Interesting Science Videos
What is Pseudomonas aeruginosa?
Pseudomonas aeruginosa is an aerobic microorganism that is a motile, Gram-negative rod-shaped bacteria distributed throughout different habitats in the world.
- It has an absolute aerobic metabolism and thus, gives a positive oxidase reaction.
- P. aeruginosa is the unique species of this genus which is often used as the type species for the genus.
- It is a unique species of this genus that has not only all the general properties of the members of the genus but also some relatively uncommon properties.
- P. aeruginosa is one of the fluorescent species as it produces pigments that produce fluorescence under UV radiation.
- Lately, P. aeruginosa has been extensively studied and considered medically important due to its widespread distribution, resistance against many antibacterial compounds, and a large number of pathogenicity factors.
- The species name ‘aeruginosa‘ is derived from the Latin term ‘aeruginosa’ meaning full of copper rust or verdigris (green) indicating its fluorescence.
- It has previously named Bacterium aeruginosum by Schroeter in 1872 but was later renamed Pseudomonas aeruginosa.
- The bacterium has extreme medical importance as it is one of the leading causes of community-acquired infections like hospital-acquired pneumonia, urinary tract infections, among others.
- It is a ubiquitous gramma-proteobacterium that is found in many different habitats ranging from soil and aquatic habitats to the animate surfaces of plants, animals, and human beings.
- P. aeruginosa is an opportunistic pathogen that exists in the body of living beings as a part of the normal flora but might induce infections under immunocompromised situations.
- However, the bacterium also has several industrial applications where it is cultivated for the production of primary and secondary metabolites. These are also used as agents of biosurfactants for environmental cleanup, restoration, and remediation.
- One of the challenges associated with the treatment of P. aeruginosa is its increasing resistance to multiple antibiotics which makes them almost intractable once inside the body of the host.

Image Source: Kenneth Todar, HansN (Wikimedia) and HansN (Wikimedia).
Classification of Pseudomonas aeruginosa
- Pseudomonas aeruginosa belong to the order Pseudomonadales based on the phylogenetic analysis of 16S rRNA sequences, which further contains two families; Pseudomonasaceae and Moraxellaceae.
- The species of this genus are proteobacteria belonging to the sub-group, gamma-proteobacteria, which is the most diverse group of proteobacteria.
- Based on the rRNA/DNA hybridization studies, Pseudomonas can be divided into rRNA homology groups, each of which is represented by at least a separate genus.
- Initially, the name ‘Pseudomonas‘ was reserved for rRNA group I, consisting of P. aeruginosa.
- The approximate number of species belonging to the genus Pseudomonas is 65 even though it has been speculated that some of the non-pathogenic species of Pseudomonas are not included in that number.
- One of the important classifications of Pseudomonas is based on the production of pigments and fluorescence. P. aeruginosa belongs to the fluorescent group of Pseudomonas species.
- P. aeruginosa is differentiated from other fluorescent species by the presence of a polar flagellum.
The following is the taxonomical classification of P. aeruginosa:
| Domain | Bacteria |
| Phylum | Proteobacteria |
| Class | Gammaproteobacteria |
| Order | Pseudomonadales |
| Family | Pseudomonadaceae |
| Genus | Pseudomonas |
| Species | P. aeruginosa |
Habitat of Pseudomonas aeruginosa
- Pseudomonas aeruginosa is ubiquitous with a wide range of ecological distribution ranging from natural habitats as well as clinical settings.
- In nature, the organism is commonly found in soil and aquatic environments where it exists in a close association with Bacillus.
- P. aeruginosa comprises an essential part of the rhizospheric group of organisms in different plants and soil samples.
- These are also occasionally found in natural and processed foods, which might even act as a source of infections in some cases.
- P. aeruginosa is a part of the normal flora of the human body where it colonizes areas like the respiratory tract, skin, and digestive system.
- As a part of the normal flora, these are essential for the production of primary and secondary metabolites required for the host.
- However, these are opportunistic pathogens that might result in mild to severe infections if they reach sterile sites of the body.
- The ability of P. aeruginosa to colonize animate surfaces as well as natural habitats is due to its versatile metabolic activities.
- Besides, the capacity of this organism to react to environmental changes and to exchange their genetic material makes them important members of the natural microbial communities.
Morphology of Pseudomonas aeruginosa
- The cells of P. aeruginosa are rod-shaped with an average size of 0.5 to 0.8 µm in width and 1.5 to 3.0 µm in length.
- The cells are Gram-negative that often occur as single cells or in pairs. The cells produce pigments that are water-soluble and thus, diffuse through the media.
- All strains of P. aeruginosa are motile with a single flagellum inserted at the tip of the cell. The flagella can be either polar or subpolar in some strains.
- The flagella yield heat-labile antigens (H antigens) acting as a virulence factor in pathogenic strains.
- Besides flagella, polar fimbriae or pili are also found in some strains of P. aeruginosa. These pili are usually 6 nm wide and act as a receptor for various phages and are even retractile.
