The immune system is made up of different immune organs and tissues located all over the body. The immune organs are categorized based on their functions and there are two main categories, which include:
- Primary lymphoid organs provide a development and maturation site for lymphocytes, and
- Secondary lymphoid organs whose function includes trapping antigens from the tissues, and the vascular spaces. They are also the site for lymphocyte interaction with the antigens.
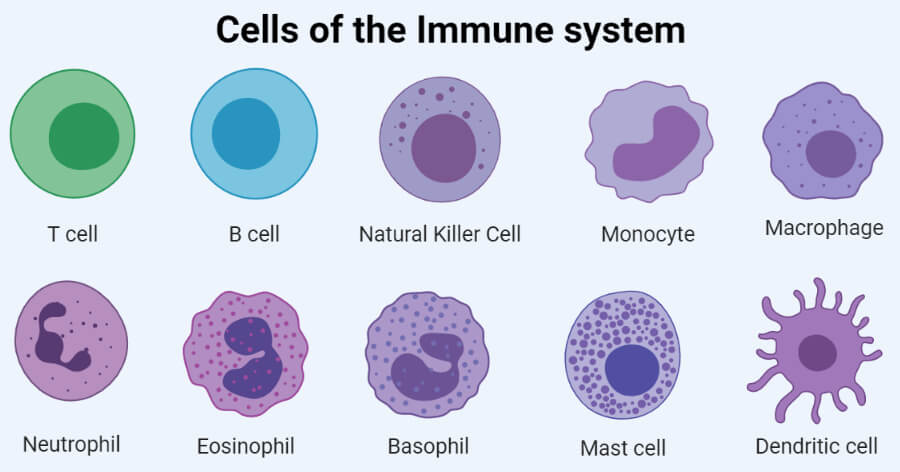
All these organs are connected by the lymphatic system and the blood vessels into a functional unit. In the blood and the lymph and populating the lymphoid organs are various types of white blood cells (leukocytes) that play a key role in the body’s immune responses, therefore defining the cells of the immune system. Nevertheless, white blood cells are an assemblage of different immune cells. White blood cells provide the defense mechanisms of the body fighting off foreign elements (antigens) from the body. Under the White Blood Cells group of cells, they can be categorized into lymphocytes, (including T-lymphocytes, B-lymphocytes, and Natural Killers cells), neutrophils, monocytes, and macrophages.
In all these categories, only the lymphocytes have the characteristics of diversity, specificity, memory, and self/nonself recognition, which are the hallmark features of the adaptive immune responses. All the other cells play additional roles in adaptive immunity such as activation of lymphocytes, increasing the effector mechanisms of antigen clearance by phagocytosis, or secreting various immune-effector molecules. Some white blood cells secrete protein molecules known as cytokines which are immunoregulators (regulate the immune responses). Other major proteins of the immune system include antibodies produced by B-lymphocytes, and complement proteins (activated by antibodies).
Interesting Science Videos
List of Cells of Immune System
- T cells
- B cells
- Natural Killer (NK) Cells
- Monocytes
- Macrophages
- Neutrophils
- Eosinophils
- Basophils
- Mast Cells
- Dendritic Cells
Types of Cells of Immune System
The lymphocytes are the central cells of the immune system which are responsible for adaptive immunity and immunological features of diversity, specificity, memory, and self/non-self recognition. The other immune cells function to engulf and destroy micro-organisms, present antigens and secrete cytokines.
Lymphoid cells (Lymphocytes)
The lymphocytes make up 20%–40% of the body’s white blood cells and 99% of the cells in the lymph. There are about 1011 lymphocytes in the human body. These lymphocytes circulate continuously in the blood and the lymph hence they are able to migrate into the body tissue spaces and lymphoid organs, therefore integrating the immune system to a high degree.
