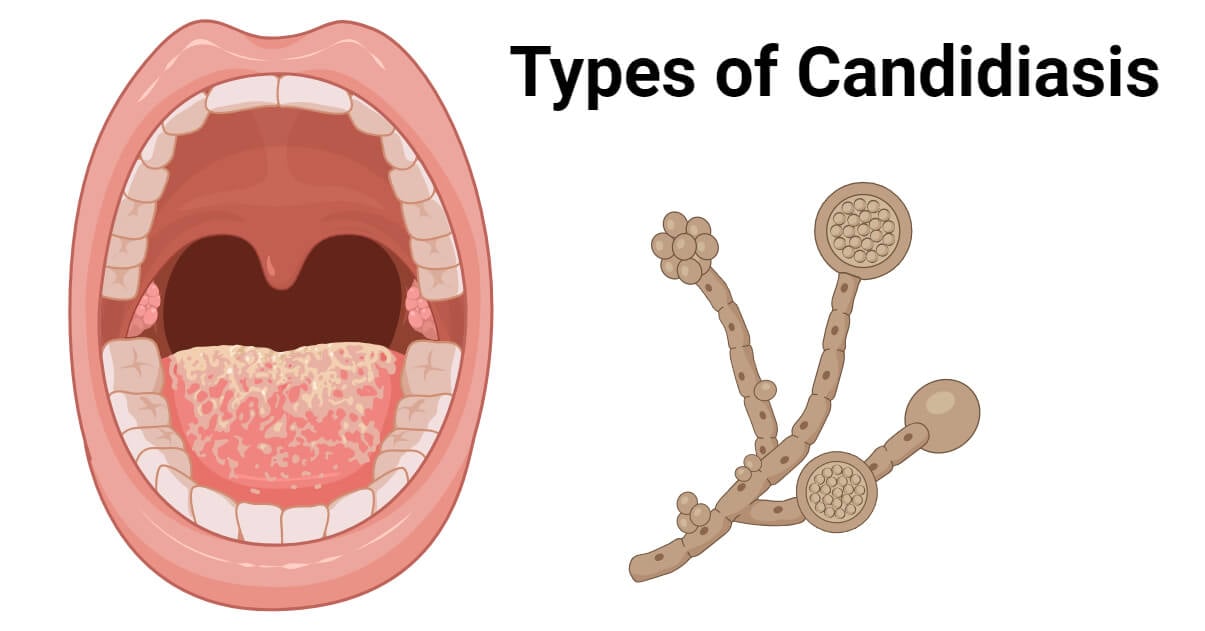
Candidiasis also known as moniliasis, is a fungal disease that is classified under opportunistic fungal infection, because of its occurrence in persons with an immune-suppressed system, especially newborns, HIV/AIDS patients, patients on antibiotic therapies, and cancer therapy patients.
- It usually does not cause disease in healthy individuals.
- It is an overgrowth in the gut by Candida albicans species of yeast-like fungi.
- The yeast-like fungi mutate into a fungal form, proliferating and invading the gastrointestinal tract and its walls, to cause candidiasis.
Interesting Science Videos
Causative agent of Candidiasis
- It is caused by a yeast-like fungus, known as Candida, and most commonly by a specific species known as Candida albicans.
- Candida albicans are normal gut inhabitants living in various sites of the body including the gastrointestinal tract, respiratory tract, vagina, and mouth.
- They are dimorphic fungi, existing in both mold and yeast forms.
- They are strictly aerobic, utilizing oxygen in its metabolisms and growth, therefore it is highly adaptive to the human mucous membranes.
- Their growth is naturally suppressed by other normal microbiota but when these microbiotas are disrupted, Candida multiplies rapidly, producing candidiasis disease.
- They have also been found to commonly live in hospitals, causing nosocomial blood infections in hospitalized patients.
Transmission of Candida albicans
- Besides being a normal flora, it is a transmissible fungal pathogen.
- Some modes of transmission include:
- Mother-to-infant transmission through childbirth, remaining as normal microflora, unless there is an overgrowth which can result in symptomatic disease, hence candidiasis.
- Child-to-mother transmission during breastfeeding, whereby the candida on the child’s tongue/mouth binds to the breast nipples on the mother during breastfeeding.
- Sexual transmission, this form is rare but it can occur and it has been listed by CDC as a sexually transmissible disease.
