Hypersensitivity is increased reactivity or increased sensitivity by the animal body to an antigen to which it has been previously exposed.
The term is often used as a synonym for allergy, which describes a state of altered reactivity to an antigen.
Hypersensitivity has been divided into categories based upon whether it can be passively transferred by antibodies or by specifically immune lymphoid cells.
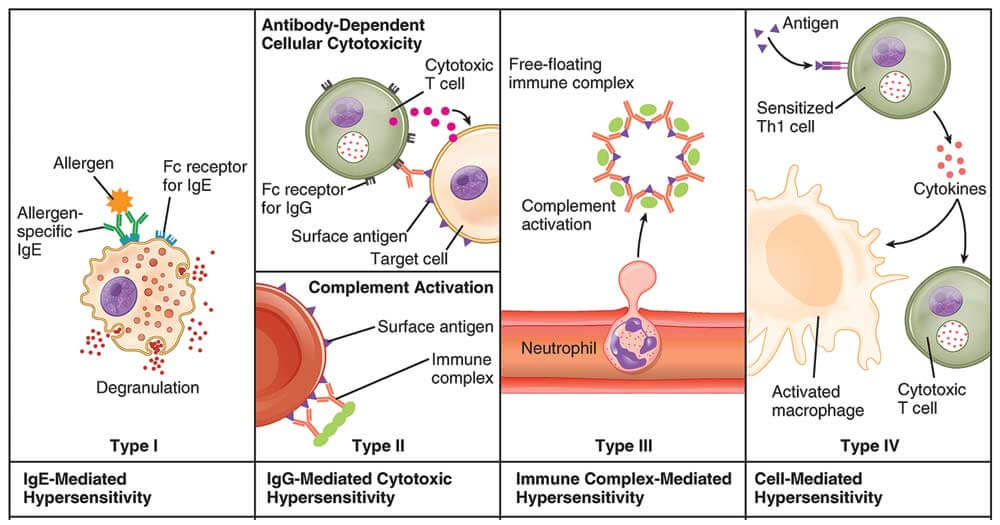
The most widely adopted current classification is that of Coombs and Gell which designates immunoglobulin-mediated (immediate) hypersensitivity reactions as types I, II, and III, and lymphoid cell-mediated (delayed-type) hypersensitivity/cell-mediated immunity as a type IV reaction.
“Hypersensitivity” generally represents the “dark side,” signifying the undesirable aspects of an immune reaction, whereas the term “immunity” implies a desirable effect.
A hypersensitive response (HR) is an anti-pathogen response in plants produced by avr-R system activation that leads to alterations in Ca+ flux, MAPK activation, and NO and ROI formation.
There is rapid necrosis of plant cells in contact with the pathogen.
This process prevents spread of the pathogen and releases hydrolytic enzymes that facilitate injury to the pathogen’s structural integrity.
Interesting Science Videos
Causes of Hypersensitivity
Immune responses that are the cause of hypersensitivity diseases may be specific for antigens from different
sources:
- Autoimmunity: reactions against self antigens.
- Reactions against microbes.
- Reactions against non-microbial environmental antigens.
Mechanism of Hypersensitivity
Hypersensitivity diseases are commonly classified according to the type of immune response and the effector
mechanism responsible for cell and tissue injury. These mechanisms include some that are predominantly dependent on antibodies and others predominantly dependent on T cells, although a role for both humoral and cell-mediated immunity is often found in many hypersensitivity diseases.
Immediate (type I) hypersensitivity
It is caused by IgE antibodies specific for environmental antigens and is the most prevalent type of hypersensitivity disease. Immediate hypersensitivity diseases, commonly grouped under allergy or atopy, are often caused by activation of interleukin-4 (IL-4), IL-5, and IL-13 producing Th2 cells and the production of IgE antibodies, which activate mast cells and eosinophils and induce inflammation.
Antibody-mediated (type II) hypersensitivity
IgG and IgM antibodies specific for cell surface or extracellular matrix antigens can cause tissue injury by activating the complement system, by recruiting inflammatory cells, and by interfering with normal cellular functions.
