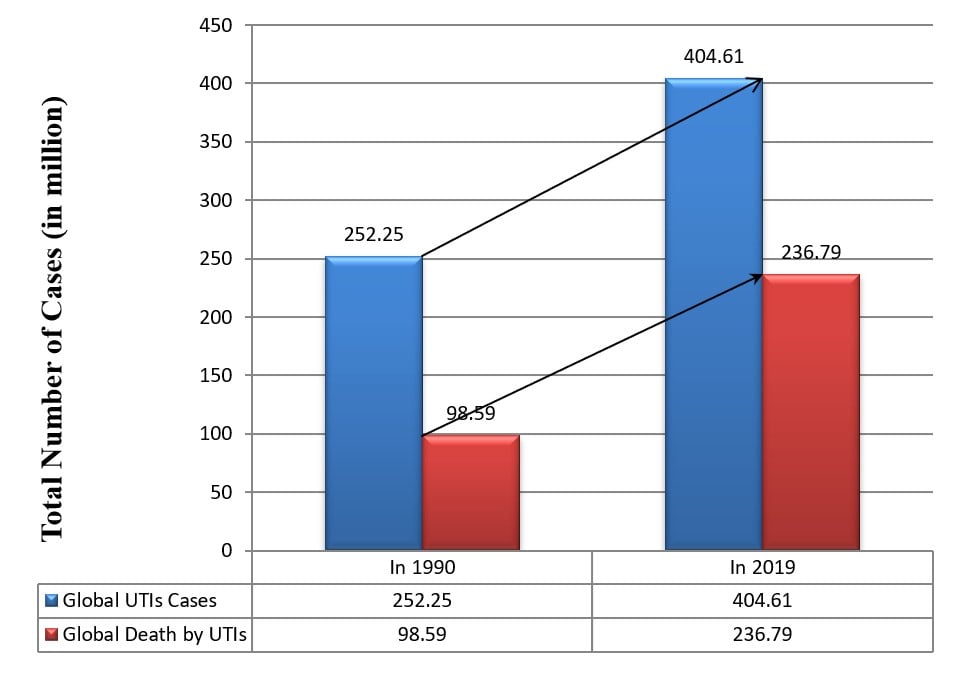
Urinary tract infection (UTI) is an infection of the urinary system. Bacterial UTI is the most prevalent bacterial infection, resulting in more than 400 million cases yearly. There is a substantial increase in UTI cases globally – 252.25 million cases in 1990 while 404.61 million cases in 2019. Based on this data derived from 30-year-long research, it can be estimated that soon prevalence of UTI cases will be more intense and worst, resulting in more case severity and a higher mortality rate. In addition, the development of antimicrobial resistance is worsening the case. Despite of huge burden on global health and the economy, there is no genuine surveillance and case recording system.
Introduction to UTI
Urinary tract infections (UTIs) are among the most prevalent bacterial infections in the world, globally accounting for more than 404 million clinical cases in 2019 (Yang, X. et.al, 2022). After Respiratory Tract Infections (RTIs), UTI account for the most common infection in human populations. UTIs are infections of the urinary system caused by the invasion of pathogens within the urinary tract. It includes infection of the urethra (called urethritis), bladder (called cystitis), kidneys (called pyelonephritis), ureter (called ureteritis), or simply the presence of bacteria in urine (called bacteriuria).
There is heterogeneity in the classification scheme of UTIs. Based on the 2017’s updated German guidelines, UTIs can be categorized as: (Medina, M., 2019)
- Uncomplicated UTIs (where no abnormalities in the urinary system, kidney functioning, and no associated complications are observed),
- Acute Uncomplicated Cystitis (where symptoms associated with lower UTIs like dysuria, urgency in urination, pain above symphysis, and pollakiuria),
- Acute Uncomplicated Pyelonephritis (Upper UTIs with persistent flank pain and tenderness, and fever >100.4°F),
- Asymptomatic Bacteriuria (positive urine culture with significant microbial growth), and
- Recurrent UTIs (with 2 UTIs within 6 months or 3 UTIs within 12 months).