- Nosocomial transmission whereby immunocompromised patients acquire the yeast form healthcare workers, from invasive devices such as catheters and respirators. They account for 10% of nosocomial bloodstream infections.
Pathogenesis and pathology of Candidiasis
Candida albicans colonization of the host is based on the virulence factors it elicits making it adherent to the host organ systems.
These virulence factors include:
- The dimorphic nature of Candida albicans. It exists as both mold and/or yeast.
- Presence of adhesins and invasins, Als-3 proteins that enable it to attach and invade the surfaces.
- They also form biofilms during adherence which enables it to survive and thrive on the host.
- They also secrete proteases, phospholipases, and lipases which allows it to penetrate into the host cells.
Based on these virulence factors and the site of colonization of the fungal agent, candida infections (candidiasis) can be classified as follows:
- Mucosal Candidiasis affects the mucosal lining of the host such as oral candidiasis, candidal vulvovaginitis, gastrointestinal candidiasis, and respiratory candidiasis.
- Cutaneous candidiasis affects the skin, skin pores and nails, for example, candidal folliculitis, candidid, chronic mucocutaneous candidiasis, congenital cutaneous candidiasis, diaper candidiasis, candidal onychomycosis
- Systemic candidiasis affects the deep-seated organs and the bloodstream, for example, candidemia, a form of fungemia that causes sepsis, invasive candidiasis, chronic systemic candidiasis (hepatosplenic candidiasis).
- Antibiotic candidiasis is also known as iatrogenic candidiasis.
Disease cycle
- On the fungal colonization on the epithelial lining of the host, the fungi acquire nutrients from the lining and its cells, providing a suitable platform for growth.
- They cause superficial infection by degrading the surface proteins and if there is no prompt treatment, the infection persists into the tissues.
- Invasion of the tissues can affect the vascular system, through the spread and escaping immune interventions.
- The disease then disseminates into the endothelial tissues of various organs causing disseminated disease.
Clinical Manifestations of Candidiasis
- Candidiasis infection affects the cutaneous layer and the mucous membrane, which provides suitable conditions for growth. These manifestations affect the mouth, skin, vagina, and intestines.
- The most common types of candidiasis include:
Cutaneous and Mucosal candidiasis
- This infection is most common among persons who are immune-compromised including AIDS patients, pregnant mothers, diabetes, infants and children, women on birth control pills, and trauma patients (burns, maceration of the skin).
Oral candidiasis is also known as thrush or oropharyngeal candidiasis is the most common cutaneous and mucous candidiasis affecting the mouth cavity.
- It majorly affects newborns, who acquire it from the mother during childbirth, whose vagina is infected with Candida albicans.
- The fungi colonize the upper respiratory tract of the newborn during passage through the birth canal.
- Normally, when newborns are born, they do not harbor any microbiota, which allows Candida albicans growth.
- This enables the fungi to thrive and grow without competition or inhibition.
- Thrush occurs on the tongue, lips, gums, or the palates causing patchy to confluent, whitish pseudomembranous lesions made up of epithelial cells, yeast, and pseudohyphae.
- Other risks of developing Oral thrush include treatment with corticosteroids and antibiotics, high glucose levels, and cellular immunodeficiency.
- Another common cutaneous and mucosal is candidal vulvovaginitis.
- This is a yeast invasion of the vaginal mucosa characterized by irritation, pruritus, and vaginal discharge. Those at-risk are pregnant women, diabetic patients, and persons taking antibacterial drugs. These factors alter the normal microflora, local acidity, and secretions
- Other forms of cutaneous and mucosal candidiasis include skin invasions that occur due to trauma such as burns or surgical wounds.
- Intertriginous infection occurs in moist, warm parts of the body such as the axillae, groin, and intergluteal or inframammary folds; it is most common in obese and diabetic individuals forming red and moist vesicles.
- Onychomycosis is a candidal invasion of the nails and the nail plates causing painful erythematous swelling on the nail folds which resemble pyogenic paronychia, which destroys the nails,
Systemic Candidiasis
- This is also known as candidemia.
- Those most at risk are patients which invasive devices such as catheters, surgery patients, intravenous drug invasives, invasive drug abusers, aspirator patients, skin abrasions such as wounds, and gastrointestinal tract patients.
- Patients with an immune-compromised system especially the phagocytic defenses, develop occult lesions in the kidney, skin (macronodular lesions), eyes, heart, and meninges.
