Macrophages are mononuclear cells functioning as professional phagocytes to remove dying, dead or harmful pathogens.
Macrophages are a type of white blood cell of the immune system where they engulf and digest particles that are detected as antigens by other blood cells.
- These are larger phagocytic cells that occur in essentially all types of tissues, and their structure and shape depend on the stage of maturation of the cells.
- Macrophages found in different organs have different names like the macrophages of lungs are called alveolar macrophages, while those in the liver are called Kupffer cells.
- Even though phagocytosis is the primary function of macrophages, these also play an essential role in nonspecific defense as well as in adaptive immunity.
- Macrophages are important blood cells that have important roles in almost all aspects of an organism’s biology as different subsets of macrophages are involved in different functions in the body.
- Macrophages in the body are produced by the differentiation of monocytes in tissues that can then be identified by flow cytometry or immunohistochemical staining.
- Macrophages keep flowing through the blood where they migrate to and circulate within all tissues, patrolling for pathogens or eliminating dead cells and debris.
- Macrophages consist of a specialized group of receptors called Toll-like receptors that recognize products of bacteria and other microorganisms.
Interesting Science Videos
Structure of Macrophages
- The morphology of macrophages depends on the various state of activity of the cells. The size of the cells ranges between 10-30 µm in diameter.
- The cytoplasm of a macrophage contains vacuoles and granules that are basophilic in nature. The nucleus is ovoid and measures about 6-12 µm in diameter.
- In a phase-contrast microscope, peritoneal macrophages contain light gray diffuse cytoplasm with dark gray rod-shaped mitochondria.
- The periphery of the cytoplasm contains finely granular and lacks structures like endoplasmic reticula and attached ribosomes.
- Three different types of vesicles are visible in the cytoplasm in the form of pinocytic vesicles with various sized organelles contained a diner granular material.
- Ribosomes can be observed attached to the external portion of the nuclear membrane that is continuous with the endoplasmic reticula.
- The dense granules in the cytoplasm are mostly secondary lysosomes that are derived from endocytic vacuoles.
- In the case of inflammatory macrophages, slim cytoplasmic extensions are observed that remain tightly intertwined with adjacent epithelioid cells.
- Some observations might even indicate giant cells of granuloma as a result of the fusion of preexisting macrophages.
How do Macrophages work against pathogens? (Immunity)
The primary role of macrophages is homeostasis, where the cells protect the host against foreign invaders and clears necrotic and apoptotic debris post-injury. Macrophages perform these functions by four distinct mechanisms; sensing, chemotaxis, phagocytosis and repair, and adaptive stimulation.
1. Sensing
- Many macrophages remain in the bloodstream as patrolling cells. These macrophages use different intracellular and cell-surface pattern recognition receptors (PRRs) to sense their local environment.
- When these receptors detect appropriate particles, they generate signals that detect the macrophage response.
- The innate receptors of macrophages can recognize molecular patterns that can detect such patterns across a number of species.
- The sensing groups detected by macrophages can be categorized into two groups; pathogen and danger signals and modified host proteins and cellular debris.
- The Toll-like Receptors (TLR) family of receptors is the most predominant pathogen sensing group of molecules with 14 members.
- In addition to the detection of antigens, these receptors also induce inflammatory signaling by the expression of cytokines like IL-6, TNF-α, and IL-2.
- Macrophages also express cell-surface Fc receptors like Fc gamma and Fc epsilon. These receptors bind to antibodies that are already bound to antigens, resulting in phagocytosis.
2. Chemotaxis
- After the sensing of an antigen, macrophages stimulate the expansion of activated T cells and the secretion of chemokines to recruit other effector cells, resulting in neutralization and clearance.
- Some of the common chemokines released by activated macrophages are CCL-3, CCL-4, CCL-5, CXCL-9, etc.
- Other chemokines like CCL-17 and CCL-22 attract Th2 lymphocytes and natural killer cells along with eosinophils and basophils.