- The cell envelope of P. aeruginosa is similar to other Gram-negative species, consisting of three distinct layers; outer membrane, inner cytoplasmic membrane, and the peptidoglycan layer.
- The cell membrane of the bacteria has a lipid bilayer that undergoes rapid changes to adjust its fluidity to the changes in the environment.
- The outer membrane, however, is asymmetrically composed of a special lipopolysaccharide providing less fluidity.
- Different serologic types of P. aeruginosa have been distinguished based on the evaluations of O-specific antigens.
- The organisms might appear pigmented as these are capable of producing about six different types of pigments. Among these, the phenazine blue pigment is the most commonly observed.
Cultural Characteristics of Pseudomonas aeruginosa
- The growth of P. aeruginosa in solid agar media can occur between the temperature of 4°C and 44°C; however, the growth at the higher temperature is more prominent.
- It has a simple nutritional requirement and can grow in media containing acetate as a source of carbon and ammonium sulfate as the source of nitrogen.
- The colonies produced by P. aeruginosa are usually of two types; (1) large and smooth colonies with flat edges and elevated centers resulting in fried-egg appearance, (2) small, rough and convex type.
- The organisms isolated from clinical materials form large types of colonies, whereas those from natural sources form a small types of colonies.
- The large colonies might have silver-grey metallic shining patches at the edges.
- A third mucoid type of colony is also observed in isolates from respiratory and urinary tract infections.
- P. aeruginosa colonies on agar media have a tendency to form localized swarming from the edge of the colony. Besides, the colonies produce green and fluorescing pigments.
- Another important feature of these colonies is a fruity odor and the occurrence of metallic patches.
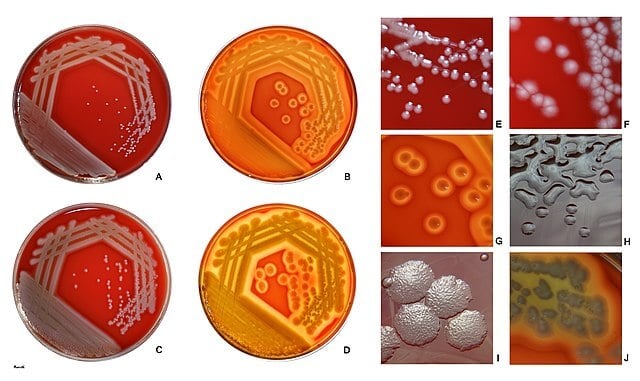
Figure: Pseudomonas aeruginosa growing on sheep blood agar at 37 °C after 24 h (A, C, E, F) and 48 h (B, D, G, H, I, J). P. aeruginosa strains are frequently haemolytic (B, D, G, J; reflected + transmitted light). This species gives rise to a variety of colony types. Most of the colonies are smooth, but varying grades of roughness may occur. Figure I shows an image of colonies with a “beaten-copper“ surface and slightly irregular edge. Capsulated strains of P. aeruginosa, usually isolated from patients with pneumonia, produce large, mucoid colonies (Fig. H). On routine blood agar, the typical P. aeruginosa colony is pigmented (gray/gray-white with a yellowish tint through green to red or brown). Pigment production is usually better visible and more profound on transparent media (e.g., Mueller-Hinton agar). Image Source: HansN (Wikimedia).
The following are some cultural characteristics of P. aeruginosa on different culture media:
P. aeruginosa on Nutrient Agar
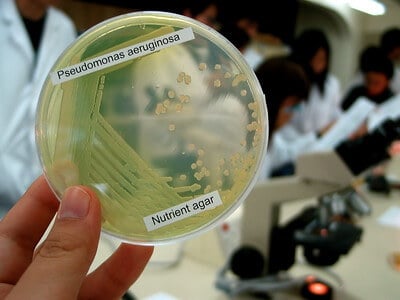
Figure: Pseudomonas aeruginosa on Nutrient Agar. Image Source: Denise Chan.
- P. aeruginosa forms large opaque and flat colonies with irregular margins and fruity or earthy odor.
- The colonies appear pigmented, but the color depends on the type of pigment produces. Usually, on NA, green-colored colonies can be seen due to the production of Pyoverdin pigment.
P. aeruginosa on Cetrimide Agar
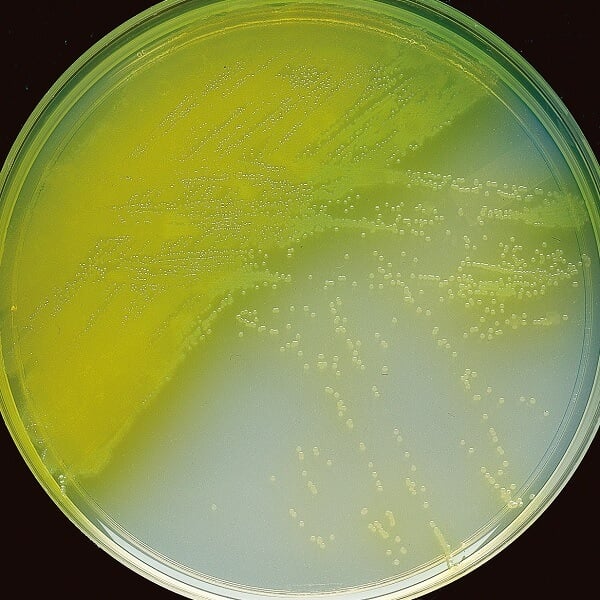
Figure: P. aeruginosa on Cetrimide Agar. Image Source: BD.
