Interesting Science Videos
Habitat of Clostridium perfringens
- Clostridium perfringens are isolated from fecal specimens from humans and animals.
- They are an inhabitant of human normal intestinal flora.
- They are present in nature and can be found as a normal component of decaying vegetation, marine sediments, and soil.
- Beef, poultry, gravies and dried or pre-cooked foods are common sources of Clostridium perfringens infections.
- Also found in raw meat and poultry.
- Encountered in improperly sterilized (canned) foods in which endospores have germinated.
Morphology of Clostridium perfringens
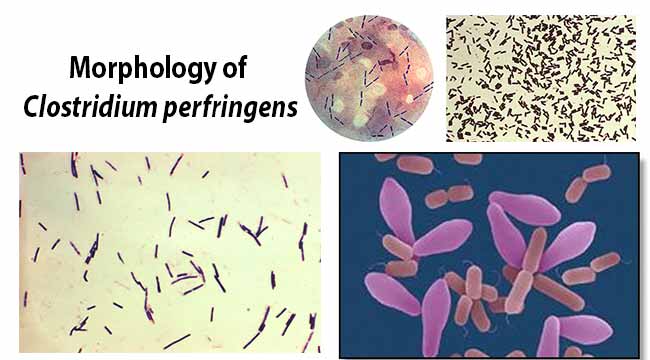
- Clostridium perfringens is large rectangular gram-positive bacilli with rounded or truncated ends.
- It is pleomorphic with straight or curved rods.
- Size is about 3-8 µm X 0.4-1.2 µm.
- It is a capsulated, non-motile, and non-flagellated pathogenic bacteria.
- It contains spores with central or sub-terminal spores but spores are rarely seen.
- Endospores are able to survive long periods of exposure to air and other adverse environmental conditions.
- Spores are wider than the bacillary body, giving bacillus a swollen appearance resembling a spindle.
- It is heat resistant anaerobic bacterium.
- It has a protective thick cell wall made up of peptidoglycan.
- It is able to glide across the surface because their bodies are lined with filaments from end-to-end.
Genome Structure
- Single circular chromosome
- 6 million base pair
- GC content from 24 to 55%
- Contains 10 rRNA gene and 96 tRNA genes.
Cultural characteristics of Clostridium perfringens
- It is an anaerobic bacteria but can grow under micro-aerophilic conditions.
- They form large, translucent, flat, and filamentous colonies with irregular edges.
- PH: 5.5 to 8.0 (Average PH: 7.2)
- Temperature: 20°C to 50°C (Average: 37°C)
- At 45°C, generation time is 10 minutes.
Clostridium perfringens on Robertson’s Cooked Meat Broth
- Saccharolytic species turn meat pink. Meat particles remain intact.
- Proteolytic species turn meat black with a foul smell.
- Acidic reactions
- Produces gas
Clostridium perfringens on Litmus Milk
- Stormy fermentation and acid clot in litmus milk
Clostridium perfringens on Blood Agar
- Target hemolysis
- Double zone of beta hemolysis
- Inner zone: complete hemolysis
- Outer zone: partial hemolysis
Clostridium perfringens on Tryptose Sulfite Cycloserine (TSC) Agar
- Isolation and enumeration of both vegetative and spores of Clostridium perfringens in food and clinical samples.
Clostridium perfringens on Marshal’s Medium
- Black colonies
Clostridium perfringens on Egg yolk agar media
- Used for the detection of Lecithinase C
Clostridium perfringens on MacConkey Agar
- Green Fluorescent colonies
Biochemical Characteristics of Clostridium perfringens
Virulence Factors of Clostridium perfringens
- Clostridium perfringens, which produces a huge array of invasins and exotoxins, causes wound and surgical infections that lead to gas gangrene, in addition to severe uterine infections.
- The virulence of C. perfringens is attributable largely to its ability to produce at least 16 different toxins and extracellular enzymes. However, no single strain produces this entire toxin panoply.
- Clostridium perfringens produces many different toxins, four of which (alpha, beta, epsilon, iota) can cause potentially deadly syndromes. The toxins cause damage to tissues, blood cells, and blood vessels.
- Clostridial hemolysins and extracellular enzymes such as proteases, lipases, collagenase, and hyaluronidase, contribute to the invasive process.
- Clostridium perfringens also produces an enterotoxin and is an important cause of food poisoning.
- The CPE (for Clostridium perfringens enterotoxin) is a polypeptide of 35.5 kDa that accumulates at the beginning of the sporulation and is excreted to the media when it lysates at the end of the sporulation. It is coded by the CPE gene, present in less than 5% of the type A strains, and it can be located in the chromosome or in an external plasmid.