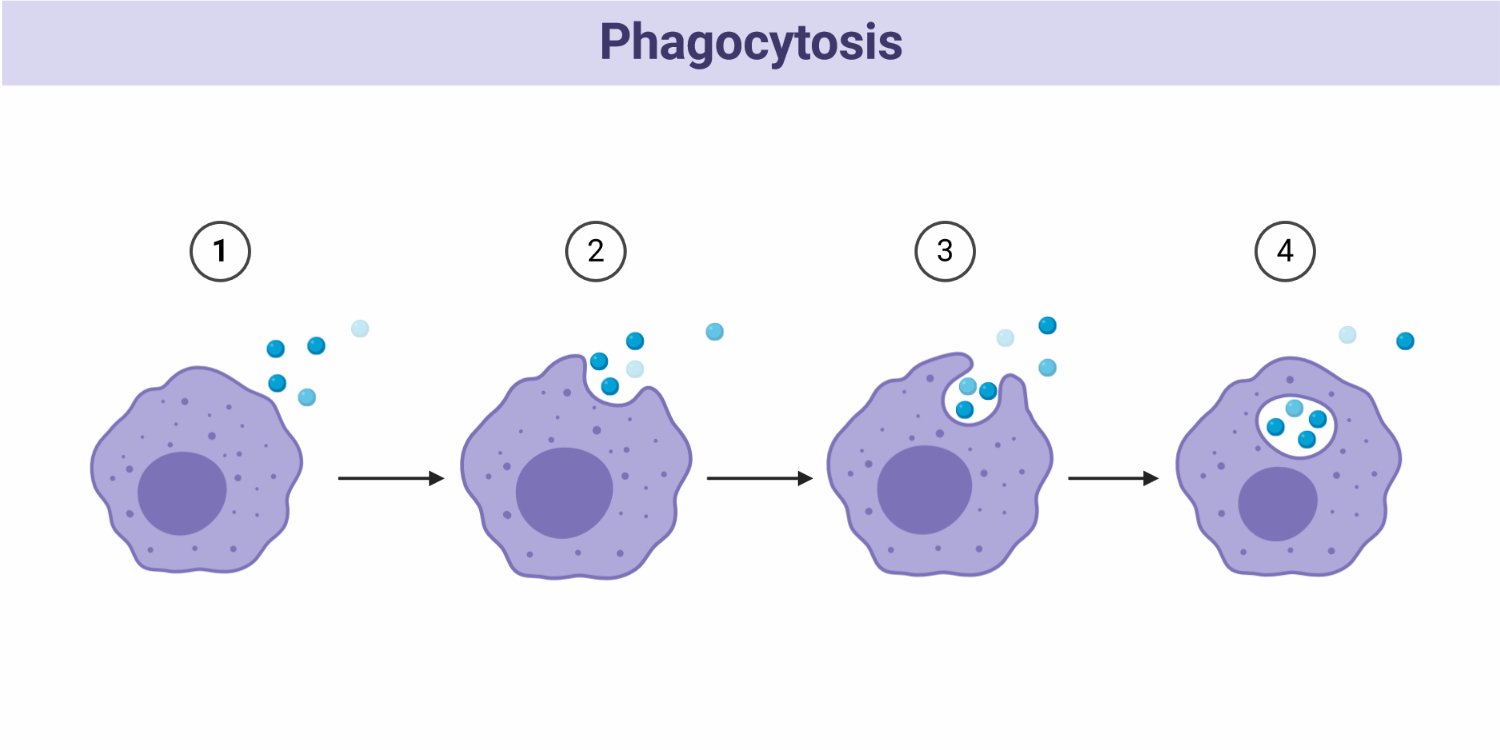
3. Phagocytosis and Tissue repair
- The most important mechanism of immune response by macrophages is phagocytosis for the clearance of damaged and cell debris.
- Macrophages begin to engulf unwanted materials with the help of cell-surface receptors that can identify their targets.
- The materials are sequestered into compartments that fuse with a lysosomal compartment containing a number of highly reactive and toxic molecules.
- Some of the common compounds involved in the destruction of the phagosomal contents are ROS and NO. Nitric acid regulates the level of ROS to produce toxic reactive nitrogen species.
- The returning of host tissues into the homeostatic state requires the repair and remodeling of the local environment. The activated macrophages are responsible for tasks like promoting extracellular matrix remodeling, cell growth, angiogenesis, and collagen production.