There is heterogeneity in etiology also; new pathogens are emerging, and existing pathogens vary with geographical regions. UTIs are mainly caused by bacteria, bacterial UTIs, like E. coli, Klebsiella, Proteus, Staphylococcus, Enterobacter, Enterococci, Acinetobacter, Serratia, etc. Fungal species, mainly Candida spp. are responsible for fungal UTIs. (Flores-Mireles, A. L., et.al, 2015)
UTI is one serious public health issue – both community-acquired and healthcare-associated infections (HAIs) are common. Nosocomial UTIs, especially those caused by antimicrobial-resistant species, are responsible for the severity of the patient’s condition and increment in mortality. It is estimated that about 50% – 80% of individuals are affected by any form of UTI in their lifetime (Zhao, Fei, et.al, 2020). Females are more frequently infected with UTIs; about 60% of females will experience UTIs at least once in a lifetime (Medina, M., 2019).
Although UTIs are among the most common infections and globally billions of dollars are invested in treating UTIs, there is no systematic surveillance system to track the number of incidences of UTIs. In this article, we tried to summarize the global burden of UTIs with a comprehensive estimation of reported cases, etiology, and risk factors.
Objectives
- To study the global trend of UTI incidences.
- To study the etiology of UTIs and their prevalence rate
- To study the prevalence of UTI cases in different ages and sex
Methods and Methodologies
Search Strategy
Data are collected from research articles, news portals, and different trustable sites available on the internet. Google, Pub Med, Google Scholar, Research Gate, Scopus, Lancet Microbiology, and Research Square were used as search tools to search for articles published from 2000 to 2022.
The keywords used for searching articles are: “Urinary Tract Infections”, “Epidemiology of UTIs”, “Prevalence of UTI”, “Incidence of Urinary Tract Infections”, “Global Burden of UTI”, “Etiology of UTI”, “Antimicrobial resistance in UTI”, “Review on Urinary Tract Infections”, and “Recent UTI Articles”.
Selection Criteria
The articles meeting the following criteria were included in the study:
- Original research articles or review articles on epidemiology, prevalence, and incidences of UTIs
- Articles on UTIs containing study reports from 2000 and onwards
- Articles that include studies on UTIs caused by overall etiological agents rather than a specific one.
Results
1. Etiology of the UTIs
