Interesting Science Videos
What is Salmonella?
Salmonella is one of the major food-borne pathogens that cause systemic or enteric infection affecting approximately 2 million people worldwide each year.
The first organism, Salmonella choleraesuis was isolated from a pig intestine by a scientist named Dr. Daniel Salmon.
Salmonella belongs to a member of the Enterobacteriaceae family and only two species of Salmonella namely S. enterica and S. bongori are pathogenic and cause illness to humans.
What is Salmonellosis?
Salmonellosis is a serious disease that has a clinical spectrum of gastroenteritis and typhoid fever.
S. Typhi and S. Paratyphi A is responsible for causing typhoid fever and is usually common in South and Southeast Asia.
S. Typhimurium and S. enteritidis are non-typhoidal Salmonellae and cause invasive bacterial disease most common in sub-Saharan Africa.
The fatality rate of Salmonellosis is less than 1% but malnourished children, immunocompromised patients, adults with HIV are at high risk.
Salmonella Characteristics
- Gram-negative bacteria
- Facultative anaerobes
- Motile, rod-shaped bacteria
- Non-spore former
- Non-capsulated (except S. Typhi and S. Paratyphi)
- Growth temperature ranges from 5 to 45°C (Optimum temperature – 35 to 37°C)
- Broad pH range 3.8 to 9.5
- Resists bile salts
- Produces H2S
Sources of transmission of Salmonellosis
- Poultry is the major reservoir of Salmonella and is transmitted to other organisms through the fecal-oral route.
- Salmonella species are also present in the GI tract of many animals, birds and reptiles.
- Salmonella was first isolated from the intestine of turkey flocks and chicken broiler flocks.
- The water and foods get contaminated from the feces and/or urine of the infected humans or animals.
- Consuming contaminated water and food infects the healthy individual and cause infections.
- The person-to-person also get infected through fecal-oral transmission and/or by handling contaminated food products or utensils and poor hygiene practices.
- Consuming tropical fish from contaminated water, raw meats, eggs, milk and milk products, salad dressing, cake desserts and topping, cocoa, peanut butter and chocolate are the possible source of Salmonella infection.
Epidemiology of Salmonellosis
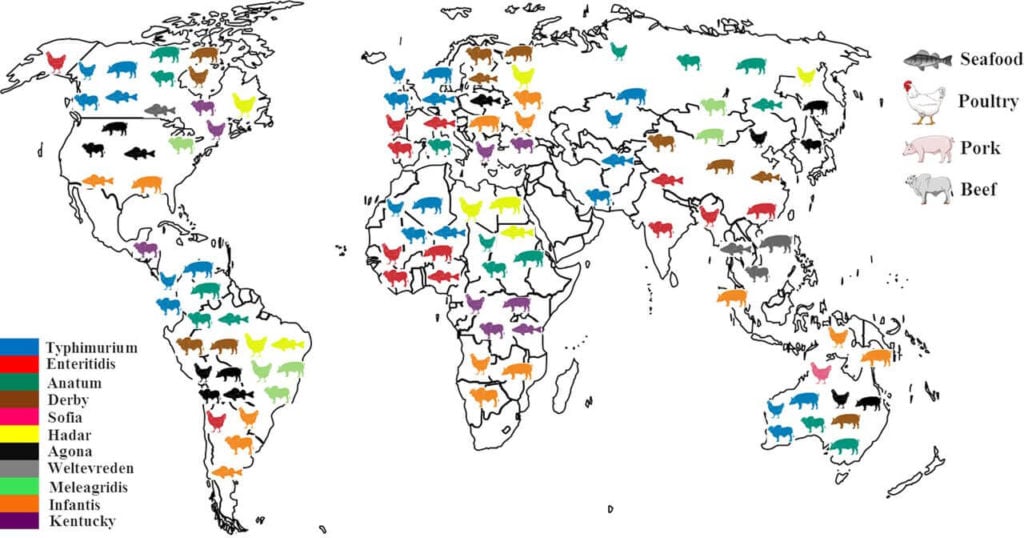
- Salmonella infection has been reported since the 19th century and is still encountered 2 million cases every year.
