Entamoeba histolytica is a microscopic one-celled intestinal protozoan parasite that infects the large intestine and causes amoebic dysentery or amoebiasis, leading to increase mucus production, diarrhea, bleeding, and intestinal ulcers.
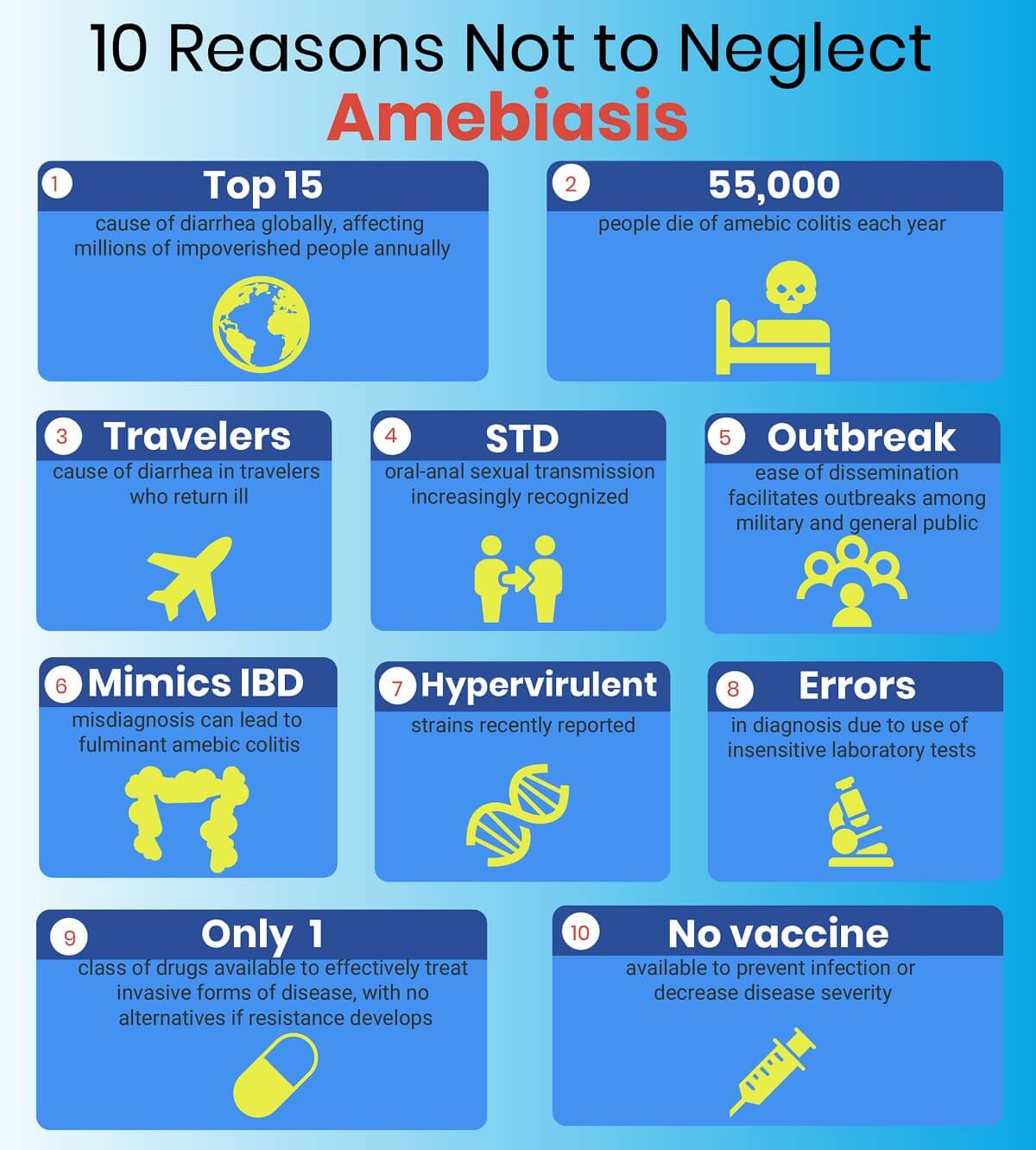
Amoebiasis causes major death worldwide, infecting 30 – 50 million people yearly by amoebic colitis or extraintestinal infection.
Many amoebae inhabit human gastrointestinal tract such as Dientamoeba fragilis, Entamoeba histolytica, Entamoeba coli, Entamoeba dispar, Entamoeba gingivalis, Entamoeba hartmanni, Entamoeba moshkovskii, Entamoeba polecki, Chilomastix mesnili, Endolimax nana and Iodamoeba butschlii.