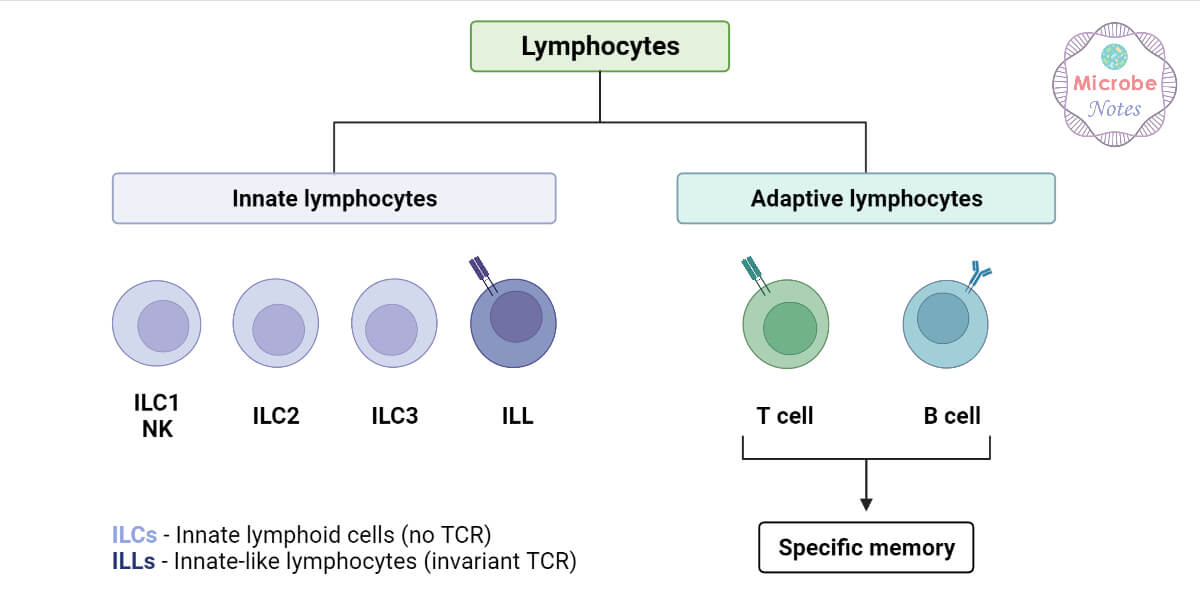
The lymphocytes are broadly divided into three populations based on their functions and cell-membrane components i.e:
1. B-lymphocytes
- B-lymphocytes are also known as B-cells and on lab reports, they are known as CD19 or CD20 cells.
- They are the specialized cells of the immune system whose major function is to produce antibodies also known as immunoglobulins or gamma globulins.
- B-lymphocytes are synthesized and mature in the bone marrow from the hematopoietic stem cells, and after which they mature, migrate, and express themselves by forming unique antigen-binding receptors on their membranes, known as B-cell receptors or antibodies.
- Migration of mature B-cells moves to the bone marrow, lymph nodes, spleen, some parts of the intestines, and the bloodstream.
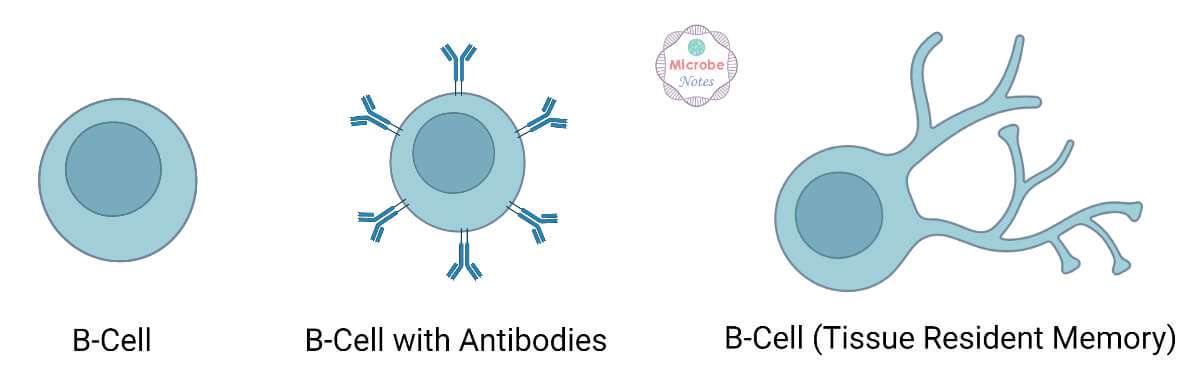
- When a naive B-cell interacts with an antigen for the first time and it has to match membrane-bound receptors (antibodies), the antibodies bound to the B-cell bind the antigen causing the B-cell to divide rapidly, and its progenitors to differentiate into memory B-cells and effector B-cells known as plasma cells.
