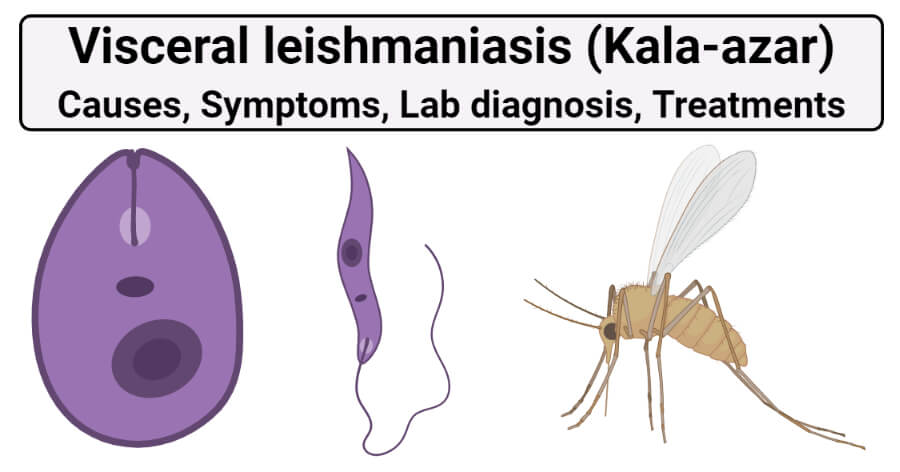
Visceral leishmaniasis is sometimes known as systemic leishmaniasis or kala-azar. Kala-azar also is known as black fever or Dumdum fever in Asia.
It usually occurs 3 to 6 months after being bitten by a sandfly. It primarily infects the reticuloendothelial system. It damages internal organs, such as the spleen and liver. It also affects bone marrow, as well as the immune system through damage to these organs. It is the most severe form of the disease and, left untreated, is usually fatal. Annually an estimated 50 000 to 90 000 new cases of VL occur worldwide with only between 25 to 45% reported to WHO. It remains one of the top parasitic diseases with outbreak and mortality potential. This disease is the second-largest parasitic killer in the world (after malaria), responsible for an estimated 20,000 to 30,000 deaths each year worldwide.
Post-Kala-Azar Dermal Leishmaniasis (PKDL)
Post-kala-azar dermal leishmaniasis (PKDL) is usually a consequence of visceral leishmaniasis that may appear after 1 month or years after the treatment of visceral leishmaniasis. In this leishmaniasis, parasites invade the skin and develop macular, papular, or nodular rash usually on the face, upper arms, trunks, and other parts of the body. 5-10% of kala-azar patients are reported to develop this PkDL. It occurs mainly in East Africa and on the Indian subcontinent.PKDL is not-life threatening but still considered a potential source of Leishmania infection.
Interesting Science Videos
Causes of Visceral leishmaniasis (Kala-azar)
- It is caused by Leishmania donovani (India and Eastern Africa), L. infantum (Mediterranean area), and L. chagasi, which is transmitted by the bite of small blood-sucking sandflies Phlebotomus, and Sergentomyia, common vectors of the Old World.
- The sandfly species notorious for spreading New World disease is Lutzomyia.
- Sandflies are very small insects, about one-third the size of a small mosquito or < 3.5 mm in length.
- They cannot withstand the dehydration and therefore develop well in moist climates.
- These flies are nocturnal, and during the day are found in burrows and under rocks or other shelters.
- Males and females both obtain carbohydrates from plant juices, females require a blood meal. It is during this meal that the vector fly transmits the protozoa to the human host.
Symptoms of Visceral leishmaniasis (Kala-azar)
- The incubation period is from 3 to 6 months and symptoms may appear even after 2years.
- The at-risk population includes preschool children and immunocompromised and undernourished individuals.