UTIs are either bacterial or fungal. Bacterial UTIs are the most common types of UTIs. Escherichia coli is the predominant uropathogen causing UTIs, community-acquired and nosocomial, as well as complicated and uncomplicated UTIs. E. coli alone is responsible for about 80% of UTIs globally.
The order of causative agents based on their prevalence differs in the case of complicated UTIs (cUTIs) and uncomplicated UTIs (ucUTIs). The etiologies of UTIs also differ with underlying factors like age, sex, health condition, catheterization, geography, environment, etc.
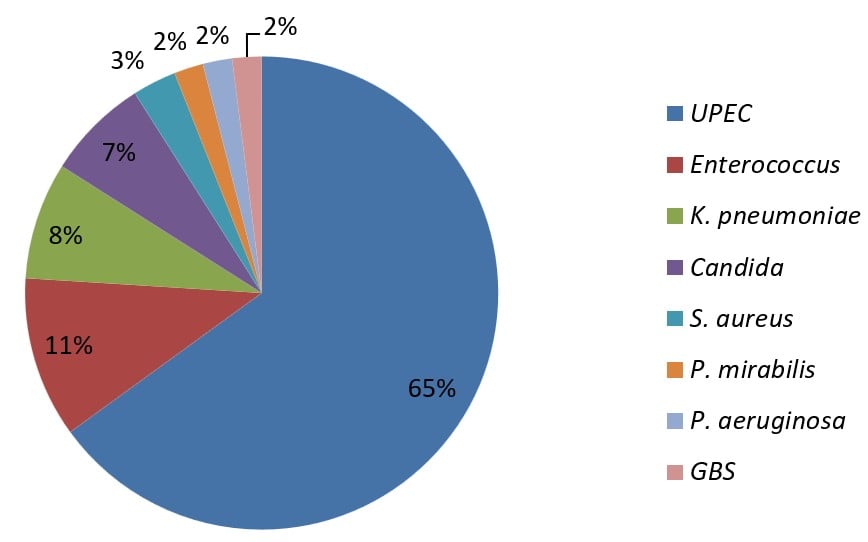
a. Complicated UTIs;
Uropathogens involved in complicated UTIs can be ordered, based on their prevalence, as E. coli (Uropathogenic E. coli (UPEC)) 65%, Enterococcus spp. 11%, Klebsiella pneumoniae 8%, Candida spp. 7%, Staphylococcus aureus 3%, Proteus mirabilis 2%, Pseudomonas aeruginosa 2%, and Group B Streptococcus spp. (GBS) 2%. (Flores-Mireles, A. L, et.al, 2015)
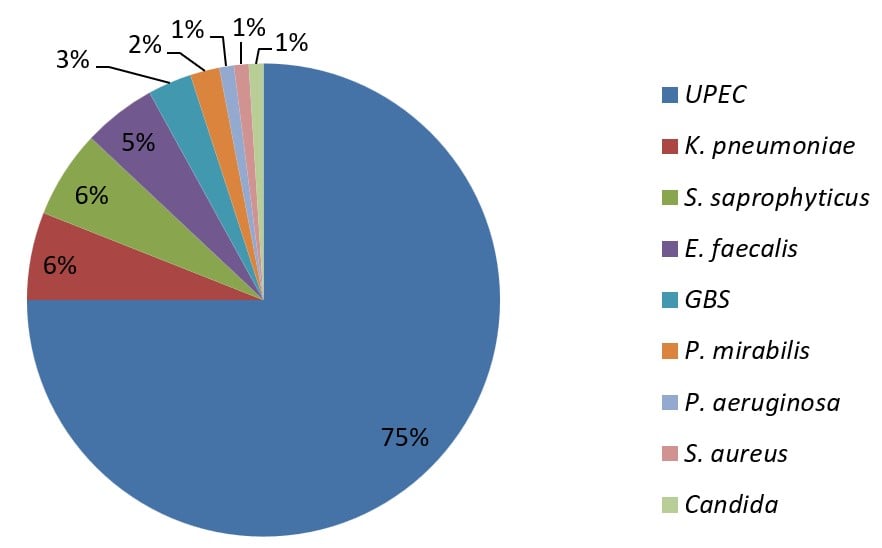
b. Uncomplicated UTIs;
Uropathogens involved in complicated UTIs can be ordered, based on their prevalence, as UPEC 75%, Klebsiella pneumoniae 6%, Staphylococcus saprophyticus 6%, Enterococcus faecalis 5%, GBS 3%, Proteus mirabilis 2%, Pseudomonas aeruginosa 1%, Staphylococcus aureus 1%, and Candida spp. 1%. (Flores-Mireles, A. L, et.al, 2015)
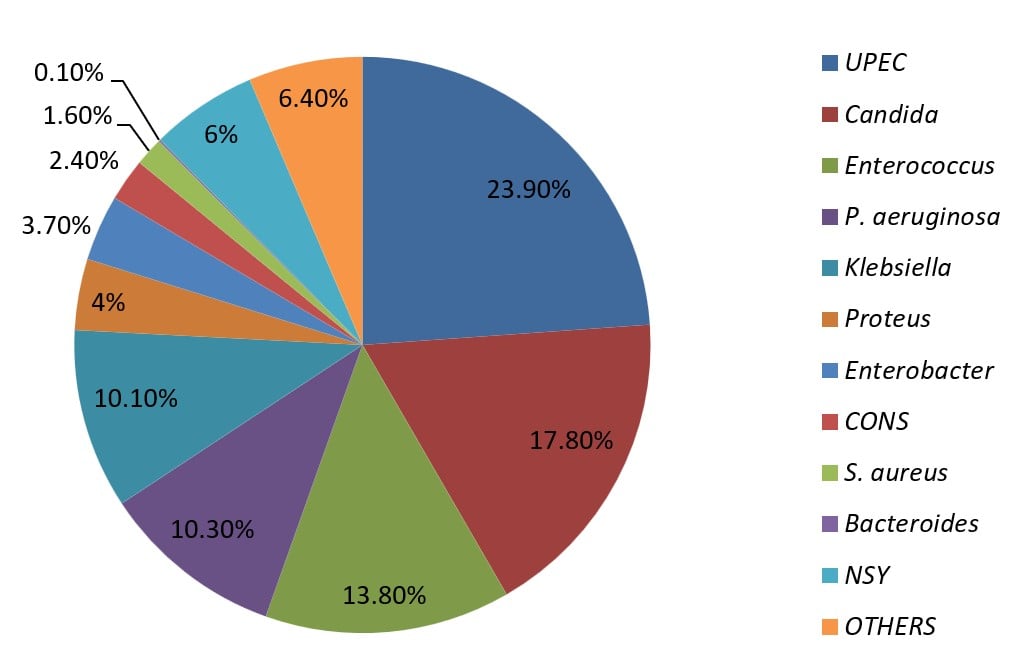
c. Catheter-Associated UTIs (CAUTI);
Uropathogens associated with CAUTI are different than in un-catheterized victims of UTIs. The order of prevalence of causatives is UPEC 23.9%, Candida spp. 17.8%, Enterococcus spp. 13.8%, Pseudomonas aeruginosa 10.3%, Klebsiella spp. 10.1%, Proteus spp. 4%, Enterobacter spp. 3.7%, Coagulase negative Staphylococcus (CONS) 2.4%, Staphylococcus aureus 1.6%, Bacteroides spp. 0.1%, not specified yeasts (NSY) 6%, and OTHERS 6.4%. (Flores-Mireles, A., et.al, 2019) OTHERS include opportunistic pathogens like Acinetobacter baumannii and other Acinetobacter spp., Clostridium difficile, Stenotrophomonas maltophilia, Citrobacter spp., Salmonella spp., Aeromonas spp., Serratia spp., Neisseria spp., Providencia spp., Veillonella spp., Corynebacterium spp., Lactobacillus spp., Aerococcus spp., Actinobaculum spp., Gardnerella spp., Propionibacterium spp., Burkholderia sp., Ureaplasma spp., Mycoplasma spp., etc.
2. Global Trend of the UTIs