- The appearance of yellow-green to blue-colored colonies on cetrimide agar indicates the presence of P. aeruginosa.
- The colonies are medium-sized with irregular margins. The visual examination of the plates is performed by using ultraviolet light to detect the presence of fluorescein.
P. aeruginosa on MacConkey Agar
- P. aeruginosa forms round, flat, and colorless colonies on the MacConkey agar indicating that the organism is a lactose non-fermenter.
- Like in the case of Cetrimide agar, the colonies on MacConkey agar are also observed under ultraviolet to detect the presence of fluorescence.
P. aeruginosa on Blood Agar
- P. aeruginosa produces mucoid-type colonies with a typical metallic sheen.
- β-hemolysis is observed on Blood Agar represented by the clear zone around the colonies.
Biochemical Characteristics of Pseudomonas aeruginosa
The biochemical characteristics of P. aeruginosa can be tabulated as follows:
| S.N | Biochemical Characteristics | P. aeruginosa |
| 1. | Capsule | Non-Capsulated |
| 2. | Shape | Rod |
| 3. | Gram Staining | Gram-Negative |
| 4. | Catalase | Positive (+) |
| 5. | Oxidase | Positive (+) |
| 6. | Citrate | Positive (+) |
| 7. | Methyl Red (MR) | Negative (-) |
| 8. | Voges Proskauer (VR) | Negative (-) |
| 9. | OF (Oxidative-Fermentative) | Oxidative |
| 10. | Coagulase | Negative (-) |
| 11. | DNase | Negative (-) |
| 12. | Urease | Negative (-) |
| 13. | Gas | Negative (-) |
| 14. | H2S | Negative (-) |
| 15. | Hemolysis | β-hemolytic |
| 16. | Motility | Motile with single flagella |
| 17. | Nitrate Reduction | Positive (+) |
| 18. | Gelatin Hydrolysis | Positive (+) |
| 19. | Pigment Production | Positive (+) (Yellow-green/ Blue) |
| 20. | Indole | Negative (-) |
| 21. | TSIA (Triple Sugar Iron Agar) | Alkali/Alkali (Red/ Red) |
| 22. | Spore | Non-sporing |
| 23. | Cetrimide Test | Positive (+) |
Fermentation
| S.N | Substrate | P. aeruginosa |
| 1. | Adonitol | Negative (-) |
| 2. | Arabinose | Negative (-) |
| 3. | Cellobiose | Negative (-) |
| 4. | Dulcitol | Negative (-) |
| 5. | Fructose | Positive (+) |
| 6. | Galactose | Negative (-) |
| 7. | Glucose | Positive (+) |
| 8. | Glycerol | Positive (+) |
| 9. | Glycogen | Negative (-) |
| 10. | Hippurate | Negative (-) |
| 11. | Inulin | Negative (-) |
| 12. | Inositol | Negative (-) |
| 13. | Lactose | Negative (-) |
| 14. | Malonate | Positive (+) |
| 15. | Maltose | Positive (+) |
| 16. | Mannitol | Negative (-) |
| 17. | Mannose | Negative (-) |
| 18. | Pyruvate | Negative (-) |
| 19. | Raffinose | Negative (-) |
| 20. | Rhamnose | Negative (-) |
| 21. | Ribose | Positive (+) |
| 22. | Salicin | Positive (+) |
| 23. | Sorbitol | Negative (-) |
| 24. | Starch | Negative (-) |
| 25. | Sucrose | Negative (-) |
| 26. | Trehalose | Negative (-) |
| 27 | Xylose | Negative (-) |
Enzymatic Reactions
| S.N | Enzymes | P. aeruginosa |
| 1. | Acetoin | Negative (-) |
| 2. | Acetate Utilization | Positive (+) |
| 3. | Arginine Dehydrolase | Positive (+) |
| 4. | Esculin Hydrolysis | Negative (-) |
| 5. | Lecithinase | Negative (-) |
| 6. | Lipase | Positive (+) |
| 7. | Lysine | Negative (-) |
| 8. | Ornithine Decarboxylase | Negative (-) |
| 9. | Phenylalanine Deaminase | Negative (-) |
Virulence Factors of Pseudomonas aeruginosa
- Pseudomonas aeruginosa is an opportunistic pathogen that is associated with various mild and severe nosocomial infections in immunocompromised people.
- The entry, colonization, and infection by P. aeruginosa depend on a number of factors; termed virulence factors that assist the survival of the organisms and evasion of host defense.