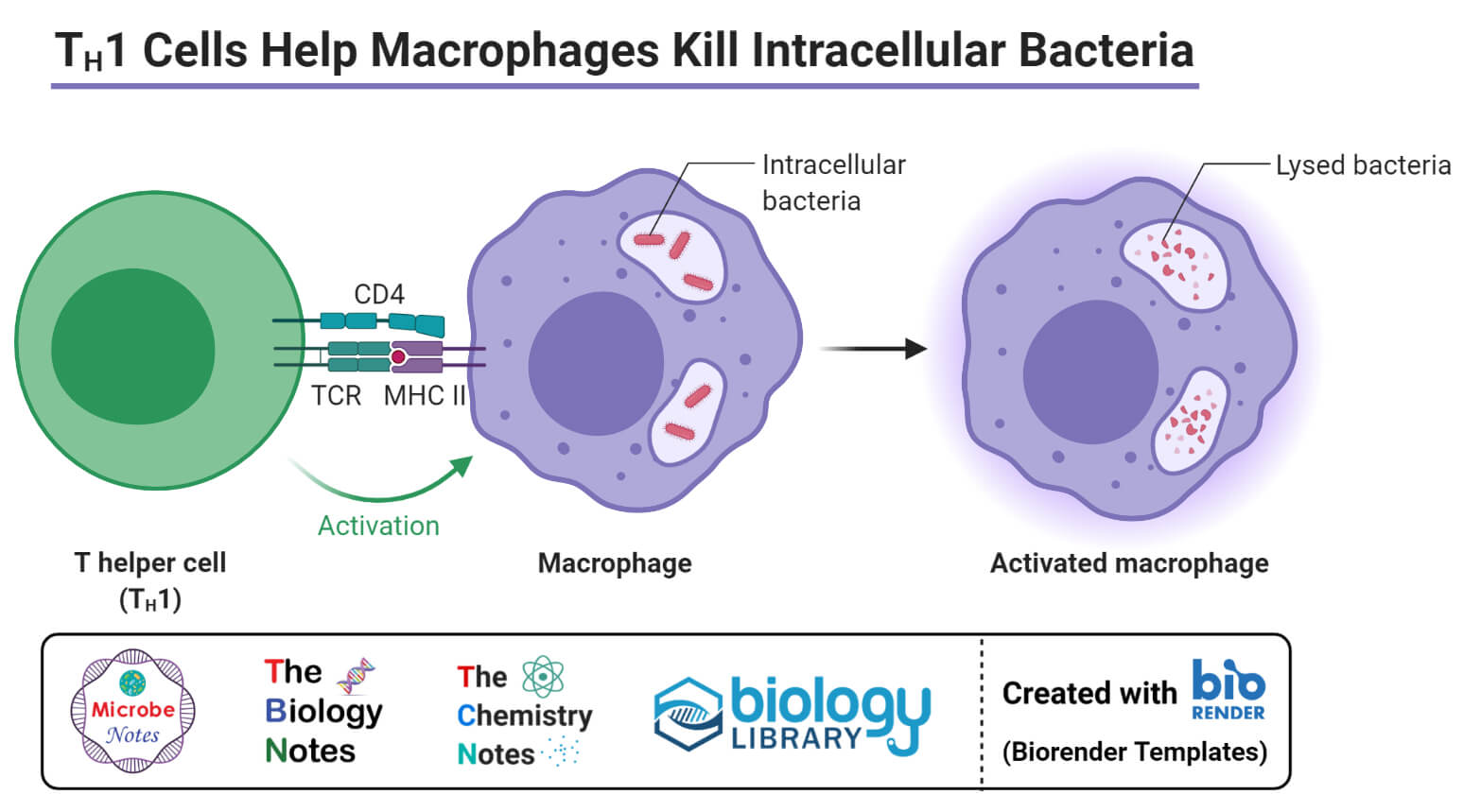
4. Adaptive Stimulation
- Adaptive stimulation of T lymphocytes is also a mechanism of immune response of macrophages as these cells provide a means to generate antigenic peptide sequences.
- These peptides are presented to T cells to bind to the cell-surface MHC class II receptors.
- The stimulation of macrophages, when coupled with additional signaling of IL-12 or IL-4, will lead to the expansion of antigen-specific T lymphocytes.
- However, the adaptive stimulation of macrophages is more limited than other innate immune cells like dendritic cells, as these can only stimulate the expansion of activated T lymphocytes.