- The Memory B-cells have a long life span than the naive cells, expressing the same membrane-bound antibody as the parent B-cells.
- The plasma cells are responsible for producing the antibodies that can be secreted into the bloodstream, tissues, respiratory secretions, intestinal secretions, and tears.
- Therefore, antibodies are highly specialized serum protein molecules.
- The plasma cells have a short life span of few days but they secrete large amounts of antibodies during this time, with approximately 2000 molecules of antibodies per plasma cell per second.
- The secreted antibodies play the major effector roles in the humoral immune responses.
- Note that, during maturation, B-cells are trained not to produce antibodies on healthy tissues.
- The antibody molecules are specifically designed for every foreign antigen they encounter and interact like a lock and key mechanism.
- Therefore B-cells have the ability to produce vitally a variety of antibodies for all microbes in our environment, however as stated above, each plasma cell produces only one kind of antibody.
- Antibodies’ varieties are based on their specialized functions in the body with variations in their chemical structure, which ultimately determine the class of antibody.
2. T-Lymphocytes
- T-lymphocytes are also known as T-cells, often named in lab reports as CD3 cells
- They also arise in the bone marrow but migrate to the thymus gland for maturation, where they express a unique antigen-binding molecule on its membrane known as the T-cell receptor.
- The name T originated from its site of maturation, the Thymus.
- Mature T-cells leave the thymus and populate other organs of the immune system, such as the spleen, lymph nodes, bone marrow, and blood.
- Unlike the B-cell receptors that can recognize antigens alone, T-cell receptors only recognize antigens that are bound to cell membrane proteins known as Major Histocompatibility Complex (MHC) molecules.
- The MHC molecule recognizes antigens that are presented to them by antigen-processing cells (APCs) on their cell membrane.
- The two major classes of MHC molecules are Class I MHC molecules, which are expressed by nearly all nucleated cells of vertebrate species, consist of a heavy chain linked to a small invariant protein called 2-microglobulin. Class II MHC molecules, which consist of an alpha and a beta glycoprotein chain, are expressed only by antigen-presenting cells.
- When a naive T cell encounters an antigen combined with an MHC molecule on a cell, the T cell proliferates and differentiates into memory T cells and various effector T cells.
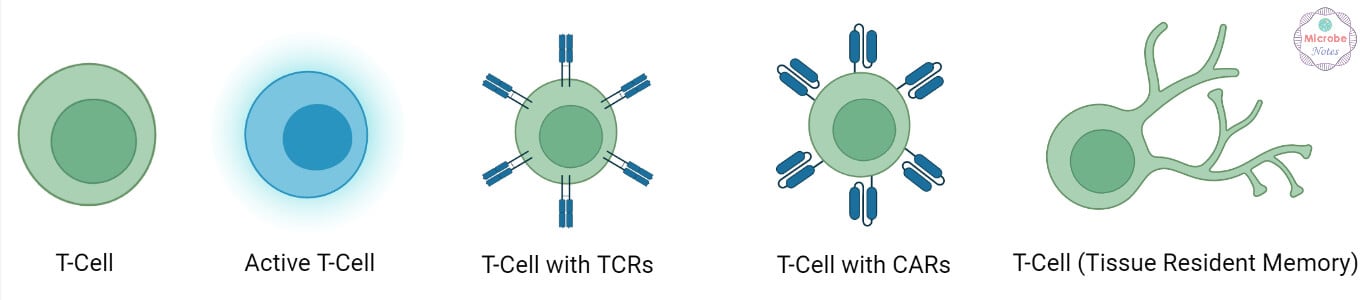
- The T-cells are classified into three categories: T helper (Th), T cytotoxic (Tc), and T suppressor (Ts) cells.
- The Th and Tc cells are differentiated from each other with the presence of their CD4 and CD8 membrane glycoproteins on their surfaces.
- T cells naturally displaying CD4 function as T helper (Th) cells while those displaying CD8 naturally function as T cytotoxic (Tc) cells.
- The Th cells recognize and interact with antigens that are presented on the MHC class II molecule complex, then they become activated becoming effector cells that are able to secrete various growth factors that are collectively known as cytokines.
- The cytokines that are secreted are actively involved in the activation of B-cells, T-cytotoxic cells, macrophages, and other immune cells.