Approximately 252.25 million UTI cases were reported in 1990 globally, whereas the cases were found to rise to about 404.61 million in 2019 globally (Yang, X. et.al, 2022). UTI cases increased by 60.40% from 1990 to 2019.
The estimated death from UTIs was 98.59 million (89.03 million to 106.32 million) in 1990. The death toll also increased to about 236.79 million (198.4 million to 259.03 million) in 2019.
3. Incidences of UTIs and Age Groups
The prevalence of UTIs varies accordingly to the age group due to anatomical and physiological changes in the body, sexual activity, immunity, hygiene, and other lifestyle changes.
The UTI cases are mainly concentrated in the age group of 25 to 34 years and 0 to 14 years (Zhu, C. et.al, 2021). UTI incidence usually increases with age. However, higher prevalence is seen in the age group of 20 – 40 years. Uncomplicated UTI cases occur at peak rate during the years of maximum sexual activity i.e., 20 to 40 years (Medina M. et.al, 2019) (Tomer, V.K. et.al 2021).
Complicated UTIs are concentrated in elderly people 65 years and above (Rowe, T. A, et.al, 2013)(Sabih, A. et.al, 2022).
4. Incidences of UTIs and Gender
UTIs are more frequent in females than in males. It is estimated that females are about 30 times more prone to UTIs than males. The higher incidence of UTIs in females is mainly because of the shorter urethra in females (about 3 – 6 times shorter than males’), shorter anogenital distance, menstruation cycle, penetrative sexual intercourse, pregnancy, moist (mucosal) lining of the urethral meatus, and types of contraceptives with the higher potentiality to contaminate and disseminate pathogens.
Discussion
There is no systematic approach for recording UTI cases in every country. Due to this, no accurate data is available to analyze the global trend of UTIs. The data presented above is based on research done by Zhu, C., et.al 2021 on epidemiological trends of UTIs in 203 countries from 1990 to 2019. It is found that the highest numbers of UTI cases are reported in the South East Asian region. This may be associated with environmental factors and socioeconomic status.
UTI cases are concentrated in the age group from 25 to 34. Activeness in sexual activities, body physiology, physical work, and working environment might have caused maximum UTI incidences in this age group.
Similarly, the prevalence of UTIs is higher in females than in males with a higher recurrence rate. Female anatomy (shorter urethra), menstruation, and pregnancy are the major cause of this higher prevalence rate (Guglietta, Antonio 2017).