- Recently, visceral leishmaniasis frequency increases in patients who have AIDS or who are intravenous drug users or both, through contaminated syringes
Symptoms include:
Early symptoms include
- weight loss,
- weakness, fever that lasts for weeks or months,
- enlarged spleen,
- Anemia due to a decrease in the production of blood cells,
- bleeding,
- a peculiar darkening of the skin
- swollen lymph nodes.
In the advanced stage,
- skin becomes dry, rough, and dark or pigmented. Hair becomes brittles and fall out.
- usually fatal if untreated,
Lab diagnosis of Visceral leishmaniasis (Kala-azar)
Lab diagnosis of Kala-azar depends upon direct and indirect evidence.
Direct evidence
1. Microscopy
Samples:
- The demonstration of amastigotes in smears of tissue aspirates is the gold standard for the diagnosis of visceral leishmaniasis.
- Peripheral blood sample,
- a biopsy from the bone marrow: obtained by sternal or iliac crest puncture.
- splenic aspirates: biopsy material: obtained by a splenic puncture.
- enlarged lymph node
- The smears of aspirates are stained with Leishman, Giemsa, or Wright’s stain for the detection of amastigote forms of the parasite through microscopy.
- For an accurate diagnosis of leishmaniasis, amastigotes should be visualized by light microscopy under oil immersion.
- Amastigote parasites can be seen within the macrophages often in large numbers. A few extracellular forms can also
be seen. - Buffy coat of peripheral blood can be utilized to look for the parasite microscopically. Buffy coat smears show a diurnal periodicity, more smears being positive when collected during the day than at night.
- Splenic aspiration, although incurring a risk of hemorrhage, is the most sensitive means (95%) for diagnosing leishmaniasis.
- Bone marrow biopsy demonstrates amastigotes in approximately two-thirds of patients.
- Lymph node aspirates are not useful in the diagnosis of Indian kala-azar, although it is employed in VL in some other countries.
- Although the specificity is high, the sensitivity of microscopy varies, being higher for spleen (93% to 99%) than for bone marrow (53-86%) or lymph nodes aspirates (53-65%).
- It is the classic confirmatory test for visceral leishmaniasis.
2. Culture
- Different samples of blood, splenic, or bone marrow aspirates, tissues are cultured on an NNN medium.
- The material is inoculated into the water of condensation and the culture is incubated at 22- 24°C for 1-4 weeks. At the end of each
week, a drop of culture fluid is examined for promastigotes under high power objective or phase contrast illumination. - Motile promastigotes can be demonstrated microscopically in a few days to 4 weeks in a positive culture.
- Another biphasic medium, like Schneider’s drosophila tissue culture medium with an added 30% fetal calf serum can also be used.
3. Animal inoculation
- It is a very sensitive method.
- It is not used for routine diagnosis.
- In this method, the material is inoculated intraperitoneally or intradermally into the skin of the nose and feet of the Chinese golden hamster, and they are kept at 23- 26°C.
- In positive cases, the amastigote can be demonstrated in smears taken from ulcers or nodules developing at the sites of inoculation or from the spleen.
Indirect evidence
1. Detection of antigen
- The concentration of antigen in the serum or other body fluids is very low.
- ELISA and PCR have been developed for the detection of leishmanial antigens.
- Two non-invasive antigen detection test in urine for VL are under evaluation.
- It showed good specificity but only low to moderate (48-87%) sensitivity.
2. Detection of antibodies
a. Complement fixation test was the first serological test used to detect serum antibodies in VL.
Specific leishmanial antigens prepared from cultures have been used in a number of tests to demonstrate specific antibodies. These tests include:
b. Indirect immunofluorescent antibody test (IFAT)
c. Counter immunoelectrophoresis (CIEP)
d. ELISA or Western Blot using whole parasite lysate, have shown high diagnostic accuracy in most studies but are poorly adapted for field settings. The ELISA assay is highly sensitive (80-100%) but the specificity varies with the antigen used, from 80-94% with whole parasite lysate.