- The major cause of enteric fever is S. Typhi but in Asia, S. Paratyphi A is the main cause of enteric fever.
- S. Enteritidis and S. Typhimurium are the major strains that cause bloodstream infections in parts of sub-Saharan Africa whereas, in England and Wales, S. Typhi and S. Paratyphi cause systemic infection.
- The major typhoid fever outbreak occurred in 2000, with 21.7 million cases and 217,000 deaths.
- According to the Center for Disease Control and Prevention, more than 1.2 million Salmonella cases with 23,000 patients hospitalized and 450 deaths are reported each year in the US.
- A total of 258 cases were reported in the outbreak from the District of Columbia with 32 hospitalized but no deaths occurred.
- A frozen raw yellowfin tuna product was the source of the outbreak from the investigation of the federal public health agencies.
- In the US, from the consumption of peanuts and peanut products more than 714 people were infected and 9 died in this outbreak.
- Following the investigation, they traced that peanuts and peanut products were used in more than 200 companies as a foodstuff to make brownies, cakes, pies, cookie products, prepackaged meals, snacks and pet foods.
- In Australia, an outbreak occurred with sea turtle meat and contaminated tap water; in the US with frozen meals and in Canada it was headcheese.
Pathogenesis of Salmonellosis
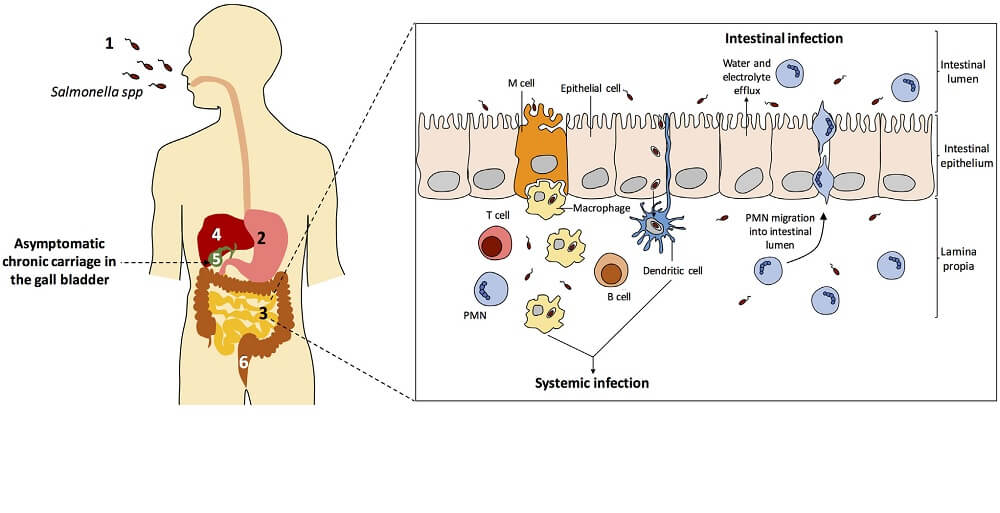
- For an organism cell to cause infection, 106 to 109 cfu/gm of viable cells must be ingested.
- After the ingestion of bacterial cells, the organism must survive a host defensive barriers such as salivary bactericidal enzymes, the hydrochloric acid of the stomach, lysozymes, bile salts, intestinal proteases and gut microflora.
- The use of oral antacids and antibiotics decreases the gut microbiome which facilitates the growth of Salmonella.
- Many factors are determined for the Salmonella to invade inside the epithelial cells that include the Type III secretion system, fimbriae, flagellin and bacterial DNA.
- The pathogen attaches to the epithelial cells within Payer’s patches with the help of fimbriae.
- Then endocytosis occurs where the pathogen gets engulfed by the cells and passes through epithelial cells within a membrane-bound vacuole.
- They multiply in the vacuoles and releases into the mucous membrane and the inflammatory cells and toxins are produced which releases prostaglandins.
- The enterotoxin produced by Salmonella activates the adenylate cyclase that stimulates intestinal secretion.