Conclusion and Future Perspective
The substantial annual increasing trend of UTI cases implies that the estimated number of cases for 2022 is no less than 404 million globally. In addition to the number of cases, the emergence of antimicrobial resistance in these uropathogens is fueling the case severity as well as surging the UTI-associated mortality; hence making the situation more worst. New uropathogens such as Aerococcus spp., Stenotrophomonas maltophilia, Corynebacterium urealyticum, Actinotignum schaalii, H. influenzae, Trueperella spp., etc. are also emerging like (Gupta K. 2003). This rapid development of antibiotic resistance in urinary tract pathogens (Wang R. et.al, 2021) and emerging new pathogens is likely to worsen the scenario of UTIs in the future.
To stop and reduce the increasing trend of UTI cases, several things are to be sorted out quickly. Primarily, the prevention of UTIs should be given priority. Secondly, early diagnosis and proper treatment to prevent transmission and development of resistance in uropathogens are very important. Thirdly, prevention from the emergence of drug resistance in uropathogens and the development of new effective treatment options for resistant pathogens should be given priority.
A system of promptly recording UTI cases must be adopted in every country so that accurate data can be obtained to formulate proper policies and plans to mitigate the global burden of UTIs.
References
- Yang, X., Chen, H., Zheng, Y., Qu, S., Wang, H., & Yi, F. (2022). Disease burden and long-term trends of urinary tract infections: A worldwide report. Frontiers in Public Health, 10. https://doi.org/10.3389/fpubh.2022.888205
- Medina, M., & Castillo-Pino, E. (2019). An introduction to the epidemiology and burden of urinary tract infections. Therapeutic Advances in Urology, 11. https://doi.org/10.1177/1756287219832172
- Zhao, Fei; Yang, Huanxin; Bi, Dezhong; Khaledi, Azad; Qiao, Mingqi (2020). A systematic review and meta-analysis of antibiotic resistance patterns, and the correlation between biofilm formation with virulence factors in uropathogenic E. coli isolated from urinary tract infections. Microbial Pathogenesis, 144(), 104196–. doi:10.1016/j.micpath.2020.104196
- Paudel, S., John, P. P., Poorbaghi, S. L., Randis, T. M., & Kulkarni, R. (2022). Systematic Review of Literature Examining Bacterial Urinary Tract Infections in Diabetes. Journal of Diabetes Research, 2022. https://doi.org/10.1155/2022/3588297
- Flores-Mireles, A. L., Walker, J. N., Caparon, M., & Hultgren, S. J. (2015). Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nature reviews. Microbiology, 13(5), 269. https://doi.org/10.1038/nrmicro3432
- Flores-Mireles, A., Hreha, T. N., & Hunstad, D. A. (2019). Pathophysiology, Treatment, and Prevention of Catheter-Associated Urinary Tract Infection. Topics in Spinal Cord Injury Rehabilitation, 25(3), 228-240. https://doi.org/10.1310/sci2503-228
- Ronald, Allan (2003). The etiology of urinary tract infection: Traditional and emerging pathogens. Disease-a-Month, 49(2), 71–82. doi:10.1067/mda.2003.8
- Foxman, Betsy (2014). Urinary Tract Infection Syndromes. Infectious Disease Clinics of North America, 28(1), 1–13. doi:10.1016/j.idc.2013.09.003
- Bono MJ, Leslie SW, Reygaert WC. Urinary Tract Infection. [Updated 2022 Jun 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470195/
- Zhu, C., Wang, DQ., Zi, H. et al. Epidemiological trends of urinary tract infections, urolithiasis and benign prostatic hyperplasia in 203 countries and territories from 1990 to 2019. Military Med Res 8, 64 (2021). https://doi.org/10.1186/s40779-021-00359-8
- Le Brun C, Robert S, Bruyere F, Lanotte P. Mise au point : les uropathogènes émergents [Emerging uropathogens: Point for urologists and biologists]. Prog Urol. 2015 Jun;25(7):363-9. French. doi: 10.1016/j.purol.2015.01.021. Epub 2015 Feb 27. PMID: 25726694.
- Wang R, LaSala C. Role of antibiotic resistance in urinary tract infection management: a cost-effectiveness analysis. Am J Obstet Gynecol. 2021 Nov;225(5):550.e1-550.e10. doi: 10.1016/j.ajog.2021.08.014. Epub 2021 Aug 18. PMID: 34418350.
- Gupta K. Emerging antibiotic resistance in urinary tract pathogens. Infect Dis Clin North Am. 2003 Jun;17(2):243-59. doi: 10.1016/s0891-5520(03)00006-0. PMID: 12848469.
