All blood cells are produced by a mechanism known as hematopoiesis, arising from a single cell type known as a hematopoietic stem cell (HSC). Stem cells are cells that differentiate into other cell types; they are self-renewing-maintaining their population level by cell division.
Interesting Science Videos
Hematopoietic Stem Cell Lineages and Growth Factors
- In humans, hematopoietic formation and development of red and white blood cells being in the embryonic yolk sac in the first week of development. The yolk-sac stem cells differentiate into primitive erythroid cells that contain embryonic hemoglobin.
- During the third month of the gestation period, the hematopoietic stem cells migrate from the yolk sac to the fetal liver and the spleen, which are the major organs from hematopoiesis from the 3rd to the 7th month of the gestation. Then the hematopoietic process of the stem cells then starts in the bone marrow until birth when there is little or no hematopoiesis in the liver and spleen.
- Therefore, every mature and specialized blood cell is derived from the same type of stem cell, a type of cell lineage known as multipotent or pluripotent hematopoietic stem cells. These are stem cells that are able to differentiate and generate various cell types including erythrocytes, granulocytes, monocytes, mast cells, lymphocytes, and megakaryocytes. However, their numbers are few (1 HSC in every 5104 cells in the bone marrow).
- Hematopoietic stem cells remain at a stable level throughout adult life and research has shown that their proliferation capacity is enormous.
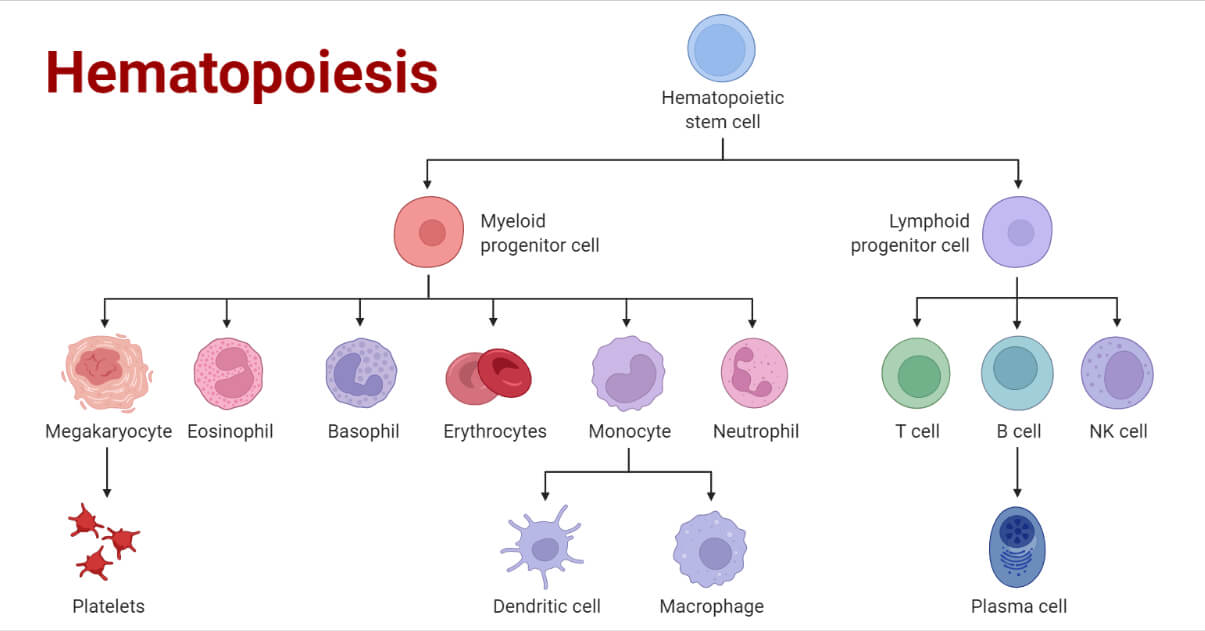
- In the early phase of hematopoiesis, the multipotent stem cells differentiate along with one of the two pathways, which gives rise to either a common lymphoid progenitor cell or a common myeloid progenitor cell, which is dictated by its microenvironment.
- During the development of the lymphoid and myeloid lineages, stem cells differentiate into progenitor cells, which have lost the capacity for self-renewal and are committed to a particular cell lineage.
- Common lymphoid progenitor cells give rise to B-cells, T-cells, NK (natural killer) cells, and some dendritic cells.