- Such virulence factors in P. aeruginosa are classified into different groups based on their involvement during infection.
- The three major types of virulence factors in P. aeruginosa include; factors involved in attachment and motility, factors involved in colonization, and factors involved in chronic infection.
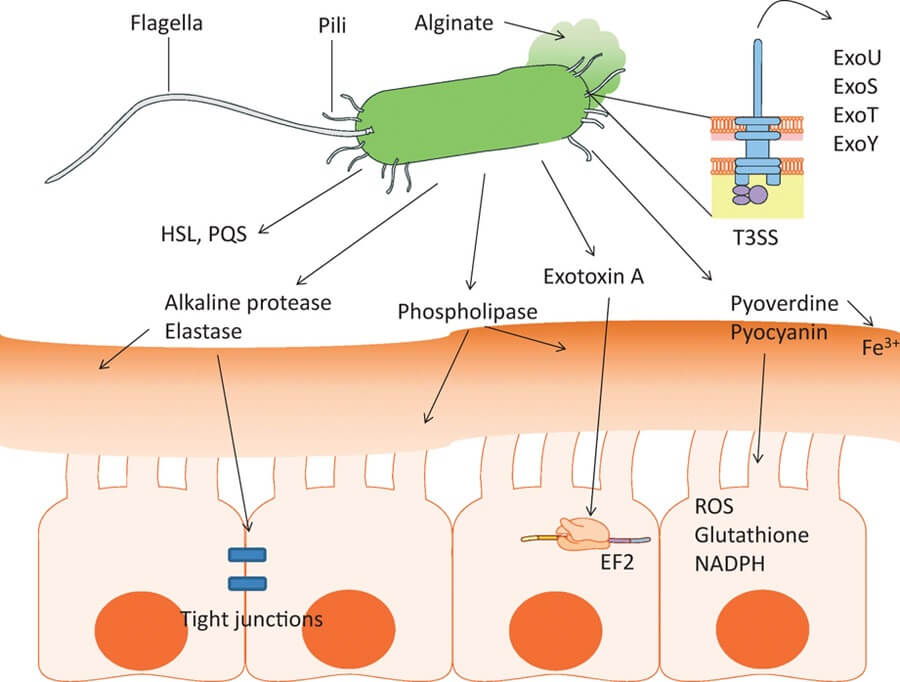
Figure: A multitude of virulence factors are produced by Pseudomonas aeruginosa. Image Source: https://doi.org/10.1111/2049-632X.12033
Factors involved in entry and motility
Flagella
- All P. aeruginosa cells contain a single polar flagellum which results in the swimming type motility of the organism.
- The flagellum is activated by a motor present at the base which drives the filament acting like a helix.
- The flagellum assists the attachment of bacteria to cells of the respiratory tract, which enables them to move through the respiratory tract.
- The flagellum induces an inflammatory reaction by interacting with the Toll-like receptors on the cells, resulting in the release of factors like IL-8, IL-6, and mucin.
Pili
- Type IV pili are the main adhesin of P. aeruginosa, which enables the attachment of bacteria to epithelial cells.
- These structures interact with the glycosylated regions of the glycosphingolipids GM1 and GM2 of the epithelial cells.
- Fimbriae-type pili are also known to induce attachment of the bacterium to the epithelial cells.
- These pili assembled in the chaperone or cup shape which supports the adhesion to abiotic surfaces during the formation of biofilm.
Lipopolysaccharides (LPS)
- The outer membrane of the bacteria is composed of lipopolysaccharide, which prevents the lysis of bacteria and induces endotoxic activity.
- The lipopolysaccharide also stimulates an inflammatory response by interacting with the host tissues.
- The lipopolysaccharide consists of three distinct parts;
- lipid A (endotoxin) which causes excessive stimulation of the immune system, resulting in septic shock.
- The oligosaccharide
- The O-antigen, which prevents lysis by the host serum.
Factors involved in host colonization
Exotoxin A
- Exotoxin A in P. aeruginosa is the most important protein compound produced by bacteria.
- The toxin is secreted as an inactive pre-toxin consisting of two domains; domain A and domain B.
- The domain B of the toxin interacts with the receptor present on the surface of the host cell and induces the termination of protein synthesis.
- Destruction of protein synthesis results in target necrosis of cells.
Elastase
- Elastase is a zinc metalloprotease that has proteolytic activity against the protein elastin.
- In P. aeruginosa, the elastase activity is mediated by two enzymes; Las A and LasB. Las A elastase is a serine protease that acts in synergy with LasB, thus increasing the power of degradation.
- These enzymes have activity against other proteins like IgA and IgG of complement components.
- These enzymes also attack cytokines like γ-interferon and TNF.
Pigments
- P. aeruginosa produces a number of pigments like pyocyanin and pyoverdin.
- Pyocyanin suppresses the immune response of the cell and induces apoptosis of neutrophils. Pyoverdin also acts as a regulator of the secretion of certain virulence factors like exotoxin A.