- Guglietta, Antonio (2017). Recurrent urinary tract infections in women: risk factors, etiology, pathogenesis and prophylaxis. Future Microbiology, 12(3), 239–246. doi:10.2217/fmb-2016-0145
- Öztürk, Recep; Murt, Ahmet (2020). Epidemiology of urological infections: a global burden. World Journal of Urology, (), –. doi:10.1007/s00345-019-03071-4
- Podkovik, S., Toor, H., Gattupalli, M., Kashyap, S., Brazdzionis, J., Patchana, T., Bonda, S., Wong, S., Kang, C., Mo, K., Wacker, M. R., Miulli, D. E., & Wang, S. (2019). Prevalence of Catheter-Associated Urinary Tract Infections in Neurosurgical Intensive Care Patients – The Overdiagnosis of Urinary Tract Infections. Cureus, 11(8). https://doi.org/10.7759/cureus.5494
- Tandogdu, Zafer; Wagenlehner, Florian M.E. (2016). Global epidemiology of urinary tract infections. Current Opinion in Infectious Diseases, 29(1), 73–79. doi:10.1097/qco.0000000000000228
- Bono MJ, Leslie SW, Reygaert WC, et al. Urinary Tract Infection (Nursing) [Updated 2022 Jun 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK568701/
- Shafrin, J., Marijam, A., Joshi, A.V. et al. Economic burden of antibiotic-not-susceptible isolates in uncomplicated urinary tract infection: Analysis of a US integrated delivery network database. Antimicrob Resist Infect Control 11, 84 (2022). https://doi.org/10.1186/s13756-022-01121-y
- Li X, Fan H, Zi H, Hu H, Li B, Huang J, Luo P, Zeng X. Global and Regional Burden of Bacterial Antimicrobial Resistance in Urinary Tract Infections in 2019. Journal of Clinical Medicine. 2022; 11(10):2817. https://doi.org/10.3390/jcm11102817
- Rozwadowski, M., & Gawel, D. (2022). Molecular Factors and Mechanisms Driving Multidrug Resistance in Uropathogenic Escherichia coli—An Update. Genes, 13(8). https://doi.org/10.3390/genes13081397
- Papanikolopoulou, A., Maltezou, H. C., Stoupis, A., Kalimeri, D., Pavli, A., Boufidou, F., Karalexi, M., Pantazis, N., Pantos, C., Tountas, Y., Koumaki, V., Kantzanou, M., & Tsakris, A. (2022). Catheter-Associated Urinary Tract Infections, Bacteremia, and Infection Control Interventions in a Hospital: A Six-Year Time-Series Study. Journal of Clinical Medicine, 11(18). https://doi.org/10.3390/jcm11185418
- Magliano, E., Grazioli, V., Deflorio, L., Leuci, A. I., Mattina, R., Romano, P., & Cocuzza, C. E. (2012). Gender and Age-Dependent Etiology of Community-Acquired Urinary Tract Infections. The Scientific World Journal, 2012. https://doi.org/10.1100/2012/349597
- Medina, M., & Castillo-Pino, E. (2019). An introduction to the epidemiology and burden of urinary tract infections. Therapeutic Advances in Urology. https://doi.org/10.1177/1756287219832172
- Tomer, V.K., Dhama, V., Kaushik, S., Kumar, M., Singh, B., Panwar, R., & Singh, R. (2021) Prevalence of UTI in Different Age Groups and AntimicrobialSusceptibility Pattern of Isolates. International Journal of Medical and Allied Health Sciences.
- Rowe, T. A., & Juthani-Mehta, M. (2013). Urinary tract infection in older adults. Aging health, 9(5). https://doi.org/10.2217/ahe.13.38
- Sabih A, Leslie SW. Complicated Urinary Tract Infections. [Updated 2022 May 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436013/
- 7 Reasons Why Women Get More UTIs Than Men | Virginia Physicians for Women (vpfw.com)
- Urinary tract infections | Office on Women’s Health (womenshealth.gov)
- Your Ultimate UTI Prevention Guide: Everything You Need To Know To STOP Your UTIs (Get Yours Now) (dmanna.com)
- Urinary tract infection (UTI) – Symptoms and causes – Mayo Clinic
- Urinary Tract Infections: Statistics And Facts (dmanna.com)