- The cytokine patterns produced by the activated Th cells result in different immune responses. The Th-derived cytokines enable the recognition of an antigen-MHC class I molecule complex by the Tc cells which then proliferate and differentiate into effector cells known as Cytotoxic T-lymphocytes (CTL).
- The T-cytotoxic cells have the ability to induce cytokine secretion, unlike the Cytotoxic T-Cells which do not induce secretion of cytokines, rather they exhibit cell-killing or cytotoxic activity.
- Cytotoxic T-lymphocytes (CTL) play a key role in monitoring the body cells and eliminating any of these cells that display antigens such as tumor cells, cells infected with viruses, and cells of a foreign tissue graft.
- CTLs target foreign antigen (altered self-cells) complexes displayed by the class I MHC molecule.
3. Natural killer cells (NK cells)
- These are large granular lymphocytes, that do not express surface markers like the B and T-cell lineages
- They were first described in 1976 by indications of the presence of a small population of large granular lymphocytes that had a cytotoxic effect against a wide range of tumor cells in the absence of any previous immunization with the tumor.
- These cells also indicated that they play key roles in host defense against tumor cells and cells infected with some, not all viruses.
- They constitute 5-10% of lymphocytes in the human peripheral blood.
- Their ability to recognize antigens is based on two mechanisms:
- They can employ NK cell receptors to distinguish abnormalities such as a reduction in the expression of class I MHC molecules and the abnormal profile of the surface antigens that are displayed by some tumor cells and cells infected by some viruses.
- Secondly, the NK cells also recognize potential target cells which are tumor cells and cells that are infected by viruses. These target cells display antigens against which the immune system has already produced antibody response to as antitumor or antiviral antibodies, that bind to the surfaces of these targets.
- The NK cells express membrane receptors called CD16, which are receptors for the carboxyl-terminal end of the IgG molecule, Fc region. The NK CD16 receptors attach to these antibodies and destroy the targeted cells subsequently, by a mechanism known as the Antibody-dependent cell-mediated cytotoxicity (ADCC).
- Therefore, NK cells play an important role in host defense mechanisms against tumors.
- For example, in humans, the Chediak-Higashi syndrome, an autosomal recessive disorder is associated with impairment in neutrophils, macrophages, and NK cells and an increased incidence of lymphomas. Likewise, mice with an autosomal mutation called beige lack NK cells; these mutations are more susceptible to tumor growth than normal mice following injection with live tumor cells.
- There are some unique NK cells known as the NK1-T-cells which have been recognized to have some combined characteristics of the T-lymphocytes and the Natural Killer cells. They have T-cell receptors (TCRs) that interact with the MHC-like molecule known as a CD1, unlike the normal TCRs of the T-cell which interact with class I or class II MHC molecules. Additionally, like the NK cells, they have variable levels of CD16 and other NK receptors which enable it to kill cells.
- A population that is triggered by NK1-T cells secretes large amounts of cytokines, rapidly. These cytokines support the antibody production by B-cells, also inflammation, and the development and expansion of cytotoxic T-cells.
- Some immunologists view this cell type as a kind of rapid response system that has evolved to provide early help while conventional TH responses are still developing.
Mononuclear Phagocytes
- These are immune cells i.e monocytes that are freely circulating in blood and macrophages that are found in the tissues.
- During hematopoiesis in the bone marrow, granulocyte-monocyte progenitor cells differentiate into promonocytes, which leave the bone marrow and enter the blood, where they differentiate further into mature monocytes.
- Monocytes circulate in the bloodstream for about 8 h, during which they enlarge and then migrate into the tissues and differentiate into specific tissue macrophages or into dendritic cells.
- Differentiation of monocyte into a tissue macrophage involves a number of changes
- The cell enlarges five- to tenfold
- Its intracellular organelles increase in both number and complexity
- It acquires increased phagocytic ability and produces higher levels of hydrolytic enzymes
- It begins to secrete a variety of soluble factors.
- Macrophages are dispersed throughout the body. Some take up residence in particular tissues, becoming fixed macrophages, whereas others remain motile and are called free, or wandering, macrophages.
- Free macrophages travel by amoeboid movement throughout the tissues. Macrophage-like cells serve different functions in different tissues and are named according to their tissue location:
- Alveolar macrophages in the lung
- Histiocytes in connective tissues
- Kupffer cells in the liver
- Mesangial cells in the kidney
- Microglial cells in the brain
- Osteoclasts in bone
- Macrophages are normally in a resting phase but they can be activated by several immune responses.