- Systemic candidemia is associated with chronic administration of corticosteroids or immune-suppressive agents, especially in persons with leukemia, lymphoma, and aplastic anemia.
- Candidal endocarditis can occur when there are deposition and growth of yeast and pseudohyphae on the heart valves.
- Systemic kidney infection can also occur associated with urinary tract infection in persons with foley catheters, diabetes, pregnancy, and antibacterial antibiotics
Chronic Mucocutaneous Candidiasis
- It is a rare form of candida infection that normally starts in early childhood. It is associated with cellular immunodeficiencies and endocrinopathies causing chronic superficial disfiguring infection affecting any areas of skin or the mucosa.
- Chronic mucocutaneous candidiasis affects effective Th17 immune responses.
Laboratory Diagnosis of Candidiasis
Specimen and specimen preparation
- Oral swabs and scrapings from lesions, vaginal swabs, blood, spinal fluid, tissue biopsies, urine, exudate, intravenous catheter materials.
- Spinal fluids are prepared by centrifugation.
Microscopic Examination
- Using tissue biopsies, centrifuged spinal fluid, tongue and mouth swabs, and scrapings, examine the specimens by Gram staining for identification of pseudohyphae and budding cells
- Skin or nail scrapings can be analyzed using KOH wet mount and calcofluor white dye for observation of the pseudohyphae and formation of a germ tube.
Cultural examination
- The specimens can be examined by culture methods using fungal media and/or bacterial media at room temperature or at 37°C.
- The colonies are examined for the formation of pseudohyphae or chlamydospores.
- A 10% KOH wet mount after culturing is used for the identification of pseudohyphae and the germ tube formed by Candida albicans.
- Candidemia is primarily diagnosed through blood cultures.
Treatment of Candidiasis
- Candidiasis is treated with antifungal drugs such as clotrimazole, nystatin, fluconazole, voriconazole, amphotericin B, and echinocandins. Fluconazole and echinocandins are administered intravenously. Caspofungin is used for the treatment of immunocompromised individuals.
- Localized infections such as mouth and throat candidiasis can be treated with topical medications and oral antifungals.
- Candidal skin infections are treated with topical antifungal treatment such as nystatin and miconazole.
- Gentian violet is used to treat oral thrush in breastfeeding babies and topical miconazole for breastfeeding mothers with breast candidal infection.
- Esophagitis candida infection can be treated with oral or intravenous amphotericin B.
- Vaginal candidiasis is treated with topical antifungal agents majorly fluconazole, imidazole or triazole some using vaginal suppositories or medical douches. This can also be done during pregnancy.
- Candidemia can be treated orally or intravenously using fluconazole, echinocandin like caspofungin, and also amphotericin B can be used.
Prevention and control
- Maintain a healthy lifestyle to reduce the overgrowth of Candida albicans.
- Good hygienic practices such as brushing teeth
- Proper nutrition
- Careful use of antibiotics
References and sources
- Medical Microbiology by Jawertz, 25th Edition
- Microbiology by Prescott 5th Edition
- https://www.cdc.gov/fungal/diseases/candidiasis/index.html
- https://www.ncbi.nlm.nih.gov/pubmed/25809621
- https://www.britannica.com/science/candidiasis
- https://microbewiki.kenyon.edu/index.php/Candida_albicans_(Pathogenesis)
- https://pmj.bmj.com/content/78/922/455
- https://www.ahajournals.org/doi/full/10.1161/CIR.0000000000000298
- https://uomustansiriyah.edu.iq/media/lectures/4/4_2018_12_27!04_51_18_PM.pptx
- https://www.researchgate.net/publication/254510262_Non-Candida_albicans_Candida_yeasts_of_the_oral_cavity
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6441600/
- https://www.medicalnewstoday.com/articles/317970
- https://www.medicalnewstoday.com/articles/312495
- https://www.healthgrades.com/right-care/womens-health/candidiasis-information
- https://www.aihw.gov.au/getmedia/3876a585-9a48-4553-8939-59711f1aa573/ah16-6-14-safety-quality-australian-hospitals.pdf.aspx
- https://web.duke.edu/pathology/MicroCases/Microbiology_Infectious_Disease_Case_Studies.doc
- https://quizlet.com/56305997/yeasts-moulds-flash-cards/
- https://quizlet.com/143926689/neonate-flash-cards/

This is a very elaborate resume of candida infection for academic and professional purpose.