Pathogenesis of Clostridium perfringens
Invasive infection and Gas gangrenes
- In invasive clostridial infections, spores reach tissue either by contamination of traumatized areas (soil, feces) or from the intestinal tract.
- The spores germinate at low oxidation-reduction potential; vegetative cells multiply, ferment carbohydrates present in the tissue, and produce gas.
- The distention of tissue and interference with blood supply, together with the secretion of necrotizing toxin and hyaluronidase, favor the spread of infection.
- Tissue necrosis extends, providing an opportunity for increased bacterial growth; hemolytic anemia; and, ultimately, severe toxemia and death.
- The toxin involved in gas gangrene is known as α-toxin, which inserts into the plasma membrane of cells, producing gaps in the membrane that disrupt normal cellular function.
Diarrheal disease ( C. perfringens type A food poisoning)
- Illness is caused by eating food contaminated with large numbers of C. perfringens bacteria that produce enough toxin in the intestines to cause illness.
- C. perfringens can survive high temperatures. During cooling and holding of food at temperatures from 54°F–140°F (12°C–60°C), the bacteria grows. It can grow very rapidly between 109°F–117°F (43°C–47°C).
- If the food is served without reheating to kill the bacteria, live bacteria may be eaten. The bacteria produce a toxin (CPE toxin for Clostridium perfringens toxin) inside the intestine that causes illness.
- Upon ingestion of heavily contaminated food, vegetative cells of a chromosomal CPE strain survive passage into the intestines, where they initially multiply but then soon sporulate; Spo0A and alternate sigma factors control both in vivo sporulation and CPE production.
- The toxin accumulates in the mother cell until it is released at the completion of sporulation when the mother cell lyses.
- The released toxin then acts, to damage the intestines and trigger diarrhea and abdominal cramping.
Clinical Features of Clostridium perfringens
Gas gangrene
- Clostridium perfringens is the most common strain of clostridia associated with trauma-induced gas gangrene in humans and is also a major cause of spontaneous (nontraumatic) gas gangrene.
- The classic features of gas gangrene are extensive local tissue destruction progressing to profound shock and death.
- From a contaminated wound (eg, a compound fracture, postpartum uterus), the infection spreads in 1–3 days to produce crepitation in the subcutaneous tissue and muscle, foul-smelling discharge, rapidly progressing necrosis, fever, hemolysis, toxemia, shock, and death.
- At times, the infection results only in anaerobic fasciitis or cellulitis.
Food Poisoning
- perfringens food poisoning usually follows the ingestion of large numbers of clostridia that have grown in warmed meat dishes.
- The toxin forms when the organisms sporulate in the gut, with the onset of diarrhea and abdominal cramps—usually without vomiting or fever—in 7–30 hours.
- The illness suddenly begins and lasts only 1–2 days.
Laboratory Diagnosis of Clostridium perfringens
For Diarrheal Disease
- Laboratories diagnose C. perfringens food poisoning by detecting a type of bacterial toxin in feces or by tests to determine the number of bacteria in the feces.
- A count of at least 106 C. perfringens spores per gram of stool within 48 hours of when the illness began is required to diagnose infection.
For Other Infections
- Specimens consist of material from wounds, pus, and tissue.
- The presence of large gram-positive rods in Gram-stained smears suggests clostridia; spores are not regularly present.
- Material is inoculated into chopped meat–glucose medium and thioglycolate medium and onto blood agar plates incubated anaerobically.
- The growth from one of the media is transferred into the milk. A clot torn by gas in 24 hours is suggestive of C. perfringens.
- After pure cultures have been obtained by selecting colonies from anaerobically incubated blood plates, they are identified by biochemical reactions (various sugars in thioglycolate, action on milk), hemolysis, and colony morphology.
- Lecithinase activity is evaluated by the precipitate formed around colonies on egg yolk media.
- Final identification rests on toxin production and neutralization by specific antitoxin.
Note: C. perfringens rarely produces spores when cultured on agar in the laboratory.
Nagler’s Test
- C. perfringens can be diagnosed by Nagler’s reaction, where the suspect organism is cultured on an egg yolk media plate.
- One side of the plate contains anti-alpha-toxin, while the other side does not.
- A streak of a suspect organism is placed through both sides.
- An area of turbidity will form around the side that does not have the anti-alpha-toxin, indicating uninhibited lecithinase activity.