- For example, the phagocytic mechanism of certain antigens is normally the initial stimulus for macrophages. However, macrophage activity can be further enhanced by cytokines secreted by activated TH cells, by mediators of the inflammatory response, and by components of bacterial cell walls.
- One of the most potent activators of macrophages is interferon-gamma which is secreted by activated TH cells.
- Activated macrophages effectively eliminate potential pathogens than the resting macrophages because they exhibit greater phagocytic activity, an increased ability to kill ingested microbes, increased secretion of inflammatory mediators, and an increased ability to activate T cells.
- Additionally, activated macrophages, but not resting ones, secrete various cytotoxic proteins that help them eliminate a broad range of
pathogens, including virus-infected cells, tumor cells, and intracellular bacteria. - Activated macrophages also express higher levels of class II MHC molecules, allowing them to function more effectively as antigen-presenting cells. Thus, macrophages and TH cells facilitate each other’s activation during the immune response.
- Some of the functions of macrophages include:
- Phagocytosis -Phagocytosis of bacteria, viruses, and other foreign particles is the most important function of macrophages. The macrophages on their cell surfaces have Fc receptors that interact with the Fc component of the IgG, thereby facilitating the ingestion of the opsonized organisms. They also have receptors for C3b, another important opsonin. After ingestion, the phagosome containing the microbe fuses with a lysosome. The microbe within the phagolysosome is killed by reactive oxygen, reactive nitrogen compounds, and lysosomal enzymes.
- Antimicrobial and cytotoxic activities include the oxygen-dependent and oxygen-independent cytotoxicity/killing.
- Antigen processing – After ingestion and degradation of foreign materials, the fragments of antigen are presented on the macrophage cell surface in conjunction with class II MHC proteins for interaction with the TCR of CD4+ helper T cells. Degradation of the foreign protein is stopped following the association of antigen with the class II MHC proteins in the cytoplasm. This is followed by transportation of the complex to the cell surface by transporter proteins.
- Secretion of growth factors important for the development of an immune response such as cytokines, such as interleukin 1 (IL-1), TNF-α, and interleukin 6 (IL-6), that promote inflammatory responses, complement proteins, hydrolytic enzymes, and a cascade of Tumor Necrotic Factors, TNF-α (GM-CSF, G-CSF, M-CSF) that induce and kill tumor cells and promote hematopoiesis.
Granulocytic Cells
- Granulocytes are white blood cells (leukocytes).
- They are classified based on their cellular morphologies and cytoplasmic staining characteristics and they include neutrophils, eosinophils, basophils, or mast cells.
- All granulocytes have multilobed nuclei that make them visually distinctive and easily distinguishable from lymphocytes, whose nuclei are round. The cytoplasm of all granulocytes is replete with granules that are released in response to contact with pathogens.
- These granules contain a variety of proteins with distinct functions: Some damage pathogens directly; some regulate trafficking and activity of other white blood cells, including lymphocytes; and some contribute to the remodeling of tissues at the site of infection.
- Neutrophils have a multilobed nucleus and a granulated cytoplasm that stains with both acid and basic dyes; it is often called a polymorphonuclear leukocyte (PMN) for its multilobed nucleus.
- The eosinophils have a bilobed nucleus and a granulated cytoplasm that stains with the acid dye eosin red (hence its name).
- The basophil has a lobed nucleus and heavily granulated cytoplasm that stains with the basic dye methylene blue.
- Both neutrophils and eosinophils are phagocytic, whereas basophils are not.
- Neutrophils constitute the majority (50% to 70%) of circulating leukocytes and are much more numerous than eosinophils (1%–3%), basophils (≤ 1%), or mast cells (≤ 1%).
Neutrophils
- Neutrophils are produced by hematopoiesis n the bone marrow. They are released into the peripheral blood and circulate for 7–10 h before migrating into the tissues, where they have a life span of only a few days.
- In the bone marrow, a surmountable level of neutrophils is produced in response to the types of infections and they are normally the first cells that arrive at the site of inflammation.
- The resulting transitory increases in the number of circulating neutrophils known as leukocytosis, which is an indicator of an infection, medically.
- The movement of circulating neutrophils into tissues is also known as extravasation.