- These pigments also induce inflammation by inducing the production of IL-8.
- It has also been studied that these pigments inactivate vacuolar ATPase and mitochondrial transport.
Enzymes
- Enzymes like alkaline protease and protease IV are also involved in the pathogenesis of infections caused by P. aeruginosa.
- Alkaline proteases break down fibrin allowing the colonization of tissues by the bacteria.
Factors involved in chronic infections
a. Acquisition of Iron
- Iron is an important mineral for the growth and development of bacteria like P. aeruginosa.
- The acquisition of iron by P. aeruginosa is an essential factor to prevent the loss of bacteria during infections.
- Different factors like chelating agents, iron-laden pyoverdin, and exotoxin A are essential for the purpose.
b. Alginates and Biofilm formation
- Biofilm formation is a common virulence in many bacteria-inducing nosocomial infections.
- The biofilm consists of microcolonies embedded in an exopolysaccharide matrix.
- The biofilm is a durable structure that protects the organisms from the host’s defense mechanism, hinders the penetration of antibiotic agents, and increases resistance to phagocytosis and antibodies.
Pathogenesis of Pseudomonas aeruginosa
The pathogenesis of infections caused by P. aeruginosa is mediated by different virulence factors that facilitate the entry colonization and invasion of host tissue. P. aeruginosa is unique in its ability to cause severe invasive infections while evading the immune system defenses, resulting in persistent infections. During the course of infection, subsequent tissue damage, invasion, and dissemination of P. aeruginosa are attributed to such virulence factors. The pathogenesis of infections caused by P. aeruginosa follows a particular path, ultimately leading to persistent invasive disease.
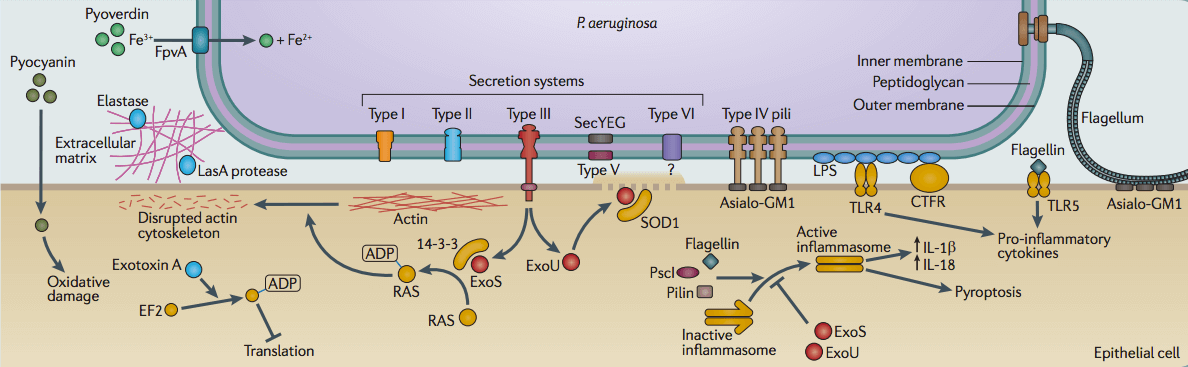
Figure: Pathogenesis of Pseudomonas aeruginosa. Image Source: Microbe Wiki.
a. Bacterial Attachment and Colonization
- The first step in the pathogenesis of disease caused by P. aeruginosa is the entry of the bacteria into the host.
- The route of entry might be different in different individuals, but in the case of nosocomial or acquired infections, the entry usually occurs through punctured skin and tissues.
- The initial colonization of host tissue is brought about by factors like the flagellum and pili.
- The flagellum supports the movement of bacteria through the host body to reach the target sites.
- Once in the target sites, structures like the Type IV pili bind to the glycosphingolipid present on the host epithelial cells.
- Colonization is also enhanced by the production of proteolytic enzymes like elastase that degrade the elastin protein of the tissue to generate a path of infection.
b. Invasion
- The colonization of host tissue by P. aeruginosa is followed by the release of the Type III secretion system which delivers proteins directly from the cytoplasm of P. aeruginosa into the cytoplasm of the host cells.
- The system delivers cytotoxins among which, Exo S and Exo T are the most lethal ones.
- These are bifunctional cytotoxins that possess both Rho GTPase-activating protein and ADP ribosyltransferase activities.
- The toxins then inhibit phagocytosis by disrupting actin cytoskeleton rearrangement, focal adhesions, and signal transductions.
- Exo U is another toxin present in the secretion system that contributes directly to acute cytotoxicity towards epithelial cells and macrophages.
- Similarly, other toxins induce an adenylate cyclase activity that affects intracellular cAMP levels and cytoskeleton reorganization.
c. Biofilm formation
- Resistance against antimicrobial agents is essential pathogenesis of infections caused by P. aeruginosa.
- A different component like the exopolysaccharide, rhamnolipid, pyoverdine, and proteinaceous surface appendages are involved in the process of biofilm formation.
