- Human enteric viruses are the major cause of nonbacterial gastroenteritis also known as stomach flu and are transmitted via food and waterborne route.
- Foodborne viruses include the human noroviruses (HNoV), hepatitis A virus (HAV), hepatitis E virus (HEV), rotavirus (RV), Aichi virus (AiV), astroviruses, sapoviruses, adenoviruses, coxsackievirus, parvovirus, and picornavirus.
- These viruses are categorized into three types according to the disease caused by them: gastroenteritis causing viruses, fecal-orally transmitted hepatitis viruses, and illness-causing viruses.
- Astrovirus, rotavirus, the enteric adenovirus, and the enteric caliciviruses cause acute gastroenteritis in humans.
- Hepatitis viruses such as HAV and HEV are transmitted through the fecal-oral route and cause liver inflammation whereas enteroviruses cause other illnesses such as diarrhea, vomiting, abdominal pain, and fever.
- Viral outbreak and their associated illnesses have been a major problem globally affecting the health of exposed individuals and also affecting their economy for treatment.
- Foodborne viruses are a major concern in the food industry although they are obligate parasites they can remain infective in food and water for over a month and even more.
- They cannot proliferate in food during processing and storage but their low infectious dose can cause a risk to the consumer.
- Most reported viral outbreaks are caused by infected food handlers and through the process from farm to fork which has not gone heating process.
Interesting Science Videos
Sources of Contamination
- The main source of contamination is through the food and water route mainly by the infected food handlers during food preparation.
- The processing and preparation of animal products harboring a zoonotic virus is the major reservoir for the contamination of consumers.
- Vectors such as mosquitoes and ticks are responsible for transferring arthropod-borne viruses.
- Other transmission ways are droplets from an infected person while coughing and sneezing, sexual intercourse, and contaminated fecal samples.
- Most common is the fecal-oral route transmission where only a few viral particles can cause illness in humans.
- Viruses do not cause spoilage of food as they cannot replicate in processed food therefore, there is a passive transfer of viruses to consumers.
- Use of fecally contaminated irrigation water for food preparation especially raw products such as salads, fruits, vegetables, and ready-to-eat food products.
- Poor hygiene during processing and handling and direct consumption of undercooked infected food products are also possible sources of contamination.
Foodborne viruses Examples
Human Noroviruses
- Noroviruses are +ve sense single-stranded RNA viruses of 23 – 40 nm diameter and 7.5 kb genome size.
- HNoVs include five major genera: Norovirus, Sapovirus, Vesivirus, Lagovirus, and Nebovirus.
- NoV has six genogroups (GI to GVI) in which GI, GII, and GIV genogroups are human pathogens responsible for causing illnesses.
- Their genome consists of nonstructural proteins such as ORF1, VP1 capsid protein (ORF2), and a phosphorylated VP2 protein (ORF3).
- The majority of food-borne illnesses are caused by norovirus with self-limiting symptoms but their emerging virulent strains may cause death in an elderly and immunocompromised patient.
- After the consumption of HNoV contaminated food, it reaches the human intestine and binds to the histoblood group antigens.
- Replication occurs at the upper intestinal tract and symptoms start appearing within 24 to 48 hours and last up to a week.
- Mild gastrointestinal problems such as nausea, headache, abdominal pain and vomiting are observed.
- These viruses can survive at low pH (2 – 4) and can remain in the environment and food for a long time.
- Maintaining good hygienic practices by food handlers can prevent the transmission rate as there is no vaccine and antiviral treatment available against this infection.
- Oral and intravenous fluid therapy is recommended in case of gastroenteritis and dehydration.
Hepatitis A virus
- Hepatitis A viruses are also +ve sense single-stranded RNA virus similar to the size of human norovirus but contain only a single ORF serotype.
- The genome contains 3 structural capsid proteins VP1, VP2 and VP3 in the p1 region whereas RNA replication occurs in P2 and P3 regions.
- The incubation period of HAV is approximately 28 days long with severe symptoms of jaundice, dark urine, vomiting, fever and loss of appetite.
- HAV can resist very low pH up to 1.0 therefore it has high infectivity in the environment and can survive in harsh conditions as well.
- The pathogenic mechanism is similar to all the viruses occurring in the upper gastrointestinal tract of the human intestine.
- Vaccination is available which provides lifetime immunity but a majority of HAV infection resolves on their own.
Other viruses
Rotavirus
- Rotavirus causes infantile diarrhea in children under 5 years of age mostly in developing nations.
- Symptoms are mild and less severe like fever, abdominal pain, watery diarrhea and vomiting but last only a week.
- Dehydration is the main cause of death in young children as the infection is severe in the initial stage but later immunity develops.
- Rotavirus vaccine is recommended by the WHO but tends to be less effective because of strain diversity and resistivity.
Hepatitis E virus
- HEV is a small 32-34 sized single-stranded +ve sense RNA virus containing three ORFs (ORF1, ORF2, and ORF3) genomes.
- The ORF1 genome forms helicase, protease, and RNA polymerase similarly, ORF2 codes for capsid protein and ORF3 encodes for replication.
- Genotypes 1 and 2 of HEV are responsible for causing disease in humans while others affect swine animals.
- The incubation period is 2 to 10 weeks long with two different phases of illness.
- The first is the preicteric phase developing symptoms like fever, vomiting, anorexia, and abdominal pain which is usually mild and the icteric phase develops severe illnesses like jaundice.