- Extravasation takes place in several steps:
- Adherence to the vascular endothelium
- Penetration into the gap between adjacent endothelial cells lining the vessel wall
- Penetration into the vascular basement membrane and moving out into the tissue spaces.
- Several substances can be generated during an inflammatory reaction which serves as chemotactic factors. They promote the accumulation of neutrophils at the site of inflammation. Some of these chemotactic factors include complement components, blood-clotting system components, and several cytokines secreted by activated Th Cells and macrophages.
- The functions include:
- Neutrophils are also active phagocytes just like macrophages and the mechanism of phagocytosis is similar to that of macrophages except for the lytic enzymes and bactericidal substances in neutrophils which are contained within primary and secondary granules.
- The neutrophils have larger denser primary granules which are a type of lysosome containing peroxidase, lysozyme, and various hydrolytic enzymes, and smaller secondary granules that contain collagenase, lactoferrin, and lysozyme.
- Both the primary and the secondary granules fuse with the phagosomes and digest and eliminate the contents similar to macrophages.
- Neutrophils also employ both oxygen-dependent and oxygen-independent pathways to generate antimicrobial substances.
- Neutrophils exhibit a larger respiratory burst than macrophages and they are able to generate more reactive oxygen intermediates and reactive nitrogen intermediates.
- Neutrophils also express higher levels of defensins than macrophages.
Eosinophils
- They are motile phagocytic cells that can migrate from the blood into the tissue spaces.
- They have a phagocytic mechanism of eliminating antigens but their role as phagocytic cells is much less significant than that of neutrophils.
- They play a role in defense against multicellular parasitic organisms including worms.
- The secreted contents of eosinophilic granules may damage the parasite membrane. They can be found clustering around invading worms, whose membranes are damaged by the activity of proteins released from eosinophilic granules. Like neutrophils and basophils, eosinophils may also secrete cytokines that regulate B and T lymphocytes, thereby influencing the adaptive immune response.
- In areas where parasites are less of a health problem, eosinophils are better appreciated as contributors to asthma and allergy symptoms.
Basophils
- Basophils are nonphagocytic granulocytes containing large granules that are filled with basophilic proteins that stain blue in standard H & E staining methodologies.
- Naturally, basophils are in the body’s normal circulation but they can be very potent.
- They function by binding to circulating antibodies and react by the content of their granules which are pharmacologically active substances found in their cytoplasm.
- These substances play a major role in certain allergic responses. For example, histamines are the most common and well-known protein in that basophilic granules. They play a role in increasing blood vessel permeability and smooth muscle activity.
- Additionally, just like the eosinophils, basophils are also crucial in response to parasites, and particularly the helminths (worms).
- Basophils also secrete cytokines that assist in the modulation of the adaptive immune response.
Mast Cells
- Mast cells are formed in the bone marrow.
- They are released from the bone marrow into the blood as undifferentiated cells, and when they enter the tissues they then mature.
- Mast cells can be found in a wide variety of tissues, including the skin, connective tissues of various organs, and mucosal epithelial tissue of the respiratory, genitourinary, and digestive tracts.
- Like circulating basophils, these cells have large numbers of cytoplasmic granules that contain histamine and other pharmacologically active substances.
- Mast cells also play an important role in the development of allergies.
- Basophils and mast cells share many characteristics however, their relationship is not unequivocally understood. Some speculations state that basophils are the blood-borne version of mast cells; others speculate that they have distinct origins and functions.
Dendritic Cells
- These are special cells that were discovered by Ralph Steinman in the mid-1970s, and he won a noble prize in 2011 for this discovery.
- The dendritic cells acquire their name because they are covered with long membrane extensions resembling the dendrites of the nerve cells.
- Their membranous extension extends and retracts dynamically, increasing the surface area available for browsing lymphocytes.
- They are very diverse according to research, and they seem to arise from both the myeloid and lymphoid lineages of hematopoietic cells.
- They are not easily isolated by conventional methods because the cell isolation damages their long extensions.
- Dendritic cells generally perform the distinct functions of antigen capture in one location and antigen presentation in another.
- Outside lymph nodes, immature dendritic cells monitor the body for signs of invasion by pathogens and capture intruding or foreign antigens.
- They then process these antigens, then migrate to lymph nodes, where they present the antigen to naïve T cells, initiating the adaptive immune response.
- When acting as guards in the periphery, immature dendritic cells take on their cargo of antigen in three ways.