These amoebae are commensal and do not cause harm to the host, but some amoebae, such as D. fragilis and E. histolytica, are human pathogens.
The infection of amoebiasis is high in developing and underdeveloped countries. It is also the third leading parasite that causes 100,000 deaths annually, which is due to low socioeconomic status and poor hygienic practices.
Interesting Science Videos
Characteristics of Entamoeba histolytica
- pseudopod-forming anaerobic protozoan parasite.
- actively motile by crawling or gliding.
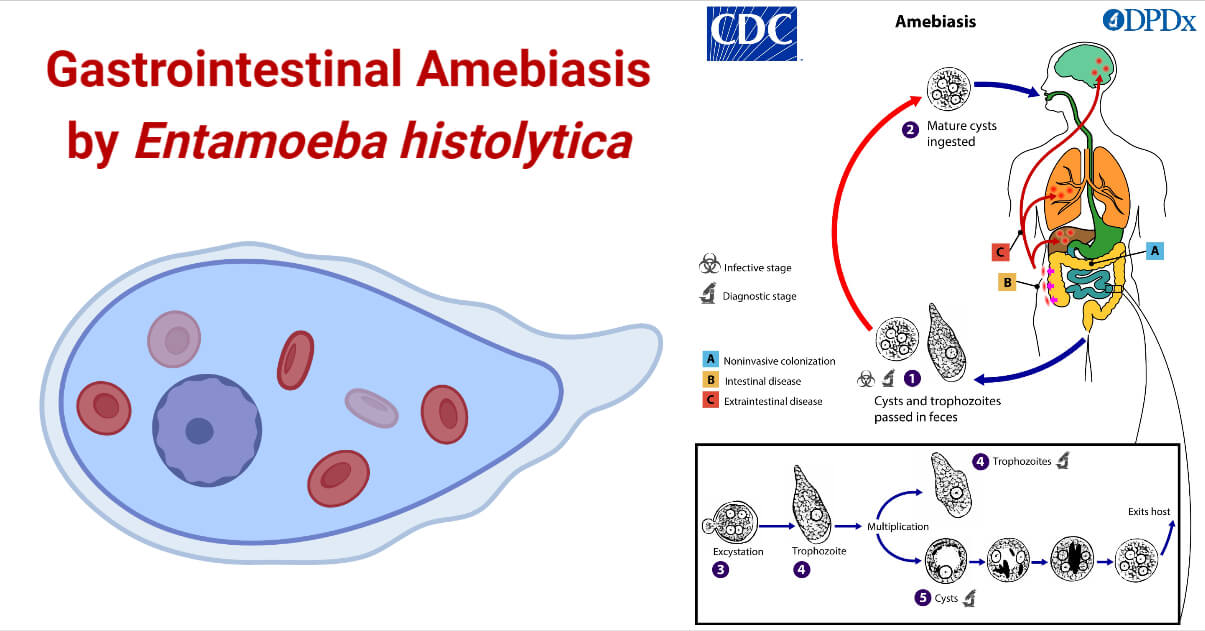
- exist in three forms: Trophozoite, Precyst, and Cyst.
- forms cysts of diameter 10 – 16 µm when immature with a single nucleus and, after maturation forms four nuclei.
- cysts can survive in soil, water, and especially moist foods.
- divided by binary fission.
- sensitive to drying, heat, and chemical sterilization.
- at low temperatures, pseudopodia formation and motility are inhibited.
- The diameter size of trophozoites is 10 – 50 µm with a single nucleus.
Sources of contamination of Amebiasis
- The most common source of contamination is ingesting contaminated food and water by human feces.
- It is also transmitted indirectly through the objects or hands through anal-oral contact.
- At a certain level, cysts are resistant to chlorine used in drinking water, making it ineffective.
- Poor socio-economic conditions and sanitation are the major cause of endemic illness in developing countries such as India, Africa, and parts of Central and South America.
- Migrants and travelers to endemic areas are also the main cause of parasitic infection in the United States.
- Another common spreading cause of the disease is through asymptomatic carriers, especially food handlers.
- Consumption of food crops and aquatic animals that are irrigated with fecally contaminated water is also a route of transmission.
- Sexual transmission among homosexuals has also been reported.
Pathogenesis of Amebiasis
- The infection starts within 2 hours when 2000 – 4000 cysts are produced in the human after ingestion.