Two tests that are sufficiently validated and used under field are:
e. Direct agglutination test
- Widely used serological test for diagnosis of kala-azar and based on antigen-antibody reaction.
- Antigen used- trypsin treated, stained and formalin preserved promastigotes.
- Positive reaction – agglutination with specific antibodies from VL positive patient
- Test setting– room temperature
- The usefulness is limited by their variable sensitivity or specificity, the requirement of electricity, a refrigerator, or a well-equipped lab, and high cost.
- The DAT assay has been found to be 91-100% sensitive and 72-100% specific in various studies.
f. rk 39immunochromatographic
- It is a specific, rapid, and noninvasive test.
- The immunochromatographic test (ICT) method for antibody has been developed using a recombinant leishmanial antigen rk 39 consisting of 39 amino acids conserved in the kinesin region of L. infantum. The sensitivity of the test is 98% and specificity is 90%.
- rk 39 antibody test is more useful and easy to perform and recommended by the National Vector Borne Disease Control Programme (NVBDCP) in India.
- The result can be obtained within 5 min.
- The test is found in LCT or dipstick format, that are more suitable for field case.
3. molecular diagnosis
- DNA probe
- PCR
4. Nonspecific serum test
a. Napier’s Aldehyde test
- In this method, 1 mL of clear serum from then the patient is taken in a small test tube, a drop of formalin (40% formaldehyde) is added, shaken, and kept in a rack at room temperature. A control tube with normal serum is also set up.
- A positive reaction is a jellification and opacification of the test serum, resembling the coagulated white of egg appearing within 3-30 minutes.
- About 85% of patients with a disease of 4 months or more give a positive reaction.
- Aldehyde test is always negative in cutaneous leishmaniasis (CL).
- The sensitivity of this test is poor, as low as (34%)
- The test merely indicates greatly increased serum gamma-globulin and thus is nonspecific.
b. Chopra’s antimony test
- It is done by taking 0.2 mL of serum diluted 1:10 with distilled water in a Dreyer’s tube and overlaying with a few drops of 4% solution of urea stilbamine.
- The formation of white flocculant precipitate indicates a positive test.
- The reaction is said to be more sensitive than the aldehyde test.
- Both the tests give false-positive reactions in several other diseases such as multiple myeloma, cirrhosis of the liver, tuberculosis, leprosy, schistosomiasis, African trypanosomiasis.
5. Lelshmanin skin test (Montenegro test)
- It is a Delayed hypersensitivity test (DHT).
- This was first discovered by Montenegro in South America and hence, named after him.
- 0.1 mL of killed promastigote suspension (10^6 washed promastigotes/ mL) is injected intradermally on the dorsoventral aspect of the forearm.
- A positive result is indicated by induration and erythema of 5 mm or more after 48-72 hours.
- A positive result indicates prior exposure to the leishmanial parasite.
- The test is positive in African kala-azar but not in India and Mediterranean kala-azar.
- In the active kala-azar, this test is negative and becomes positive usually 6-8 weeks after a cure from the disease.
- DTH testing is very useful in the diagnosis of cutaneous leishmaniasis.
- It is utilized primarily as an epidemiological tool and has little role in the establishment of a diagnosis of acute VL.
6. Blood count
- Complete blood count shows normocytic normochromic anemia and thrombocytopenia.
- Leukocyte count reveals leukopenia accompanied by a relative increase of lymphocytes and monocytes.
- Eosinophil granulocytes are absent. During the course of the disease, there is a progressive diminution of leukocyte count falling to 1,000/mm3 of blood or even below that.
- The ratio of leukocyte to erythrocyte is greatly altered and maybe about 1:200 to 1:100 (normal 1:750).
- Serum shows hypergammaglobulinemia and a reversal of the albumin: globulin ratio.
- Liver function tests show mild elevations of liver
Treatments of Visceral leishmaniasis (Kala-azar)
- The decision to treat leishmaniasis depends on the clinical syndrome, the infecting Leishmania spp., the immunologic status of the host, and drug availability and cost.