Immune complex-mediated (type III) hypersensitivity
IgM and IgG antibodies specific for soluble antigens in the blood form complexes with the antigens, and the immune complexes may deposit in blood vessel walls in various tissues, causing inflammation, thrombosis, and tissue injury.
T cell-mediated (type IV) hypersensitivity
In these disorders, tissue injury may be due to T lymphocytes that induce inflammation or directly kill target cells. In most of these diseases, the major mechanism involves the activation of CD4+ helper T cells, which secrete cytokines that promote inflammation and activate leukocytes, mainly neutrophils and macrophages. CTLs contribute to tissue injury in some diseases.
Types of Hypersensitivity Reactions
The Gell’s and Coombs’ classification of hypersensitivity reactions considers four types of reactions. Type I, II, and III reactions are basically mediated by antibodies with or without participation of the complement system; type IV reactions are cell-mediated. While in many pathological processes mechanisms classified in more than one of these types of hypersensitivity reactions may be operative, the subdivision of hypersensitivity states into four broad types aids considerably in the understanding of their pathogenesis.
Hypersensitivity Type I, II, III and IV- Summary in table form
Alternative Name
| Type I | Type II | Type III | Type IV |
| Allergic hypersensitivity | Cytotoxic hypersensitivity | Immune complex hypersensitivity | Cell-mediated hypersensitivity/ Delayed type of hypersensitivity |
Principle
| Type I | Type II | Type III | Type IV |
| Antibody-mediated degranulation of granulocytes leads to the destruction of cells. | Antibody-mediated destruction of healthy cells. | Antigen-antibody complex-mediated destruction of cells. | T lymphocytes mediated the destruction of cells. |
Primary Mediator
| Type I | Type II | Type III | Type IV |
| IgE | IgG/IgM | IgG/IgM | Specific subsets of CD4+ helper T cells or CD8+ cytotoxic T cells. |
Other components as mediators
| Type I | Type II | Type III | Type IV |
| Mast cells, Basophils, histamine & other pharmacological agents | Complement, Neutrophils | Complement, phagocytes and K cells | Dendritic cells, macrophages, and cytokines |
Reaction time
| Type I | Type II | Type III | Type IV |
| Immediate or within a few hours | 5-8 hours | 2-8 hours | After 24 hours only, mostly 48-72 hours after contact |
Antigen
| Type I | Type II | Type III | Type IV |
| Free in circulation (Soluble) | Fixed on cells | Free in circulation ( Soluble) | Soluble or cell-bound |
Antigen origin
| Type I | Type II | Type III | Type IV |
| Exogenous | Endogenous or exogenous | Exogenous or endogenous | Exogenous or endogenous |
Antibody
| Type I | Type II | Type III | Type IV |
| Fixed on mast cells and basophils | Free in circulation | Free in circulation | Not applicable |
Mechanism
| Type I | Type II | Type III | Type IV |
