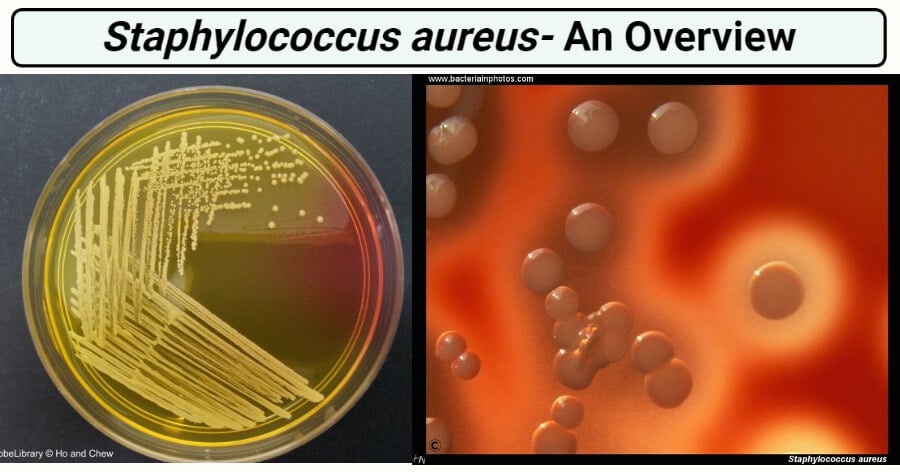
Image Source: ASM and Bacteria in Photos.
Interesting Science Videos
Habitat of Staphylococcus aureus
- The natural habitat is mammalian body surfaces.
- They are normal flora of the skin and mucous membrane.
- Also present in the nose / the anterior nares.
- They can also be found in Pharynx.
- Found in stratified epithelial cells or mucous or serum constituents associated with these cells.
- Found in skin/nasal passage and axillae of humans.
- They act as a benign or symbiotic relationship with the hosts.
- Enterogeneric strains of S. aureus are found in various food products.
- They may survive on dry skin.
- Thirty percent (30%) of the normal human healthy population is affected by S. aureus as it asymptomatically colonizes on the skin of the human host.
Morphology of Staphylococcus aureus
- Gram-positive, singly, in pairs, or in a short chain of 3-4 bacteria.
- Irregular clusters of cells.
- 1 um in diameter
- Spherical colonies in clusters in two planes.
- Cell wall- very thick peptidoglycan layer
- Non-Flagellated, Non-Motile and Non-Sporing
- They are capsulated.
- Grapes like clusters arrangement.
Cultural characteristics of Staphylococcus aureus
- Staphylococci grow readily on most bacteriologic media under aerobic or microaerophilic conditions.
- Colonies on solid media are round, smooth, raised, and glistening.
- S. aureus usually forms gray to deep golden yellow colonies.
- Mannitol Salt Agar: circular, 2–3 mm in diameter, with a smooth, shiny surface; colonies appear opaque and are often pigmented golden yellow.
- Tryptic Soy Agar: circular, convex, and entire margin.
- Blood Agar: beta-hemolysis.
- Brain heart infusion agar: Yellow pigmented colonies.

Figure: Staphylococcus aureus in Mannitol Salt Agar. Image Source: ASM.

Figure: Staphylococcus aureus colonies on blood agar, beta-hemolysis. Image Source: Bacteria in Photos.

Figure: Staphylococcus aureus on Tryptic Soy Agar. Image Source: http://www.bacteriainphotos.com/s.aureus.html
Biochemical characteristics of Staphylococcus aureus
- Catalase positive
- Oxidase negative
- OF test – fermentative
- Coagulase positive: the presence of free and /or bound coagulase
- Indole negative
- Gas negative
- Hydrogen sulfide negative
- Methyl red positive
- VP positive
- Nitrate reduction positive
- Gelatin hydrolysis positive
- Beta hemolysis on Blood agar
- Citrate positive
- Motility negative
- PYR negative
- Urease positive
Virulence factors of Staphylococcus aureus
A. Cell wall components
- Polysaccharide Capsule: inhibits phagocytosis
- Peptidoglycan: activates complement, IL-1, chemotactic to PMNs
- Teichoic acid: species-specific, mediate binding to fibronectin
- Protein A: It binds to the Fc region of IgG and complement, exerting an anti-opsonin effect.
- Fibronectin binding protein (FnBP): promote binding to, mucosal cells and tissue matrices.
- Clumping factor: FnBP enhances the clumping of the organism in presence of plasma.
B. Enzymes
- Catalase enzyme: conversion of hydrogen peroxide into water and oxygen
- Coagulase enzyme and clumping factor: an enzyme-like protein that clots oxalated or citrated plasma.