- engulf it by phagocytosis
- internalize it by receptor-mediated endocytosis
- absorb it by pinocytosis.
- During the maturation process though, they shift from an antigen-capturing phenotype to one that is specialized for the presentation of
antigen to T cells. When transitioning, some attributes are lost and others are gained. Lost is the capacity for phagocytosis and large-scale pinocytosis. - However, the ability to present antigen increases significantly, as does the expression of costimulatory molecules that are essential for the activation of naïve T cells.
- After activation, dendritic cells abandon residency in peripheral tissues, enter the blood or lymphatic circulation, and migrate to regions of the lymphoid organs, where T cells reside, and present antigen.
- There are many types of dendritic cells, although most mature dendritic cells have the same major function, the presentation of antigen to TH cells.
- There are four types of dendritic cells known:
- Langerhans cells
- interstitial dendritic cells
- myeloid cells
- lymphoid dendritic cells.
- Each of these types arises from hematopoietic stem cells via different pathways and in different locations.
- However different, they all constitutively express high levels of both class II MHC molecules and members of the co-stimulatory B7 family.
- Therefore, they are representatively more potent antigen-presenting cells than macrophages and B cells, both of which need to be activated before they can function as antigen-presenting cells (APCs).
- Immature or precursor forms of each of these types of dendritic cells acquire antigen by phagocytosis or endocytosis; the antigen is processed, and mature dendritic cells present it to TH cells.
- Following microbial invasion or during inflammation, mature and immature forms of Langerhans cells and interstitial dendritic cells migrate into draining lymph nodes, where they make the critical presentation of antigen to TH cells that is required for the initiation of responses by those key cells.
- Another type of dendritic cell, the follicular dendritic cell, does not arise in the bone marrow and has a different function from the antigen-presenting dendritic cells.
- Follicular dendritic cells do not express class II MHC molecules and therefore do not function as antigen-presenting cells for TH-cell activation.
- These follicular dendritic cells were named for their exclusive location in organized structures of the lymph node called lymph follicles, which are rich in B cells. Although they do not express class II molecules, follicular dendritic cells express high levels of membrane receptors for antibody, which allows the binding of antigen-antibody complexes.
- The interaction of B cells with this bound antigen can have important effects on B cell responses.
References and Sources
- Kuby Immunology Kuby, 5th Edition
- Kuby Immunology, 7th Edition by Judith A. Owen, Jenni Punt, Sharon A. Stranford, Patricia P. Jones
- Microbiology and Immunology by Shubash Chandra Parija: Elsevier
- 6% – https://immunologysystem.blogspot.com/2016/07/granulocytic-cells.html
- 3% – https://quizlet.com/17937095/kubych-2-flash-cards/
- 2% – https://immunologysystem.blogspot.com/2016/07/mononuclear-phagocytes.html
- 1% – https://www.slideshare.net/HodSapthagiriCollege/sce-mmuno1-26
- 1% – https://www.coursehero.com/file/p49mvpvi/If-the-pathogen-is-stubborn-neutrophils-release-cytokines-and-attract-other/
- 1% – https://www.brainkart.com/article/Cells-of-the-Immune-System_35295/
- 1% – https://primaryimmune.org/sites/default/files/IDF%20Patient%20Handbook%20Chapter%201.pdf
- 1% – https://med.seu.edu.cn/_upload/article/files/4c/37/03879d2643f0a3ee510a3f684c84/760e6b40-a7bb-477a-9dba-66d0abfc2b04.pdf
- 1% – https://immunologysystem.blogspot.com/2016/07/lymphocytes-constitute-2040-of-bodys.html
- 1% – https://immunologysystem.blogspot.com/2016/07/hematopoietic.html
- 1% – http://www.brainkart.com/article/Cells-of-the-Lymphoreticular-System_17941/
- 1% – http://www.brainkart.com/article/Antigen-presenting-cells_17944/
- 1% – http://pharmacy.uokerbala.edu.iq/wp/wp-content/uploads/2014/10/images_lec_4st_public-health_Cells%2C%20Organs%2C%20and%20%28public%202014%29.pdf

Are T-suppressor cells = T-regulatory ?
Sir please add a note on organs of Immune System
You can find more about organs like thymus, spleen, bone marrow, lymph nodes, malt, etc. from https://microbenotes.com/category/immunology/
Valuable notes