Interesting Science Videos
What is Candida glabrata?
Candida glabrata was previously known as Torulopsis glabrata, belongs to the class of Fungi Imperfecti, the order of Moniliaes and family of Cryptococcaceae.
- C. glabrata is one of the most common candida species, living commensally in the human host.
- It does not cause disease in healthy individuals.
- However, it has been found to also cause candidiasis in persons with underlying conditions with suppressed immune functions including HIV/AIDS patients, diabetic patients, chemotherapy patients, organ transplant patients, inpatient surgery patients.
- Therefore, it is a known pathogenic candidal species responsible for candidiasis infections in weakened immune hosts.
- It prevalently causes infections of the urogenital tract, systemic infections when they gain entry into the bloodstream majorly in immunocompromised patients.
- C. glabrata currently ranks second or third as the causative agent of superficial (oral, esophageal, vaginal, or urinary) or systemic candidal infections, which are often nosocomial.
- The treatment of C. glabrata infections can include azoles, amphotericin B, or flucytosine.
Habitat of Candida glabrata
- C. glabrata is found in a wide range of environments but majorly in the human host.
- They are ubiquitous inhabitants of the gastrointestinal tracts of mammals, living as normal microflora.
- It has also been isolated from various parts of the human host body including oral cavity, genitourinary tract, alimentary tract, and respiratory tract.
Morphology of Candida glabrata
- Unlike other candidal species with are dimorphic in nature, Candida glabrata in nondimorphic, existing is small blastoconidia.
- It is the only Candidal species that do not form pseudohyphae at temperatures higher than 37°C.
- The blastoconidia of C. glabrata are very small, 1 to 4 μm are considerably smaller than Candida albicans blastoconidia, which are 4 to 6 μm.
- Isolation of colonies on Sabouraud dextrose agar, C. glabrata shows the formation of glistening, smooth, cream-colored colonies with are relatively small in size however, similar to other Candidal species.
- Isolation on Chromagar, a differential medium for Candidal species, C. glabrata produces colonies that appear pink to purple, in contrast to C. albicans colonies, which appear green to blue-green.
- They have a haploid genome with small RNA subunits, unlike other Candidal species that have a diploid genome.
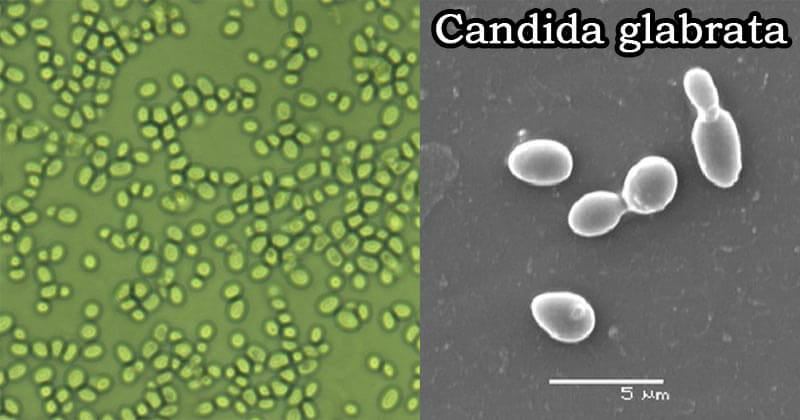
Figure: Candida glabrata – 1600x (Source: BCarver1) and Candida glabrata yeast under an electron microscope. The figure shows two single cells and two mother-daughter pairs during the budding process. Source: Khadija Mohamed Ahmad (Researchgate).
Pathogenesis of Candida glabrata
- They have very low pathogenicity but its isolation from various patient samples is an indication that it constitutes of contributing factors to its adherence, colonization, and causing candida associated infections.
- The lack of pseudohyphae formation, adhesin receptor proteins such as fibronectin, and laminin have been associated with its low virulence and pathogenicity.
- Immune defense mechanisms against Candida glabrata are minimally documented, but the role of the polymorphonuclear cells leukocytes on candidemia and systemic candidiasis caused by this species has been noted.
Virulence Factors
- Adherence Factors to the epithelial and the endothelial cells which has been associated with the cell surface hydrophobicity of the fungi, enabling it to interact with the adhesin receptors on the host cells. However, its adherence factors are equally low as compared to other Candida species.
- Protease production – Candida glabrata produces protease at minimal quantities as compared to Candida albicans
- Phenotypic switching has been detected on Candida glabrata which allows it to switch colony phenotypes without affecting the genotype of the species, which has been associated with the virulence of its virulence among other Candidal species.
Clinical Manifestations of Candida glabrata
Superficial infection
- Symptomatic mucosal infection by Candida glabrata has been detected in oropharyngeal, esophageal, and vaginal candidiasis, in HIV/AIDS patients and other immune-compromised patients.
- Oropharyngeal candidiasis is associated with acute pseudomembranous candidiasis, commonly known as oral thrush.
- It is the first sign of HIV infection, and progressive infection to AIDS, showing signs of asymptomatic erythematous forms.
- Esophageal candidiasis is associated with the disease dissemination from the oropharyngeal lining.
- Vulvovaginal candidiasis which is common in women, pregnant women, diabetic patients, associated with mild to moderately severe candidiasis.
- Urinary tract candidiasis also known as candiduria, is common in hospitalized patients with invasive catheters, diabetes mellitus patients, the elderly, and debilitated patients under antibacterial medications. However, there are no complicated hematogenous infections of the urinary tract are linked to Candida glabrata.