- Illnesses are self-limiting as there is no specific treatment if the infection is severe, PEGylated interferon administration is recommended.
Epidemiology of Foodborne viruses
- Human norovirus (hNoVs) is the major cause of nonbacterial viral outbreaks occurring worldwide all year round being the peak in the winter.
- About 31 viral pathogens are reported of causing 9.4 million foodborne illnesses in the United States according to Centres for Disease Control and Prevention.
- Human norovirus is responsible for 58% of foodborne illnesses and an 11% fatality rate.
- The first human norovirus outbreak was reported in an elementary school in 1968, Ohio where 50% of students and teachers suffered from a gastrointestinal illness.
- The emerging virulent strains are reported of causing death in older people and immunocompromised individuals.
- The cases are higher in children but young adults are at risk of suffering from illness as asymptomatic infections are common.
- Nursing homes and hospitals are the major places of a gastroenteritis outbreaks from the consumption of norovirus contaminated food.
- Norovirus infections are widely spread but Hepatitis A virus infection is endemic and is transmitted directly from person to person.
- HAV outbreak in China led to 250,000 cases of infection in 1988 from the consumption of contaminated clams by the local people.
- The incubation period of HAV is long and problematic but outbreaks and infections are rare because of today’s increased living standards and hygienic practices.
- Rotavirus infection is also linked globally in terms of outbreak cases mainly in developing countries where such as India, Pakistan, Nigeria, and Ethiopia where the place is unhygienic and lacks proper drinking water.
- Around 450,000 cases are reported every year and about 22% of death cases occur mainly in India which is due to contaminated water.
Clinical manifestation during viral infection
- Very minimum concentration of virus particles can cause infection to humans and the major cause of transmission is shedding the particles 10 to 14 days before the appearance of symptoms.
- Infections are usually asymptomatic in the initial days but later gastroenteritis problems like nausea, vomiting, diarrhea, fever, and abdominal pain are developed.
- Viral illness is self-limiting within a few days to a week but severe illness may occur in elderly people having cardiovascular and renal disease.
- In the case of HAV infection, moderate clinical symptoms like fever, malaise, anorexia, nausea, abdominal pain, discomfort, dark urine, and jaundice are observed.
- The incubation period of HAV is longer from 15 to 50 days and does not last longer than 8 weeks but in some cases, the infected patient may show symptoms for up to 6 months.
- Chronic infection is not reported but patients with chronic liver disease may develop fulminant hepatitis.
Detection Methods of Foodborne viruses
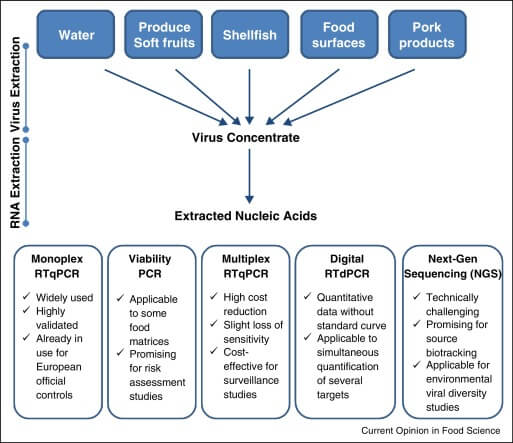
- Foodborne viruses are detected using bioassays to determine their cytopathic effect but are not applicable to human norovirus and HAV.
- Gastroenteritis infections are diagnosed using the stool sample under an electron microscope which is still the gold standard for virus detection.
- Immunological assays such as ELISA and immunoelectron microscopy are used nowadays using antibodies against the known genotypes of the viruses.
- Molecular-based detection methods are currently used as it gives valid result though the process is not simple and requires skilled manpower.
- Reverse transcription-quantitative PCR (RT-qPCR) is used for the detection of human enteric viruses from food and environmental samples.
- But the main disadvantage of this method is that it fails to provide specific infectious and non-infectious viral particles which gives a false-positive result.
References
- O’Shea, H., Blacklaws, B. A., Collins, P. J., McKillen, J., & Fitzgerald, R. (2019). Viruses Associated With Foodborne Infections. Reference Module in Life Sciences.
- D’Souza, D. H. (2015). Update on foodborne viruses: types, concentration, and sampling methods. Advances in Microbial Food Safety, 102–116.
- Baert, L. (2013). Foodborne virus inactivation by thermal and non-thermal processes. Viruses in Food and Water, 237–260.
- Maunula, L., & von Bonsdorff, C.-H. (2016). Foodborne viruses in ready-to-eat foods. Food Hygiene and Toxicology in Ready-to-Eat Foods, 51–68.
- Hoorfar, J., Schultz, A. C., Lees, D. N., & Bosch, A. (2011). Foodborne viruses: understanding the risks and developing rapid surveillance and control measures. Food Chain Integrity, 88–104.
- Koopmans, M., & Duizer, E. (2004). Foodborne viruses: an emerging problem. International Journal of Food Microbiology, 90(1), 23–41.
- D’Souza, D. H., & Joshi, S. S. (2016). Foodborne Viruses of Human Health Concern. Encyclopedia of Food and Health, 87–93.
- Manuel, C., & Jaykus, L.-A. (2014). VIRUSES | Foodborne Viruses. Encyclopedia of Food Microbiology, 732–737.
- Koopmans, M., von Bonsdorff, C.-H., Vinjé, J., de Medici, D., & Monroe, S. (2002). Foodborne viruses. FEMS Microbiology Reviews, 26(2), 187–205.