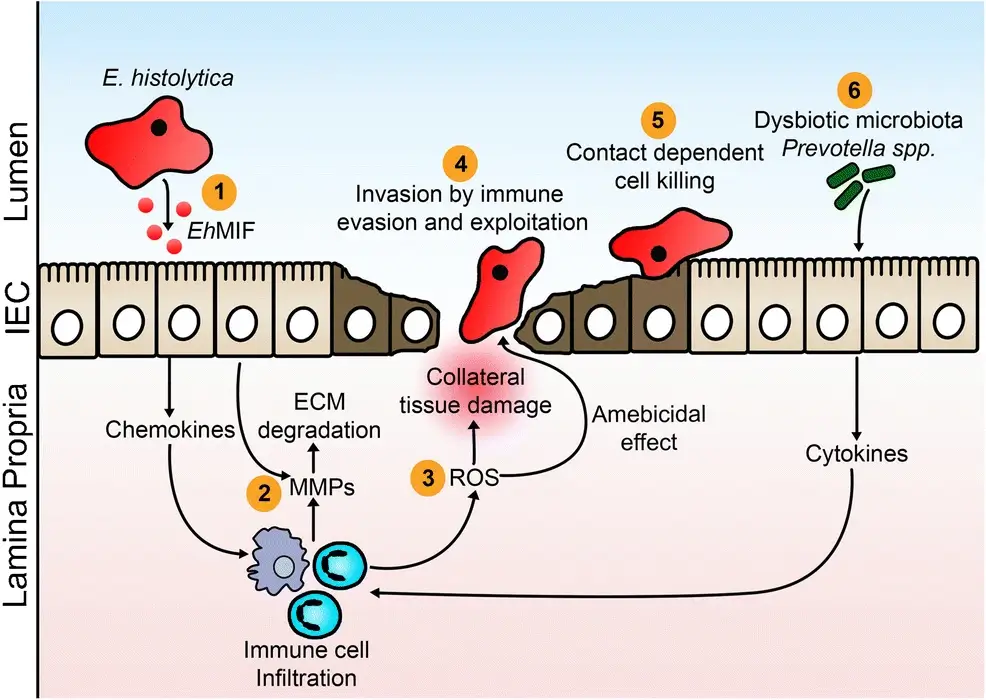
- E. histolytica infection disrupts the protective mucus coat of the stomach and detaches the enterocytes.
- It then penetrates the lamina propria and lyses the cells secreting pro-inflammatory molecules such as interleukin 1 beta, interleukin 6, 8, interferon-gamma, and tumor necrosis factor (TNF) and causes inflammation within 4 hours.
- The virulence of this parasite is attributed to its capacity to destroy the host tissues by the secretion of various molecules.
- Anchored glycoconjugates, present at the surface of the parasitic cells, are involved in the interaction of host and parasite.
- The damage to the intestinal epithelial cells is caused by the interaction between polymorphonuclear leucocytes i.e., neutrophils and lymphocytes, and trophozoites of E. histolytica.
- It degrades the DNA and mitochondria of the host and leads to apoptosis of the cells.
- In liver abscesses, a strong inflammatory response damages the liver cells. Similarly, in amebic hepatic abscess, the monocyte locomotion inhibitory factor is responsible for delayed inflammation.
- Three main virulence protein factors, Gal-lectin, cysteine proteinase, and amebapores, are involved in pathogenesis.
Epidemiology of Amebiasis
- Amoebic dysentery is the third most common parasitic infection and a leading cause of mortality and morbidity worldwide, mainly found in migrants and travelers.
- It was not described until 1875 when Fedor Losch isolated the organism from the stool of a farmer in Russia.
- Infection is common in developing countries due to a lack of personal hygiene and poor water supply and is often misdiagnosed due to the unavailability of laboratory facilities.
- According to WHO, the mortality rate is over 50,000 to 100,000 deaths related to amebiasis worldwide every year.
- Nutritional status is probably the main cause of the increased mortality rate.
- Patients with acute amebic dysentery range from 2.2% to 16%, causing invasive intestinal amebiasis.
- An outbreak occurred in three hotels by the food handlers in the early twentieth century in Chicago.
- The waterborne outbreak occurred in 1934 and 1950 when there was direct contamination of drinking water with fecal-contaminated wastewater.
- Sexual transmission has also been reported as a cause of an outbreak.
Clinical manifestation of Amebiasis
- Almost 80% of the E. histolytica infection is asymptomatic and can persist in the colon for a long period causing a risk of infection to others.
- After two to four weeks of infection, symptoms in intestinal amoebiasis normally occur, causing profuse diarrhea, mild fever, abdominal pain, and cramps.