| Allergen-specific IgE antibodies bind to mast cells via their Fc receptor. When the specific allergen binds to the IgE, cross-linking of IgE induces degranulation of mast cells. | IgG or IgM antibody binds to a cellular antigen, leading to complement activation and cell lysis. IgG can also mediate ADCC with cytotoxic T cells, natural killer cells, macrophages, and neutrophils. | Antigen-antibody complexes are deposited in tissues. Complement activation provides inflammatory mediators and recruits neutrophils. Enzymes released from neutrophils damage tissue. | Th2 cells secrete cytokines, which activate macrophages and cytotoxic T cells. |
Complement activation
| Type I | Type II | Type III | Type IV |
| No | Yes | Yes | No |
Appearance
| Type I | Type II | Type III | Type IV |
| Weal & flare | Lysis & necrosis | Erythema & edema | Erythema & induration |
Transfer with serum
| Type I | Type II | Type III | Type IV |
| Passive transfer possible with serum | Passive transfer | Passive transfer | Cannot be transferred with serum; but possible with T cells transfer |
Desensitization
| Type I | Type II | Type III | Type IV |
| Easy but short-lived | Easy but short-lived | Easy but short-lived | Difficult but long-lived. |
Examples
| Type I | Type II | Type III | Type IV |
| Asthma, Rhinitis, Atopic eczema, Bee sting reaction | Rhesus incompatibility (Rh hemolytic disease), Transfusion Reactions, Cell Destruction due to autoantigens, Drug-Induced Hemolytic Anemia | Glomerulonephritis, Systemic Lupus Erythematosus, Farmer’s lung arthritis, Vasculitis | The tuberculin reaction, Granuloma formation, Allergic contact dermatitis, Type-1 diabetes |
Hypersensitivity Type I: Immediate Reaction
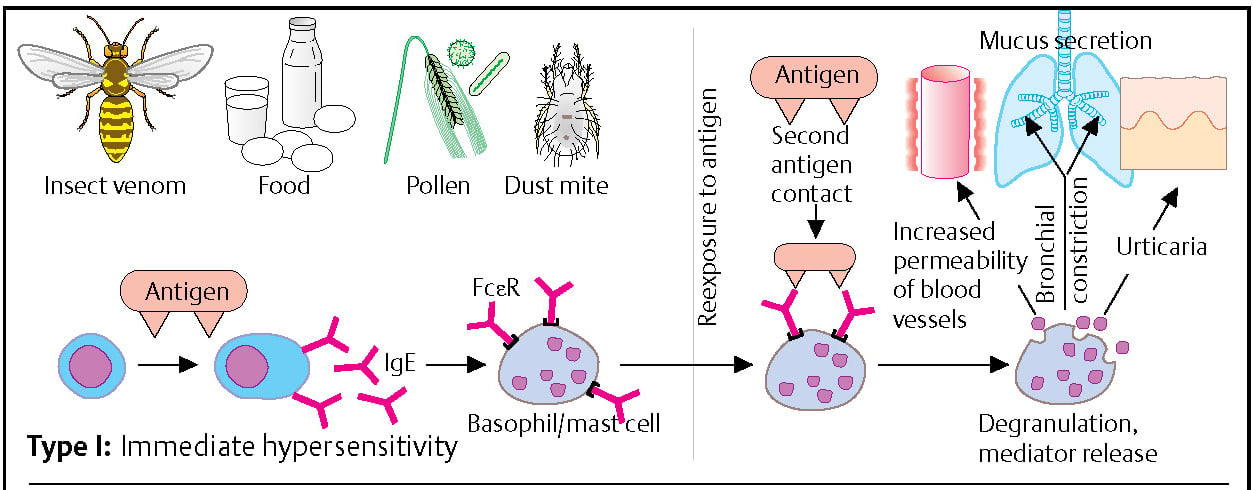
Some antigens (allergens), such as insect venom, foods, pollen, and dust mite, can induce the formation of IgE antibodies in individuals with a corresponding predisposition. The IgE antibodies bind via Fc receptors to mast cells (sensitization). If the individual is re-exposed to the allergen, cross-linkage of the membrane-bound IgE occurs. This results in the immediate release of mediators (e.g., histamine, kininogen), which induce vasodilation, smooth muscle contraction, mucus secretion, edema, and/or skin blisters. Most allergens are small proteins that can easily diffuse through the skin or mucosa. They are frequently proteases and are active at very low doses. IL-4 favors the differentiation of TH2 cells. The exact mechanism that leads B cells to produce IgE is not known.
The allergen stimulates the induction of CD4+T cells. These T cells secrete cytokines that cause IgE production by plasma cells.
The IgE molecule will bind to the Fc receptor on mast cells and basophils which in turn causes vasodilation increased vascular permeability and vascular spasm. this type may occur as a systemic or local reaction:
- systemic reactions: skin erythema, followed by respiratory difficulty due to bronchial constriction.
- local reactions: generally on the skin or mucosal surface at the site of Ag exposure. Allergy to penicillin, Aspergillus spores, rupture of Echinococcus cyst.