- Myeloid stem cells generate progenitors of red blood cells (erythrocytes), many of the various white blood cells (neutrophils, eosinophils, basophils, monocytes, mast cells, dendritic cells), and platelets.
- The progenitor productions are highly dependent on the acquisition of response to growth factors and cytokines, which help in the proliferation and differentiation of the progenitor cells into the corresponding cell types, which can either be a mature erythrocyte, a specific type of leukocyte, or a platelet-generating cell (megakaryocytes).
- The Red blood cells and the white blood cells pass into the bone marrow and through the circulation. Within the bone marrow, the hematopoietic cells grow and mature on a mesh of stromal cells which are non-hematopoietic cells supporting the growth and differentiation of hematopoietic cells.
- The stromal cells include fat cells, endothelial cells, fibroblasts, and macrophages, and they influence the process of hematopoietic differentiation by providing a hematopoietic-inducing microenvironment (HIM). The HIM consists of a cellular matrix and factors that promote growth and differentiation.
- The hematopoietic growth factors normally include soluble agents that arrive at their target cells by diffusion and other membrane-bound molecules on the surface of stromal cells that require cell-to-cell contact between the responding cells and the stromal cells.
- When the body has an infection or during infection, hematopoiesis is stimulated by the production of hematopoietic growth factors by activated macrophages and T-cells.
- Research on the genetic level of hematopoiesis identifies some of the growth factors involved to be transcriptional factors, that affect the hematopoietic lineages and other factors that influence a single lineage which leads to the development of lymphocytes.
- One transcription factor that affects multiple lineages is, GATA-2, a transcriptional factor that recognizes the tetranucleotide sequence GATA, a nucleotide motif in target genes. A functional GATA-2 gene, which specifies this transcription factor, is essential for the development of the lymphoid, erythroid, and myeloid lineages.
Regulation of Hematopoiesis and Programmed Cell death
- The hematopoietic process is a continuous process to maintain a steady and constant production of mature blood cells to balance production to that of loss by cell-aging. RBCs (erythrocytes) have an average life span of 120 days before it is phagocytosed and digested by spleen macrophages.
- The categories of white blood cells have a life span of few days like neutrophils, to over 20 years for some T-lymphocytes, and therefore to maintain a steady-state level, a human being must produce at least 3.7×1011 white blood cells per day.
- The regulation of hematopoiesis is done by several complex mechanisms that affect all individual cell types. These regulatory mechanisms ensure steady-state levels of the various blood cells yet they have enough built-in flexibility so that the production of blood cells can rapidly increase tenfold to twenty-fold in response to hemorrhage or infection.
- Steady-state regulation of hematopoiesis is accomplished in various ways, which include:
- Control of the levels and types of cytokines produced by bone marrow stromal cells
- The production of cytokines with hematopoietic activity by other cell types, such as activated T cells and macrophages
- The regulation of the expression of receptors for hematopoietically active cytokines in stem cells and progenitor cells
- The removal of some cells by the controlled induction of cell death
- A failure in one or a combination of these regulatory mechanisms can cause extreme abnormalities in expressing the hematopoietic cytokines or their receptors. This can lead to unregulated cell proliferation and it can contribute to the development of some types of leukemias.
- Therefore there should be a balance between the number of hematopoietic lineages production (differentiation and proliferation) and the number of cells that are removed by cell death.
- Lastly, hematopoietic cell lineages undergo programmed cell death known as apoptosis. Each of the immune cells has a specific life span after which they naturally die by what is referred to as programmed cell death. For example, the neutrophils are about 5×1010 in circulation, and they have a life span of a few days before programmed cell death is initiated. This death along with constant neutrophil production maintains a stable number of the cells.
- However, if programmed cell death occurs, a leukemic state may develop.
References
- https://www.stemcell.com/hematopoietic-stem-and-progenitor-cells-lp.html
- https://www.sciencedirect.com/topics/immunology-and-microbiology/hematopoiesis
- https://immunologysystem.blogspot.com/2016/07/hematopoietic.html
- https://ashpublications.org/blood/article/125/17/2605/34110/Hematopoietic-stem-cells-concepts-definitions-and
- https://en.wikipedia.org/wiki/Multipotent_hematopoietic_stem_cell
- https://www.bioexplorer.net/hematopoietic-stem-cells.html/

Plz give lukopoiesis notes.. Tbis notes is very useful thanks.. 🙏🙏🙏