- Other enzymes: hyaluronidase (spreading factor), staphylokinase(fibrinolysis), proteinases, lipases, β- lactamases
C. Toxins
- Exotoxins: comprises of four toxins α,β,γ,δ: also called hemolysin,
– α exotoxins- heterogenous protein acts on a broad spectrum of eukaryotic cell membranes
– β exotoxins- degrades sphingomyelin
– δ exotoxins- disrupts biological membrane
– γ exotoxins- interact with two proteins to form six potential two-component toxins. All six toxins lyse WBC by pore formation in the cellular membranes that increase cation permeability - Panton-Valentine leukocidin: composed of two components S and F which act synergistically to kill white blood cells
- Exfoliative toxins: composed of type A- located on phage and heat stable and type B- plasmid-mediated and heat-labile: yield generalized desquamation scalded skin syndrome
- Toxic shock syndrome toxins (TSST-1): prototypical superantigen which binds with MHC-II yielding T-cell stimulation. Toxic is associated with fever, shock, and multisystem involvement.
- Enterotoxins: altogether 15 enterotoxins(A-E, G-P), heat stable, resistant to gut enzymes
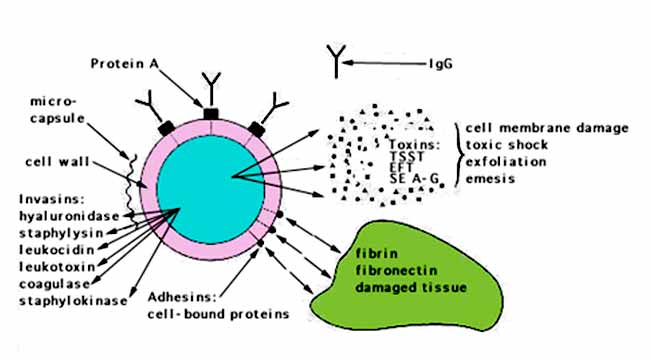
Figure: Virulence determinants of Staphylococcus aureus. Image Source: Kenneth Todar, Ph.D.
Clinical manifestation of Staphylococcus aureus
A. Localized skin infections
- Infections are small superficial abscesses involving hair follicles, sweat, or sebaceous glands.
- Subcutaneous abscesses called furuncles (boils) often formed around foreign bodies.
- Carbuncles are larger, deeper, multiloculated skin infections that can lead to bacteremia.
- Impetigo is usually localized, superficial, spreading crusty skin lesions.
B. Deep localized infections
- Metastatic from superficial infections or skin carriage or may result from trauma.
- Acute infection of joint space in children.
C. Acute endocarditis
- Generally associated with intravenous drug users.
- Bacteria can be introduced into soft tissue and the bloodstream.
D. Septicemia
- Generalized infection with sepsis or bacteremia associated with a known focus or not.
E. Pneumonia
F. Nosocomial infections
- Hospital-associated infections often of wounds or bacteremia associated with catheters.
G. Toxin mediated infections
Toxic shock syndrome
- High Fever
- Rash
- Vomiting
- Diarrhea
- Hypotension
- Multiorgan involvement
Staphylococcal gastroenteritis
- Nausea
- Vomiting
- Diarrhea
Scalded skin syndrome
- The appearance of superficial bullae.
- Marked epithelial desquamation.
Laboratory Diagnosis of Staphylococcus aureus
Microscopy
- Microscopy is useful for pyogenic infections but not blood infections or toxin-mediated infections.
- A direct smear for Gram staining may be performed as soon as the specimen is collected.
- The Gram stain showing typical Gram-positive cocci that occur singly and in pairs, tetrads, short chains, and irregular grape-like clusters can be suspected to be S. aureus.
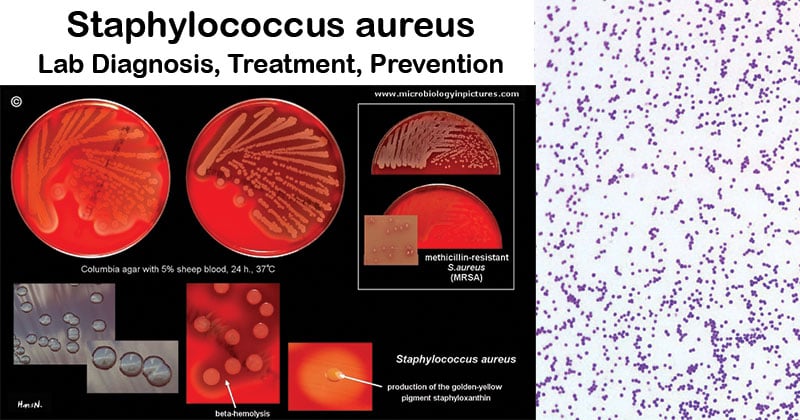
Image Source: Microbiology in pictures and Sanmukh Joshi.