Hypersensitivity Type II: Antibody-mediated cytotoxic reaction
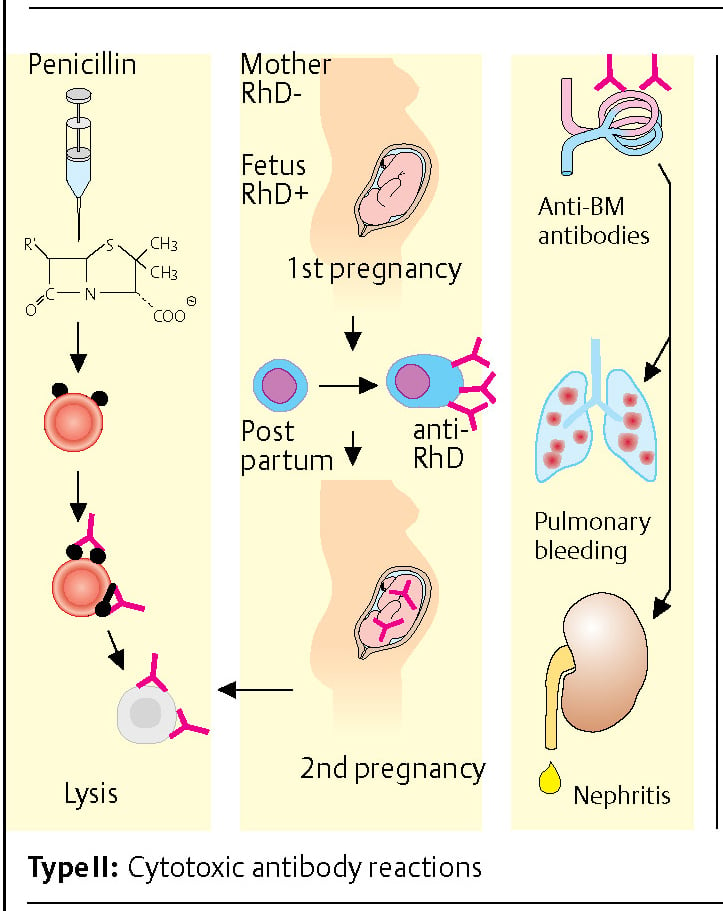
The immunization of individuals to erythrocyte antigens during pregnancy is a typical example of a type II reaction. Children who inherit the RhD erythrocyte antigen from their father can induce immunization against the RhD+ antigen in their RhD-mother. Sensitization usually occurs at birth when fetal blood cells come into contact with the maternal immune system. In any subsequent pregnancies, maternal anti-RhD antibodies of the IgG type can pass into the placenta and cause severe hemolysis of fetal RhD+ erythrocytes.
Other examples: Drugs (e.g., penicillin) can passively bind to erythrocytes. Antibodies directed against penicillin then lead to lysis of the erythrocytes. The formation of antibodies directed against the basement membrane (BM) of the glomerulus can develop during the course of kidney inflammation. Lung damage accompanied by pulmonary hemorrhage and renal inflammation (glomerulonephritis) may occur due to cross-reaction of these antibodies with the basement membrane of the lung (Good-pasture’s syndrome).
In this type Ab are formed against target Ag that are cell membrane components. Not really hypersensitivity, but cytotoxic reactions:
A) Complement-mediated
- Ab reacts with cell surface Ag leading to fixation of the complement system and then cell lysis. eg. red cells are the most common cells damaged by this mechanism>>>HEMOLYTIC ANEMIA NO MICROBES!
B) many cell types (macrophages, neutrophils, NK cells) cause lysis of target cell coated by IgG
- Poststreptococcal rheumatic fever: molecular mimicry: Antibodies produced against S. pyogenes cross-react with various tissue eg. heart, joints – inflammation
- Oncocerca worm infection may lead to blindness because of the cross-reaction of Ab produced against pathogens and proteins of the retina.
C) Antibody-mediated cellular dysfunction
- In some cases Ab is directed against cell surface receptor impairing the function but not cause cell injury>>>MYASTHENIA GRAVIS; Ab reacts with ACh receptors on the motor endplate.