- During biofilm formation, cell differentiation occurs, and oxygen and water-filled channels are formed to provide nutrition to the deep-rooted cells of the mature biofilm.
- Studies have shown that cells growing in biofilms have up to 1000 fold more resistance to antibodies than the free-swimming cells.
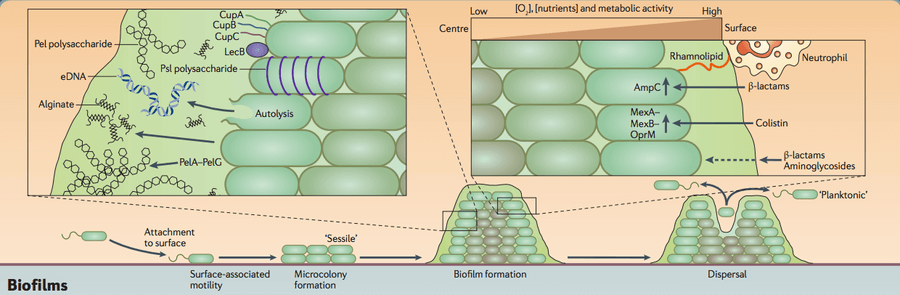
Figure: Biofilm formation in Pseudomonas aeruginosa. Image Source: Microbe Wiki.
Clinical Manifestation of Pseudomonas aeruginosa
Pseudomonas aeruginosa can result in different infections depending on the target sites and cells of the bacteria. The infections can range from mild urinary tract infections to fatal septic shock or bacteremia.
a. Pneumonia
- Pneumonia caused by P. aeruginosa is often hospital-acquired with the common source being contaminated bronchoscopes.
- The common clinical symptoms associated with this infection include fever and chills and difficulty in breathing.
- During the infection of the respiratory tract, the organisms colonize the entire upper and lower respiratory tract.
- This might result in yellow, green or sometimes, bloody mucus during cough.
- Extensive bronchopneumonia with abscess formation and necrosis of the alveolar walls in all lobes of the lung is an important manifestation.
b. Sepsis/ Bacteremia
- Like in most nosocomial infections, bacteremia or sepsis is an essential indication of P. aeruginosa.
- The sepsis is indicated by irregular alterations of the cardiac dynamics, which ultimately leads to decreased cardiac output, metabolic acidosis, and even multiorgan failure.
- Endocarditis is a common manifestation when the bacteria eventually reached the cardiac valves and forms biofilms.
- Different virulence factors of the organism induce the inflammatory response of the host immune system, which eventually leads to septic shock.
- The movement of bacteria through the bloodstream further increases the chances of the movement of infections through the body.
c. Urinary tract infection
- Urinary tract infection by P. aeruginosa has also been observed in some patients that use external medical devices or during dialysis.
- The source of urinary tract infection by P. aeruginosa is the entry of the organism from the skin.
- The bacteria might even reach the urinary bladder where it forms biofilms to protect itself from the host defenses.
- The common symptoms associated with such infections include painful urination, cloudy or bloody urine with pain in the pelvic region.
- The bacteria in the urinary tract induces invasion of tissues resulting in necrosis and tissue damage.
Lab Diagnosis of Pseudomonas aeruginosa
Laboratory diagnosis of infections caused by P. aeruginosa is based on the isolation and identification of P. aeruginosa from the clinical samples.
a. Sample collection
- The sample collected for the diagnosis of the infection depends on the site of infection.
- In the case of pneumonia, the sample might be sputum or respiratory aspirates. Similarly, urine is the sample for urinary tract infections.
- The samples collected should be appropriate in order to detect the presence of the organism.
- If necessary, appropriate transport media should be used.
b. Morphological, Cultural and Biochemical Characteristics
- The organism present in the sample is isolated on culture media like blood agar or eosin-methylthionine blue agar.
- The growth is best observed at 37°C, but the growth can be observed at a temperature as high as 42°C.
- The presence of Gram-negative rods on microscopic observation provides a piece of preliminary information on the diagnosis.
- The colonies on different media help distinguish the organism from other similar organisms.
- An important characteristic of P. aeruginosa is the production of fluorescein, which can be detected via visual examination under UV light.
- For further confirmation, sets of biochemical tests can be performed.