Tests/reactions
Catalase: Negative, Spot indole: Positive, Lecithinase: Positive, Lipase: Negative, Litmus Milk: Stormy Fermentation, Reverse CAMP plate: Positive, Gas-Liquid Chromatography products: (Acetic, Butyric, and Lactic Acids).
Treatment of Clostridium perfringens Infection
Tissue Infections
- The most important aspect of treatment is prompt and extensive surgical debridement of the involved area and excision of all devitalized tissue, in which the organisms are prone to grow.
- Administration of antimicrobial drugs, particularly penicillin, is begun at the same time.
- Hyperbaric oxygen may be of help in the medical management of clostridial tissue infections. It is said to “detoxify” patients rapidly.
- Antitoxins are available against the toxins of C. perfringens usually in the form of concentrated immune globulins. Polyvalent antitoxin (containing antibodies to several toxins) has been used.
Food Poisoning
- Food poisoning caused by C. perfringens enterotoxin usually requires only symptomatic care.
- Oral rehydration or, in severe cases, intravenous fluids and electrolyte replacement can be used to prevent or treat dehydration.
- Antibiotics are not recommended.
Prevention of Clostridium perfringens Infection
- The growth of C. perfringens spores can be prevented by most importantly cooking food, especially beef, and poultry, thoroughly, to the recommended temperatures.
- Leftover food should be refrigerated to a temperature below 40 °F (4 °C) within two hours of preparation.
- Large pots of food such as soup or stew with meats should be divided into small quantities and covered for refrigeration.
- Leftovers should be reheated to at least 165 °F (74 °C) before serving.
- A rule of thumb is that if the food tastes, smells, or looks different from what it is supposed to, then the food should be avoided. Even if it looks safe, food that has been out for a long time can also be dangerous to eat.
- In case of tissue infections, early and adequate cleansing of contaminated wounds and surgical debridement, together with the administration of antimicrobial drugs directed against clostridia (eg, penicillin), are the best available preventive measures.
- Antitoxins should not be relied on. Although toxoids for active immunization have been prepared, they have not come into practical use.
References and Sources
- Bacteriology, Clostriuidium, Dr. Nidhal Sabry.
- Murray, P. R., Rosenthal, K. S., & Pfaller, M. A. (2013). Medical microbiology. Philadelphia: Elsevier/Saunders.
- UK Standards for Microbiology Investigations, Identification of Clostridium species.
- http://jb.asm.org/content/196/8/1540.full
- http://jb.asm.org/content/early/2014/02/03/JB.01444-13
- http://microbesinfo.com/2015/02/clostridium-perfringens-morphology-cultural-characteristics-classification-and-laboratory-diagnosis/
- http://textbookofbacteriology.net/clostridia_2.html
- http://www.academia.edu/3690750/Isolation_identification_and_characterization_of_Clostridium_perfringens_from_lamb_dysentery_in_Dinajpur_district_of_Bangladesh
- http://www.fda.gov/Food/FoodScienceResearch/LaboratoryMethods/ucm070878.htm
- http://www.life.umd.edu/classroom/bsci424/pathogendescriptions/Clostridium.htm
- http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/clostridium-perfringens-eng.php
- http://www.ppdictionary.com/bacteria/gpbac/perfringens.htm
- http://www.sigmaaldrich.com/technical-documents/articles/analytix/clostridium-perfringens.html
- http://www.slideshare.net/doctortvrao/clostridium
- http://www.slideshare.net/drimtiyzwanii/clostridium-perfringens-31843111
- http://www.slideshare.net/guestfff564/clostridium-perfringens-diapo
- http://www.slideshare.net/ramitapponi/1-32201209
- http://www.sunysccc.edu/academic/mst/microbes/37cperf.htm
- http://www.vetbact.org/vetbact/?artid=29
- https://catalog.hardydiagnostics.com/cp_prod/Content/hugo/Clostridium.htm
- https://en.wikipedia.org/wiki/Clostridium_perfringens
- https://microbewiki.kenyon.edu/index.php/Clostridium_perfringens
- https://mmbr.asm.org/content/55/4/649
- https://mmbr.asm.org/content/77/2/208
- https://www.cdc.gov/foodsafety/diseases/clostridium-perfringens.html
- https://www.jstor.org/stable/4481235?seq=1#page_scan_tab_contents
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC372840/
- https://www.researchgate.net/publication/13910870_Pathogenesis_of_Clostridium_perfringens_Infection_Mechanisms_and_Mediators_of_Shock
- https://www.sciencedirect.com/topics/medicine-and-dentistry/clostridium-perfringens