- In systemic enteric fever, the macrophages take up the invaded bacteria to the mesenteric lymph nodes where the organism multiplies and enters the bloodstream causing bacteremia.
Clinical manifestations of Salmonellosis
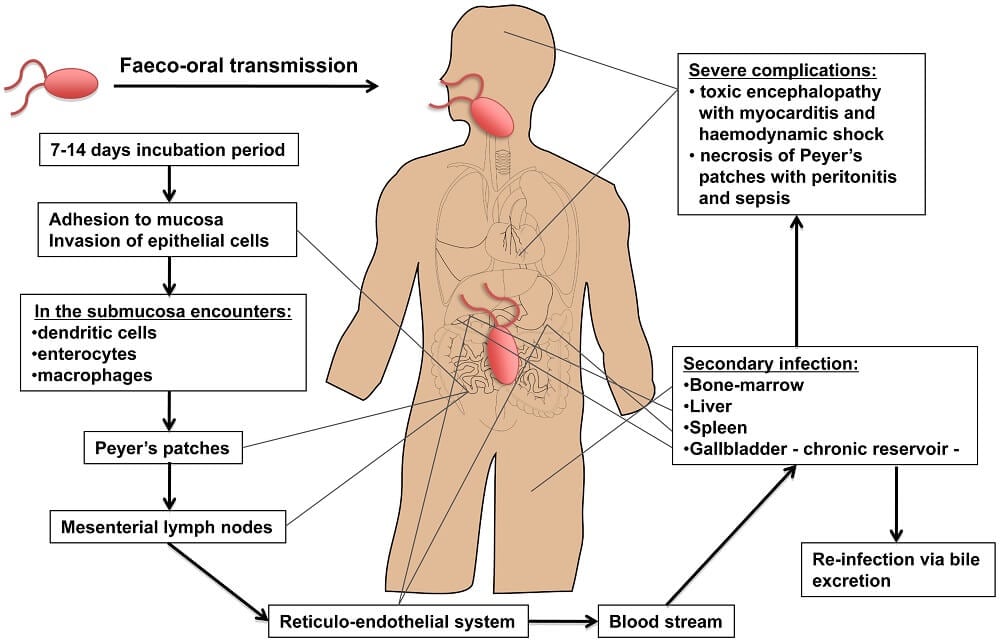
- The process of Salmonellosis starts after 6 to 48 hours of ingestion in case of gastroenteritis (food poisoning).
- The incubation period depends on the dose of bacterial cells ingested from contaminated food and water.
- Common symptoms of gastroenteritis are nausea, vomiting, diarrhea, abdominal cramp, myalgia, headache, fever and chills.
- The infection lasts only for 2 to 7 days and is self-limiting.
- In the case of enteric fever i.e, typhoid fever, the complication begins after 10 to 14 days of ingestion of bacterial cells.
- The symptoms are non-specific at the first week of infection with constipation, headache and mild fever.
- In the second week, the patient starts to develop myalgia, continuous high fever, severe headache, abdominal distension, watery diarrhea and sometimes foul green-yellow stools.
- If untreated, patients may die from toxemia, myocarditis and intestinal hemorrhage.
Laboratory Diagnosis of Salmonellosis
1. Culture method
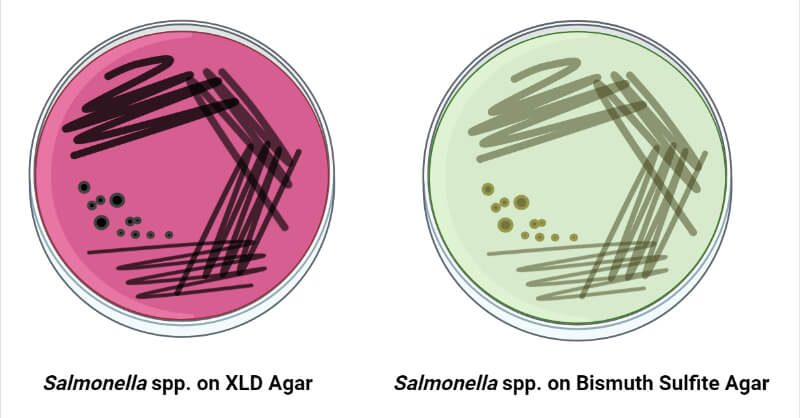
- The commonly used lab media for the isolation of Salmonella species are Desoxycholate Citrate Agar or XLD agar, Salmonella – Shigella agar and MacConkey agar.