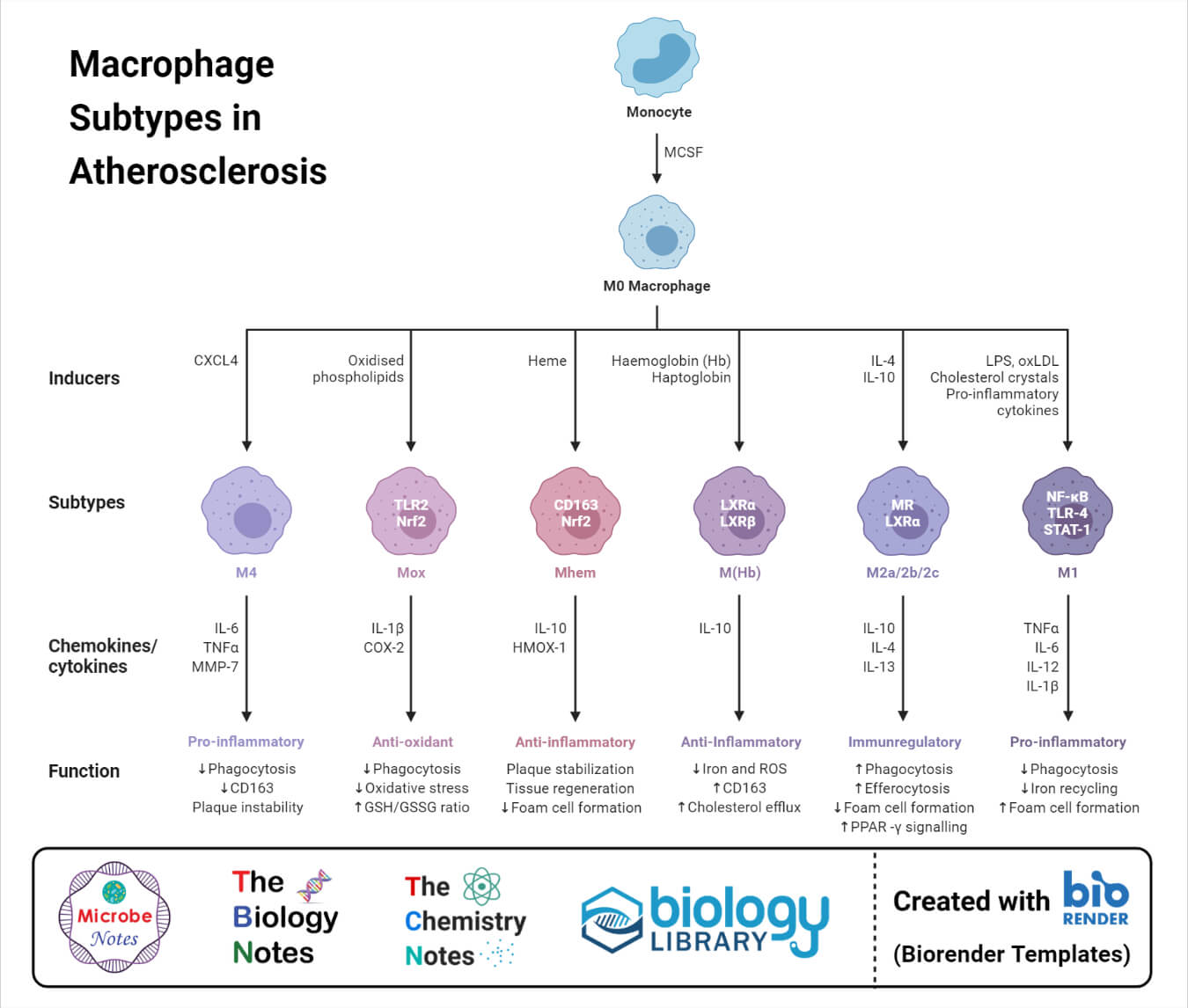
Types of Macrophages
Macrophages can be classified into one of the two opposing phenotypes; classically activated or M1 macrophages and alternatively activated or M2 macrophages. Macrophages are also of different types depending on the type of tissue they are found on. The classification is based on the activation phenotype of recruited macrophages which, in turn, depends on the surrounding microenvironment.
1. Classically activated macrophages or M1 macrophages
- Macrophages stimulated with a toll-like receptor in the presence of interferon-γ result in the formation of M1 macrophages.
- These macrophages have an enhanced capacity to present antigen, produce nitric oxide and secrete a large number of chemokines,
- These macrophages are essential in defense against bacteria which can be damaging to the host as a result of collateral damage brought about by the defense mechanisms they utilize.
2. Alternatively-activated macrophages or M2 macrophages
- Macrophages activated as a result of exposure to IL-4, IL-3 produced by CD4+ T cells from the alternatively activated macrophages or M2 macrophages.