Hypersensitivity Type III: Immune complex-mediated reaction
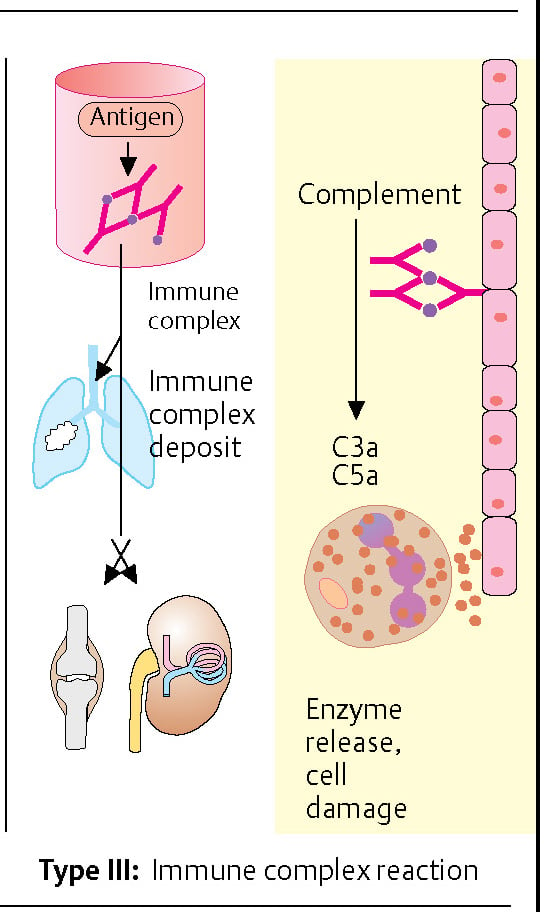
Antibody-antigen complexes (immune complexes) can form during an immune response. Immune complexes can settle in vessel walls, the basement membrane of the lungs and/or kidneys, and in the joints (synovia). They can induce inflammatory processes in these structures by binding complement factors C3a and C5a (anaphylatoxins). A particular type III reaction is the Arthus reaction: when an antigen has penetrated the skin of an individual who has preformed IgG antibodies, the immune complexes can bind to Fc receptors of most cells inducing degranulation inflammatory cells are recruited and complement is activated, leading to the release of C5a and local inflammation, platelet accumulation, and eventually to blood vessel occlusion with necrosis.
This type is mediated by ag-ab complexes which initiate an inflammatory reaction in the tissue. there are 2 patterns of immune-complex mediated injury:
A) SYSTEMIC DISEASE (serum sickness serum sickness type, SLE)
- This is because of a large excess of Ab and immune complexes are deposited at the site of injury especially within the vessel wall, the subsequent events will result in necrotizing vasculitides and accumulation of neutrophils>>>SLE
B) LOCAL DISEASE (Arthus reaction)
- Arthus reaction: intraductal injection of antigens to a personalized person may lead to local intradermal Ab – Ag complex formation and local vasculitis, redness, swelling.
- Example: Repeated (booster) vaccination with diphtheria or tetanus rarely leads to local vasculitis.
- Poststreptococcal acute Poststreptococcal acute glomerulonephritis glomerulonephritis glomerulonephritis: Ab-ag complexes deposit in glomeruli HBV infection: HBsAg-Ab complexes may HBV also cause acute glomerulonephritis
Hypersensitivity Type IV: Delayed-type hypersensitivity reaction
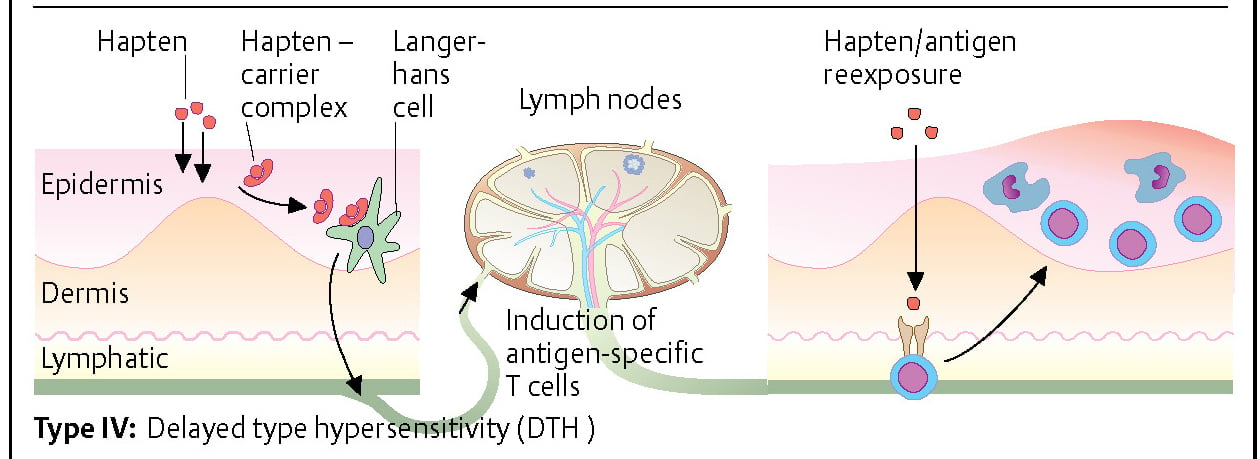
Haptens are molecules of very small molecular weight (often < 1 kDa). They are too small to function as antigens, but they can penetrate the epidermis and bind to certain proteins in the skin (carrier proteins). Hapten-carrier complexes are bound by antigen-presenting cells of the skin (Langerhans cells), which then migrate to regional lymph nodes. T-cell stimulation then occurs at the lymph node. The so-called sensitization phase lasts ca. 10-14 days. If the individual is reexposed to the hapten, antigen-specific T cells migrate to the skin, where they accumulate and proliferate. They also cause edema formation and local inflammation with the help of cytokines. Compounds containing nickel or chrome and chemicals such as those found in rubber are typical triggers of type IV hypersensitivity reactions.