- If the sample is minimum, enrichment media are used such as tetrathionate or selenite F broth.
2. Serology test
- Widal agglutination test is done which measures the antibodies against the antigens of the pathogen.
- It is determined against the somatic (O) and flagellar (H) antigens of the organism.
- High somatic (O) antibody titre specifies acute infection whereas high flagellar (H) antibody indicates enteric fever.
- But Widal test lacks specificity mostly in developing countries which may be due to cross-reaction with other pathogens.
- Now, this method has been replaced by the ELISA technique which is more specific and sensitive.
3. Blood culture for enteric fever
- Bone-marrow culture is done in case of enteric fever where the organisms are recovered from the blood clot and can be done at any stage of illness.
- The blood clot is digested using the streptokinase enzyme.
4. Molecular typing methods
- The Enteritidis or Typhimurium can be determined by phage typing or antibiotic-resistant typing.
- Specific strains of pathogens are identified by PCR-based methods, pulsed-field gel electrophoresis (PFGE) and plasmid typing.
Treatment and Control of Salmonellosis
- Antibiotics are not recommended for Salmonella entero-colitis but in case of enteric fever and typhoid fever, antibiotics such as Ciprofloxacin, Azithromycin, Ceftriaxone.
- The use of antibiotics in uncomplicated cases shortens the illness but may increase the antibiotic-resistant strains.
- Typhoid vaccines are recommended for travelers but the vaccine is ineffective against S. Paratyphi A, B and C.
- The major reservoir is the poultry and livestock therefore, to prevent the infection removing the Salmonella-infected animals, changing the slaughtering methods, maintaining good hygiene practices during processing and protecting processed foods from cross-contamination.
- Consume properly cooked foods, pasteurized milk and milk products and refrigerate foods at an adequate temperature in terms of storage are the preventive measures recommended.
References
- Bintsis, T. (2017). Foodborne pathogens. AIMS Microbiology, 3(3), 529–563.
- Feasey, N. A., & Gordon, M. A. (2014). Salmonella Infections. Manson’s Tropical Infectious Diseases, 337–348.e2.
- Hernandez, J. A., Long, M. T., Traub-Dargatz, J. L., & Besser, T. E. (2014). Salmonellosis. Equine Infectious Diseases, 321–333.e4.
- Salmonellosis. (2013). Clinical Veterinary Advisor, 726–729.
- Chart, H. (2012). Salmonella. Medical Microbiology, 265–274.
- Dawoud, T. M., Shi, Z., Kwon, Y. M., & Ricke, S. C. (2017). Overview of Salmonellosis and Food-borne Salmonella. Producing Safe Eggs, 113–138.
- De Cesare, A. (2018). Salmonella in Foods: A Reemerging Problem. Advances in Food and Nutrition Research, 137–179.
- Urdaneta V, Casadesús J. Interactions between Bacteria and Bile Salts in the Gastrointestinal and Hepatobiliary Tracts. Front Med (Lausanne). 2017;4:163. Published 2017 Oct 3. doi:10.3389/fmed.2017.00163.
- de Jong HK, Parry CM, van der Poll T, Wiersinga WJ. Host-pathogen interaction in invasive Salmonellosis. PLoS Pathog. 2012;8(10):e1002933. doi:10.1371/journal.ppat.1002933.
- Ferrari RG, Rosario DKA, Cunha-Neto A, Mano SB, Figueiredo EES, Conte-Junior CA. Worldwide Epidemiology of Salmonella Serovars in Animal-Based Foods: a Meta-analysis. Appl Environ Microbiol. 2019;85(14):e00591-19. Published 2019 Jul 1. doi:10.1128/AEM.00591-19
- https://www.ncbi.nlm.nih.gov/books/NBK8435/