- These macrophages are usually produced in the response to parasites and fungi. These express high amounts of cytosolic arginase and extracellular matrix-related proteins.
- M2 macrophages have the ability to limit inflammation and also play an essential role in tissue repair and wound healing.
Differentiation of monocyte into a tissue macrophage involves several changes as follows:
- The cell enlarges 5–10 folds.
- Its intracellular organelles increase in number and complexity.
- It acquires increased phagocytic ability.
- It produces higher levels of hydrolytic enzymes.
- It begins to secrete a variety of soluble factors.
Macrophages Examples
- Alveolar macrophages in the lung.
- Histiocytes in connective tissues.
- Kupffer cells in the liver
- Mesangial cells in the kidney.
- Microglial cells in the brain.
- Osteoclasts in the bone.
For their participation in the immune reaction, the macrophages need to be stimulated and reach an “activated state.” Macrophages can be activated by various cytokines, components of the bacterial cell wall, and mediators of the inflammatory response. Gamma interferon produced by helper T cells is a potent activator of macrophages and is secreted by various cells in response to appropriate stimuli. Bacterial lipopolysaccharides (endotoxin), bacterial peptidoglycan, and bacterial DNA are the substances that also activate macrophages.
Activated macrophages are more potent than normal macrophages in many ways, such as having greater phagocytic ability and increased ability to kill ingested microbes. They are better APCs, and they activate T-cell response in a more effective manner. By secreting various cytotoxic proteins, they help in eliminating a broad range of pathogens, including virus-infected cells, tumor cells, and intracellular bacteria.
Functions of Macrophages
The following are some of the functions of macrophages;
- Macrophages are phagocytes involved in the removal of dead cells and cellular debris as a part of homeostasis. Phagocytosis is one of the principal mechanisms involved in innate immunity.
- Macrophages also present antigens to other immune cells as a part of initiating an immune response. These also secrete different chemokines and a wide variety of powerful substances that influence the activation of cells of adaptive immunity.
- Macrophages are also involved muscle repair, growth, and regeneration after the inflammation of different sites.
- M2 macrophages are also called wound healing macrophages as these limit the extent of the inflammation and allow tissue repair and regeneration.
- Since macrophages are scavengers, they continuously remove dead erythrocytes from blood. The process results in the storage of iron released during the process in the form of ferritin, thus playing a role in iron homeostasis.
References
- Peter J. Delves, Seamus J. Martin, Dennis R. Burton, and Ivan M. Roitt(2017). Roitt’s Essential Immunology, Thirteenth Edition. John Wiley & Sons, Ltd.
- Judith A. Owen, Jenni Punt, Sharon A. Stranford (2013). Kuby Immunology. Seventh Edition. W. H. Freeman and Company.
- Shibata Y., Abiko Y., Takiguchi H. (1991) Macrophage Membrane: Structure and Function. In: Harris J.R. (eds) Megakaryocytes, Platelets, Macrophages, and Eosinophils. Blood Cell Biochemistry, vol 2. Springer, Boston, MA. https://doi.org/10.1007/978-1-4757-9531-8_8
- Wynn, Thomas A, and Kevin M Vannella. “Macrophages in Tissue Repair, Regeneration, and Fibrosis.” Immunity vol. 44,3 (2016): 450-462. doi:10.1016/j.immuni.2016.02.015
- Gordon, Siamon, and Luisa Martinez-Pomares. “Physiological roles of macrophages.” Pflugers Archiv : European journal of physiology vol. 469,3-4 (2017): 365-374. doi:10.1007/s00424-017-1945-7
- Wynn, Thomas A et al. “Macrophage biology in development, homeostasis and disease.” Nature vol. 496,7446 (2013): 445-55. doi:10.1038/nature12034
- Verschoor CP, Puchta A, Bowdish DM. The macrophage. Methods Mol Biol. 2012;844:139-56. DOI: 10.1007/978-1-61779-527-5_10. PMID: 22262440.
- Epelman, Slava et al. “Origin and functions of tissue macrophages.” Immunity vol. 41,1 (2014): 21-35. doi:10.1016/j.immuni.2014.06.013.

Had very painfully left elbow I’m left handed retired carpenter had 2 ultrasound cortisone injections without much improvement,3years ago was diagnosed with liver cirrhosis caused by methotrexate for arthritis,my elbow is 99% ok my liver is functioning well my question is does my immune system contain contain macrophage
How do macrophages crawl between tissues?