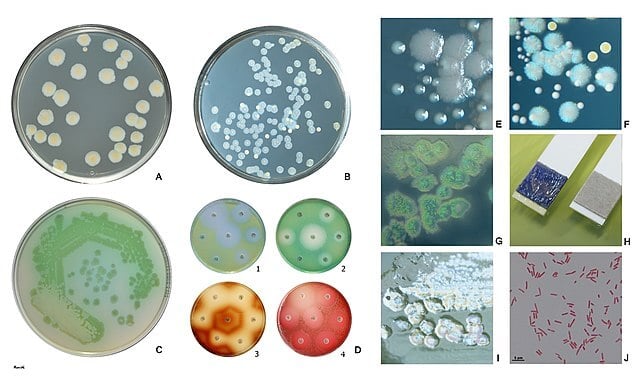
Figure: Pseudomonas aeruginosa is a non-fastidious, Gram-negative (Fig. J), oxidase-positive (Fig. H), nonfermenting rod. P. aeruginosa produces pyoverdin, a water-soluble yellow-green pigment (Fig. A, C, D1, D2). Many P. aeruginosa strains also produce the blue pigment pyocyanin (Fig. B, F). When pyoverdin combines with pyocyanin, the bright green color characteristic of P. aeruginosa is created (Fig. C). Some strains rarely produce other pigments: brown pyomelanin (D3) or red pyorubrin (D4). For the isolation and presumptive identification from clinical and environmental samples a selective agar containing cetrimide can be used (Fig. G).
Fig. A, B Trypticase soy agar (B: P.aeruginosa + S.aureus), Fig. C, D, I Mueller-Hinton agar Fig. E Larger colonies of P. aeruginosa and smaller colonies of Enterococcus faecalis on trypticase soy agar. Reflected light. Fig. F Bluish colonies of P. aeruginosa, yellow colonies of S. aureus, and white colonies of Enterococcus faecalis on trypticase soy agar.
Fig. I Plaques are frequently found in freshly isolated strains, especially in the area of confluent growth. In some strains, these are caused by phage, in others by bacteriocins.
Image Source: HansN (Wikimedia).
c. Immunological tests
- Serological methods such as crossed immune electrophoresis (CIE), Western immunoblot, and enzyme-linked immunoassay (ELISA) to detect P aeruginosa are not routinely performed.
- However, these tests can work as a confirmatory test for the detection of P. aeruginosa cells.
- These tests usually detect antigens like elastase, exotoxin A and alkaline proteases. The detection of these antigens often confirms the presence of P. aeruginosa.
- The serological tests are often rapid, which helps in the early diagnosis of disease and might help in preventing chronic infections.
d. Molecular Diagnosis
- Over recent years, the use of a molecular diagnostic method for the detection of microorganisms has been widespread.
- These tests are often rapid and provide extremely rapid results, which allow an accurate diagnosis.
- Some of the common molecular methods include PCR and DNA hybridization. Besides, RNA sequencing can also be performed to diagnose infections caused by P. aeruginosa accurately.
Treatment of Pseudomonas aeruginosa
- The method of treatment employed by the clinicians depends on the severity of the infection.
- In the case of mild infections, courses of IV antibiotics are adequate enough for treatment; however, under deeper infections, surgical debridement might also be required.
- In patients with respiratory failure, pneumonia, sepsis, or other systemic infections, ICU admissions might be necessary.
- In addition to the broad-spectrum antibiotics, double pseudomonal coverage might also be needed.
- Common antibiotics that are used as first-line therapy include carbapenems, cephalosporins, aminoglycosides, and fluoroquinolones.
- In the case of systemic infections, longer exposure to medicinal therapy might be required. In infections caused by medical devices like catheters, removal of such devices is done.
Prevention of Pseudomonas aeruginosa
- Since most of the infections caused by P. aeruginosa are nosocomial infections, specific precautions can be taken in the hospital environment to prevent infections.
- The health personnel are advised to follow strict infection control precautions.
- Strict adherence to hand hygiene and regular use of gowns and gloves are advised.
- In some cases, the infections might be induced due to poor sanitary habits of the patients, so the hygiene of the patient should also be maintained.
- Careful cleaning and monitoring of respirators, catheters, and other instruments are also required.
- The use of topical antibacterial agents to burns has been known to dramatically reduces the incidence of P. aeruginosa infections.
Industrial uses / Applications of Pseudomonas aeruginosa
- Various secondary metabolites produced by P. aeruginosa are known to be vital in the control of multiple drug-resistant bacteria.
- An esterase enzyme produced by P. aeruginosa has the ability to hydrolyze racemic methyl ester of β-acetylthioisobutyrate to result in the formation of D-enantiomer. The enantiomer thus formed is the precursor of captopril, which is an essential drug in the management of congestive heart failure and hypertension.
- The vanillin produced by P. aeruginosa is used as a component of natural flavors and is used in food, cosmetic and pharmaceutical products.
- Rhamnolipids produced by P. aeruginosa have been used in the food industry to increase the shelf life of food as a result of their antimicrobial properties.
- The proteases have multiple applications in various food and textile industries.
- The pigments of P. aeruginosa are considered bio pigments that are used as coloring agents with some even used for remediation of harmful pesticides and chemicals.
Video on Pseudomonas aeruginosa
References
- Topley W. W. C (2007). Topley and Wison’s Microbiology and Microbial Interactions; Bacteriology, 2 Vol. Tenth Edition. John Wiley and Sons Ltd.
- Bergey, D. H., Whitman, W. B., De, V. P., Garrity, G. M., & Jones, D. (2009). Bergey’s manual of systematic bacteriology: Vol. 2. New York: Springer.