- Sometimes intestinal amoebiasis can be chronic, causing vague gastrointestinal distress, blood and mucus diarrhea, severe ulceration of colonic mucosal surfaces, and obstruction of the intestine due to trophozoite masses can be seen rarely.
- Symptoms can vary according to the host-derived factor and stage of the parasite.
- Invasive trophozoite infection causes amoebic dysentery, a severe form of amoebiasis that causes diarrhea, stomach pain, weight loss, fever, and chills.
- Amoebic dysentery is the development of amoebic abscesses in extraintestinal tissue when trophozoites invade the intestinal wall and disseminates via the bloodstream.
- Most commonly infected extraintestinal organ infections are liver and brain abscesses, peritonitis, pleuropulmonary abscesses, and cutaneous and genital amoebic lesions.
- Hepatic amoebiasis is one of the most common complications when trophozoites are transferred in the blood from the intestinal mucosa.
- Fever, weakness, abdominal swelling, nausea, jaundice, cough, and upper-right quadrant pain are the symptoms that may persist for several weeks.
Laboratory Diagnosis of Amebiasis
- Initial diagnosis of cysts and trophozoites is done by microscopic examination of stool samples in developing and developed countries.
- Other samples, such as aspirates from the intestine, biopsy material, and mucus from rectal ulcers, can be used for observation.
- Trophozoite identification can also be done by saline wet mount preparation and/or Wheatley’s trichrome.
- To detect cysts, specimens are stained with iodine.
- An examination of a triplicate sample must be taken for three days as the organism excretion can vary daily.
- Microscopic examination cannot differentiate E. histolytica, E. dispar, or E. moshkovskii species; therefore, antigenic and molecular detection must be performed.
- Serologic testing can be done as antibodies against E. histolytica are detectable within 5 – 7 days of acute infection but is less sensitive for liver abscess.
- TechLab antigen testing has proven useful for detecting amoebic liver abscesses in liver pus, stool, and sera.
- Real-time PCR is recommended for detecting pathogenic organisms in liver abscess pus.
- For intestinal amebiasis diagnosis, sigmoidoscopy or colonoscopy are used in large bowel examinations.
- For extraintestinal diagnosis, organisms are supplemented by radiography.
- Pleuropulmonary disease, cardiac disease, and CNS can be detected by X-ray, echocardiogram, and MRI.
Treatment of Amebiasis
- Asymptomatic intestinal infection can be treated with the administration of paromomycin or diloxanide furoate.
- Intestinal and extraintestinal infections can be treated with metronidazole or another 5 – nitroimidazole.
- For amoebic liver abscesses, therapeutic aspiration is recommended unless the patient shows no improvement with oral therapy.
- Broad-spectrum antibiotics are recommended in case of fulminant colitis or abscess drainage.
Prevention and control measures of Amebiasis
- Conventional drinking water treatment should be implemented, such as sedimentation, coagulation, filtration, and use of disinfectants.
- Heat treatment of food at 68°C for 5 minutes kills cysts, so properly heat the food before consuming.
- Using human feces as a fertilizer in crops is one of the main causes of infection. Therefore, fruits and vegetables must be cleaned and cooked properly, and disinfectants must be used.
- Travelers should be careful while traveling to an endemic region by avoiding undercooked food and untreated water.
- Cysts resist chlorine, so food and water must be heated above 68°C or using iodine at 200ppm.
- Asymptomatic carriers shed millions of cysts per day for years, so people with amoebic infections should be prohibited from food preparation and handling.
References
- Nichols, G.L. (2014). Encyclopedia of Food Safety || Protozoa: Entamoeba histolytica. 31–36.
- Smith, H. (2009). Parasites: Cryptosporidium, Giardia, Cyclospora, Entamoeba histolytica, Toxoplasma gondii and pathogenic free-living amoebae (Acanthamoeba spp. and Naegleria fowleri) as foodborne pathogens. Foodborne Pathogens (Second edition). Hazards, Risk Analysis and Control. Woodhead Publishing Series in Food Science, Technology and Nutrition. 2009, Pages 930-1008.
- Chalmers, Rachel M. (2014). Microbiology of Waterborne Diseases || Entamoeba histolytica. 355–373.
- Royer, T.L. (2014). Encyclopedia of Food Microbiology || WATERBORNE PARASITES | Entamoeba. 782–786.
- Ghosh, S., Padalia, J. & Moonah, S. Tissue Destruction Caused by Entamoeba histolytica Parasite: Cell Death, Inflammation, Invasion, and the Gut Microbiome. Curr Clin Micro Rpt 6, 51–57 (2019). https://doi.org/10.1007/s40588-019-0113-6