- Kala-azar responds to treatment better than other forms of VL.
- The standard treatment consists of pentavalent the antimonial compound, which is the drug of choice in most of the endemic regions of the world, but there is resistance to antimony in Bihar in India, where amphotericin-Bdeoxycholate or miltefosine is preferred.
- Pentavalent antimonial compound: Two pentavalent antimonial
(Sbv) preparations are available:
1. Sodium stibogluconate
2. Meglumine antimoniate Dosages: The daily dose is 20 mg/kg by rapid intravenous (IV) infusion or intramuscular (IM) injection for 20-30 days. Cure rates exceed 90% in most of the old world, except in Bihar (India) due to resistance (cure rate 36%). - other drugs include Amphotericin-B, Liposomal amphotericin-B, Paromomycin, Millefosine.
- Prophylaxis
References and Sources
- Maxfield L, Crane JS. Leishmaniasis. [Updated 2020 Jul 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531456/.
- https://www.healthline.com/health/leishmaniasis
- Shyam Sundar, M. Rai Clinical and Diagnostic Laboratory Immunology Sep 2002, 9 (5) 951-958; DOI: 10.1128/CDLI.9.5.951-958.2002
- https://www.who.int/news-room/fact-sheets/detail/leishmaniasis.
- 2% – https://www.statpearls.com/articlelibrary/viewarticle/24181/
- 2% – https://microbeonline.com/laboratory-diagnosis-of-leishmaniasis-visceral-leishmaniasis-kala-azar-part-one/
- 1% – https://www.onlinebiologynotes.com/leishmania-donovani-morphology-life-cycle-pathogenesis-clinical-symptoms-lab-diagnosis-treatment-prevention-and-control/
- 1% – https://www.ncbi.nlm.nih.gov/pubmed/2940111
- 1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4656188/
- 1% – https://quizlet.com/128961857/leishmaniasis-flash-cards/
- 1% – https://edoc.hu-berlin.de/bitstream/handle/18452/15497/Tai.pdf?sequence=1&isAllowed=y
- <1% – https://www.sciencedirect.com/topics/medicine-and-dentistry/leishmanin-skin-test
- <1% – https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/reticuloendothelial-system
- <1% – https://www.sciencedirect.com/science/article/pii/S0735109705028020
- <1% – https://www.researchgate.net/topic/Intradermal-Injections
- <1% – https://www.researchgate.net/publication/7778372_Sensitivity_of_bone_marrow_aspirates_in_the_diagnosis_of_visceral_leishmaniasis
- <1% – https://www.researchgate.net/publication/51778984_Diagnosis_of_visceral_leishmaniasis_Developments_over_the_last_decade
- <1% – https://www.researchgate.net/publication/51064295_Do_Commercial_Serologic_Tests_for_Trypanosoma_cruzi_Infection_Detect_Mexican_Strains_in_Women_and_Newborns
- <1% – https://www.researchgate.net/publication/327086271_Leishmaniasis
- <1% – https://www.researchgate.net/publication/13664887_Use_of_PCR_for_Diagnosis_of_Post-Kala-Azar_Dermal_Leishmaniasis
- <1% – https://www.ncbi.nlm.nih.gov/pubmed/21212210
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3235892/
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2125815/
- <1% – https://www.infoplease.com/math-science/health/diseases/common-infectious-diseases-worldwide
- <1% – https://www.fishersci.com/shop/products/schneider-s-drosophila-medium/21720024
- <1% – https://link.springer.com/chapter/10.1007%2F978-3-319-74186-4_3
- <1% – https://en.wikipedia.org/wiki/Visceral_affecting_skin_leishmaniasis
- <1% – https://cvi.asm.org/content/9/5/951
- <1% – http://www.faqs.org/health/topics/46/Delayed-hypersensitivity-skin-test.html
- <1% – http://medicalfarre.in/leishmania/