This is mediated by T-cells. There are 2 types that involve CD4/8+T Cells.
A) Acute (within 2-3 days)
- Tuberculin test, contact dermatitis: mediated by CD4+ T helper cells cd4+ cells recognize ag (tuberculin), this leads to the formation of sensitized cd4+ cells.
- Upon cutaneous injection into previously sensitized individual sensitized cd4+cells become activated and secrete cytokines.
- Tuberculin/Mantoux Tuberculin/Mantoux Mantoux test test test: intradermal injection of tuberculin = purified tuberculoprotein leads to swelling after 48- 72 h if the patient has been exposed to Mycobacterium tuberculosis previously.
- Important: BCG vaccination? Yes/No!
B) Chronic (> 1 week)
- Granuloma formation, graft rejection: mediated by cd8+ cytotoxic T cell.
- lymphocytes surrounding epitheloid cells lead to the formation of granuloma.
References
- Lydyard, P.M., Whelan,A.,& Fanger,M.W. (2005).Immunology (2 ed.).London: BIOS Scientific Publishers.
- Owen, J. A., Punt, J., & Stranford, S. A. (2013). Kuby Immunology (7 ed.). New York: W.H. Freeman and Company.
- 4% – http://semmelweis.hu/mikrobiologia/files/2014/05/hypersensitivity.pdf
- 2% – https://basicmedicalkey.com/streptococcus-enterococcus-and-similar-organisms/
- 1% – https://www.researchgate.net/publication/16984737_Immune_complexes_Characteristics_clinical_correlations_and_interpretive_approaches_in_the_clinical_laboratory
- 1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3597223/
- 1% – https://quizlet.com/228679925/week-vi-flash-cards/
- 1% – https://quizlet.com/12054435/cytokines-flash-cards/
- 1% – https://en.wikipedia.org/wiki/Red_blood_cell
- 1% – http://site.iugaza.edu.ps/asilmi/files/2017/09/14.pptx
- https://courses.lumenlearning.com/microbiology/chapter/hypersensitivities/
- http://www.biologydiscussion.com/immunology/4-main-types-of-hypersensitivity-immunology/61851
- https://www.slideshare.net/drsomeshwaranamsana/hypersensitivity-reactions-dr-somesh-microbiology
- http://www.yourarticlelibrary.com/immunology/type-iii-hypersensitivity-and-its-mechanism-human-immunology/28081

Good content of hypersensitivity
this is an amazing note about hypersensitive
Ofcourse I acknowledged to say this is amazing notes. Can u tell me if I want to expert in immunology what are basics books that I need to have with me to know all the sufficient topics