Systemic Candidiasis
- Candida glabrata rarely causes systemic candidiasis, however, in weakened immune patients dissemination has been found in the bloodstream especially in prolonged hospitalized patients and bone marrow transplant patients. It has been linked to long-term administration of antibacterial agents and fluconazole antifungals.
- It disseminates to other organ systems and causes blood infection known as candidemia, associated with persistent fever, deteriorating conditions, and unresponsiveness to antifungal agents.
- Fungemia is commonly caused by C. glabrata.
Laboratory Diagnosis of Candida glabrata
Specimens
Swabs, respiratory wash, vaginal swabs, blood
Staining and Microscopic Examination
KOH wet mount for identification and differentiation from other Candida species.
Cultural Examination
- On Sabouraud dextrose agar, C. glabrata forms glistening, smooth, cream-colored colonies, similar to other Candidal species, except their relatively small size.
- On Chromagar, a differential medium for Candidal species, Candida glabrata produces colonies that appear pink to purple, in contrast to C. albicans colonies, which appear green to blue-green.
- They can also be grown on bacterial blood cultures for hemolytic characteristics of the fungi.
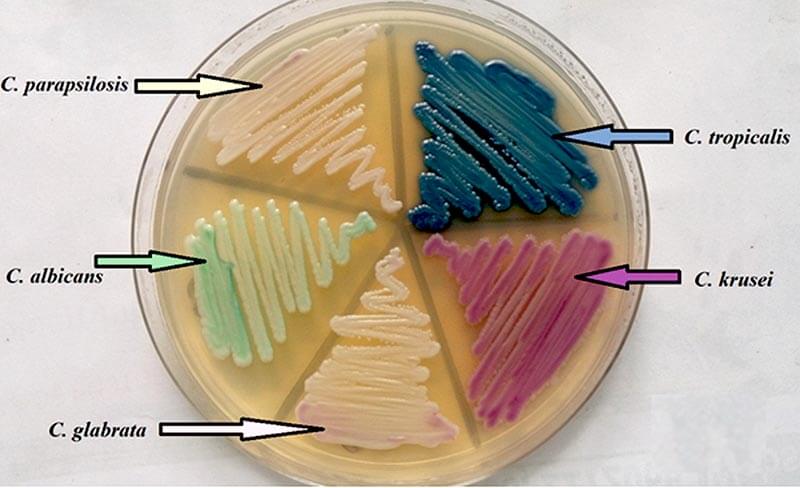
Figure: Morphology and color of yeast on Candida CHROM agar. Source: DOI : 10.7860/JCDR/2017/23578.9475.
Biochemical Tests
Candida glabrata can only ferment and assimilates glucose and trehalose, unlike other Candida species that assimilate several sugars.
Molecular Based Tests
Comparative chromosomal DNA analysis to identify and differentiate Candida species and different strains using:
- Restriction Fragment Length polymorphism
- Pulse-field Gel Electrophoresis which differentiates the chromosomal molecular weight by separating the chromosomal strands into separate bands for strain identification.
- Electrophoretic Karyotypying (EK) patterns which produce 10-13 bands for Candida glabrata strains.
- Random amplified polymorphism DNA and DNA probing.
Video: Candida glabrata Isolation (Microhub Plus)

Treatment of Candida glabrata infections
- Oropharyngeal candidiasis – topical polyene agents such as nystatin, amphotericin B and Clotrimazole, triazoles, itraconazole, and fluconazole in HIV/AIDS patients.
- Esophageal candidiasis – Oral and intravenous fluconazole, oral itraconazole, intravenous amphotericin B.
- Vulvovaginitis – Butoconazole, has excellent antifungal activity, miconazole and clotrimazole, terconazole, itraconazole, and ketoconazole show moderate activity. Fluconazole is poor for tretament of vulvovaginitis.
- Symptomatic candiduria is treated with Amphotericin B or fluconazole.
- Systemic Candidiasis – gold standard treatment for systemic candidiasis is the use of Amphotericin B including candidemia, minimal doses of fluconazole are also effective.
Prevention and Control of Candida glabrata infections
- Discontinue catheterization for patients with candiduria infection
- Prophylactic treatment with antifungal agents in hospitalized patients
References and Sources
- 8% – https://cmr.asm.org/content/12/1/80
- 1% – https://www.sciencedirect.com/topics/immunology-and-microbiology/prevotella
- 1% – https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/candida
- 1% – https://www.researchgate.net/publication/13407454_Candida_glabrata_Review_of_Epidemiology_Pathogenesis_and_Clinical_Disease_with_Comparison_toC_albicans
- 1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4019226/
- 1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2533538/
- 1% – https://www.infectiousdiseaseadvisor.com/home/decision-support-in-medicine/infectious-diseases/urinary-tract-infections-uti-pyelonephritis-complicated/
- 1% – https://wikimili.com/en/Oral_microbiology
- <1% – https://www.verywellhealth.com/disseminated-infection-3132797
- <1% – https://www.ncbi.nlm.nih.gov/pubmed/25682023
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3218701/
- <1% – https://thehealthtalks.com/candidiasis-types-causes-treatment/
- <1% – https://courses.lumenlearning.com/microbiology/chapter/introduction-to-urogenital-system-infections/