- Palleroni, N.J. (2015). Pseudomonas. In Bergey’s Manual of Systematics of Archaea and Bacteria (eds M.E. Trujillo, S. Dedysh, P. DeVos, B. Hedlund, P. Kämpfer, F.A. Rainey and W.B. Whitman). https://doi.org/10.1002/9781118960608.gbm01210
- Klockgether, Jens, and Burkhard Tümmler. “Recent advances in understanding Pseudomonas aeruginosa as a pathogen.” F1000Research vol. 6, 1261. 28 Jul. 2017, doi:10.12688/f1000research.10506.1
- de Bentzmann S, Plésiat P. The Pseudomonas aeruginosa opportunistic pathogen and human infections. Environ Microbiol. 2011 Jul;13(7):1655-65. doi: 10.1111/j.1462-2920.2011.02469.x. Epub 2011 Mar 30. PMID: 21450006.
- Iglewski BH. Pseudomonas. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 27. Available from: https://www.ncbi.nlm.nih.gov/books/NBK8326/
- Morales, Gracia et al. “Structure of Pseudomonas aeruginosa populations analyzed by single nucleotide polymorphism and pulsed-field gel electrophoresis genotyping.” Journal of bacteriology vol. 186,13 (2004): 4228-37. doi:10.1128/JB.186.13.4228-4237.2004
- Wilson MG, Pandey S. Pseudomonas Aeruginosa. [Updated 2020 Sep 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557831/
- Berube, Bryan J et al. “Pseudomonas aeruginosa: breaking down barriers.” Current genetics vol. 62,1 (2016): 109-13. doi:10.1007/s00294-015-0522-x
- Orji Frank Anayo, Ezeanyanso Chika Scholastica, Onyemali Chidi Peter, Ukaegbu Gray Nneji, Ajunwa Obinna and Lawal Oluwabusola Mistura (October 2nd 2019). The Beneficial Roles of Pseudomonas in Medicine, Industries, and Environment: A Review, Pseudomonas Aeruginosa – An Armory Within, Dinesh Sriramulu, IntechOpen, DOI: 10.5772/intechopen.85996.
- Ben Haj Khalifa A, Moissenet D, Vu Thien H, Khedher M. Les facteurs de virulence de Pseudomonas aeruginosa : mécanismes et modes de régulations [Virulence factors in Pseudomonas aeruginosa: mechanisms and modes of regulation]. Ann Biol Clin (Paris). 2011 Jul-Aug;69(4):393-403. French. doi: 10.1684/abc.2011.0589. PMID: 21896403.
- Alhazmi, A. (2015). Pseudomonas aeruginosa – Pathogenesis and Pathogenic Mechanisms. International Journal of Biology, 7(2). doi:10.5539/ijb.v7n2p44
- Tramper-Stranders, G A et al. “Diagnostic value of serological tests against Pseudomonas aeruginosa in a large cystic fibrosis population.” Thorax vol. 61,8 (2006): 689-93. doi:10.1136/thx.2005.054726
- Todd F. Hatchette, Rekha Gupta, Thomas J. Marrie, Pseudomonas aeruginosa Community-Acquired Pneumonia in Previously Healthy Adults: Case Report and Review of the Literature, Clinical Infectious Diseases, Volume 31, Issue 6, December 2000, Pages 1349–1356, https://doi.org/10.1086/317486
- Van der Bij AK, Mol M, van Westreenen M, Goessens WH, Pitout JD. The laboratory diagnosis of Pseudomonas aeruginosa that produce metallo-β-lactamases in a Dutch tertiary care centre. Scand J Infect Dis. 2011 Aug;43(8):596-602. doi: 10.3109/00365548.2011.574148. Epub 2011 Apr 21. PMID: 21506891.
- Fujitani S, Sun HY, Yu VL, Weingarten JA. Pneumonia due to Pseudomonas aeruginosa: part I: epidemiology, clinical diagnosis, and source. Chest. 2011 Apr;139(4):909-919. doi: 10.1378/chest.10-0166. PMID: 21467058.
- Dropulic, L. K., Leslie, J. M., Eldred, L. J., Zenilman, J., & Sears, C. L. (1995). Clinical Manifestations and Risk Factors of Pseudomonas aeruginosa Infection in Patients with AIDS. Journal of Infectious Diseases, 171(4), 930–937. doi:10.1093/infdis/171.4.930
- Anayo et al. (2019). The Beneficial Roles of Pseudomonas in Medicine, Industries and Environment. Pseudomonas aeruginosa; An armory within.DOI: 10.5772/intechopen.85996.

Very helpful, Thank you. but how do we cite this?
You can cite as follows:
Sapkota, A. 2023. Pseudomonas aeruginosa- An Overview – Microbe Notes. Available from: https://microbenotes.com/pseudomonas-aeruginosa/. Accessed On: 06-03-2024.
Pseudomonas gives VP test negative, doesn’t it??
Hello Rasika, Yes it give Negative, the symbol in the bracket was mistaken, I have made it (-) now. Thank you.