Culture
Growth medium
- The organism is isolated by streaking material from the clinical specimen (or from a blood culture) onto solid media such as blood agar, tryptic soy agar, or heart infusion agar.
- Specimens likely to be contaminated with other microorganisms can be plated on mannitol salt agar containing 7.5% sodium chloride, which allows the halo-tolerant staphylococci to grow.
- The inoculated plates should be incubated at 35°C to 37°C for 24 to 48 hours.
- On Blood agar, growth occurs abundantly within 18 to 24 hours. Round, raised, opaque, yellow to golden yellow colonies of 1-2mm in diameter are seen with or without beta hemolysis.
- On Mannitol Salt Agar (MSA), a selective media, S. aureus being a mannitol fermenting bacteria, gives yellow or gold colonies.
- An 18 h to 24 h culture can be used as the inoculum for additional tests.
- Isolates should be subcultured at least once on a nonselective medium after initial isolation before being used in a diagnostic test that requires pure culture or heavy inoculum.
Presumptive identification
The presumptive identification of S. aureus rests on the isolation of:
- Large mannitol fermenting colonies on MSA
- Gram-positive cocci in clusters
- Catalase-positive organisms
- Coagulase-positive organisms
Confirmatory tests
Confirmatory tests include biochemical tests, molecular probes, or mass spectrometry.
Biochemical reactions
Tests for clumping factor, coagulase, hemolysins, and thermostable deoxyribonuclease are routinely used to identify S. aureus.
Identification of toxins
- This is important for more severe cases like toxic shock syndrome and food poisoning.
- Toxins produced by S. aureus, such as enterotoxins A to D and TSST-1 may be identified using agglutination tests.
- The tests are determined by the clumping of the latex particles by the toxins present in the samples.
- Commercial latex agglutination tests are available for this purpose.
Nucleic acid amplification tests
- Commercial nucleic acid amplification tests are available for the direct detection and identification of S. aureus in clinical specimens.
- Whereas the earlier versions of these tests required manual extraction of bacterial DNA and testing multiple specimens in large batches, integrated processing of specimens (extraction, gene amplification, and target detection) is now performed on highly automated platforms with disposable reagent strips or cartridges.
- They are useful for screening patients for carriage of methicillin-sensitive S. aureus (MSSA) and MRSA.
Treatment of Staphylococcus aureus infection
- Localized infections are managed by incision and drainage while antibiotic therapy is indicated for systemic infections.
- Oral therapy can include trimethoprim-sulfamethoxazole, doxycycline or minocycline, clindamycin, or linezolid; vancomycin is the drug of choice for intravenous therapy, with daptomycin, tigecycline, or linezolid acceptable alternatives.
- Hospital- and community-acquired infections with methicillin-resistant Staphylococcus aureus (MRSA) are a significant worldwide problem. Hence, empirical therapy should include antibiotics active against MRSA strains.
- Treatment is symptomatic for patients with food poisoning (although the source of infection should be identified so that appropriate preventive procedures can be enacted)
Prevention of Staphylococcus aureus infection
- Proper cleansing of wounds and the use of disinfectants help prevent infections.
- Thorough hand washing and covering of exposed skin help medical personnel prevent infection or spread to other patients.
- Patients and staff carrying epidemic strains, particularly MRSA, should be isolated.
- Patients may be given disinfectant baths or treated with a topical antibiotic to eradicate carriage of MRSA.
- Infection control programs should be used in hospitals.
References and Sources
- Murray, P. R., Rosenthal, K. S., & Pfaller, M. A. (2013). Medical microbiology. Philadelphia: Elsevier/Saunders.
- BLAIR J. E. (1958). Laboratory diagnosis of staphylococcal infections. Bulletin of the World Health Organization, 18(3), 291–307.
- https://www.ncbi.nlm.nih.gov/books/NBK8448/
- https://microbeonline.com/staphylococcus-aureusdisease-properties-pathogenesis-and-laboratory-diagnosis/
- https://www.health.state.mn.us/diseases/staph/treat.html
- https://www.news-medical.net/health/Staphylococcus-Aureus-Diagnosis.aspx

Very resourcefull👍
Very helpful and resourceful. Has a lot of information
Very helpful and resourceful. Has a lot of information that you is difficult to find elsewhere.