Vibrio parahaemolyticus is one of the leading causative agents of human acute gastroenteritis and occur usually from the consumption of raw, undercooked, and cross-contaminated seafood products.
They are inhabitants of tropical marine and coastal environments and are found in the gut of filter-feeding molluscan shellfish (oysters, clams, and mussels), where they adhere and multiply.
Vibrio parahaemolyticus also cause wound and ear infection and septicemia in the case of immune-compromised individuals who are exposed to seawater.
Vibrio species that are pathogenic to humans are Vibrio cholera, Vibrio carchariae, Vibrio mimicus, Vibrio vulnificus, Vibrio metschnikovii, Vibrio damsel and Vibrio fluvialis.
In Japan and many Asian countries, V. parahaemolyticus is responsible for causing about 20 to 30% of food poisoning cases every year.
Similarly, in the United States, V. parahaemolyticus is known as a leading cause of human gastroenteritis therefore, its prevalence, involvement of virulence factors, and its effect on human health, along with the identification techniques, need to be addressed to reduce the potential harm.
Interesting Science Videos
Characteristics of Vibrio parahaemolyticus
- Gram-negative
- Curve rod-shaped
- Non-spore former
- Slightly halophilic (20 to 25 ppt salt)
- Facultative anaerobe
- Oxidase positive
- Motile
- Optimum temperature 30 to 35°C
- pH range from 6.8 to 10.2
Source of contamination of Vibrio parahaemolyticus
- Vibrio parahaemolyticus is a marine and halophilic bacterium that floats freely on the water with the help of its single polar flagellum.
- It adheres to animate surfaces like fishes, crabs, shrimp, lobster, zooplankton, and shells of other aquatic animals.
- When raw and undercooked seafood that is contaminated with V. parahaemolyticus is consumed, it causes acute gastroenteritis in humans.
- Other sources are cross-contamination of virulent strains of V. parahaemolyticus from the sea products or equipment to other products.
- When open wound or cuts is exposed to contaminated seawater, it can also cause infection.
Pathogenesis of Vibrio parahaemolyticus Food Poisoning
- Vibrio parahaemolyticus is classified into two types based on its antigenic properties; Somatic (O) and Capsular (K) antigen.
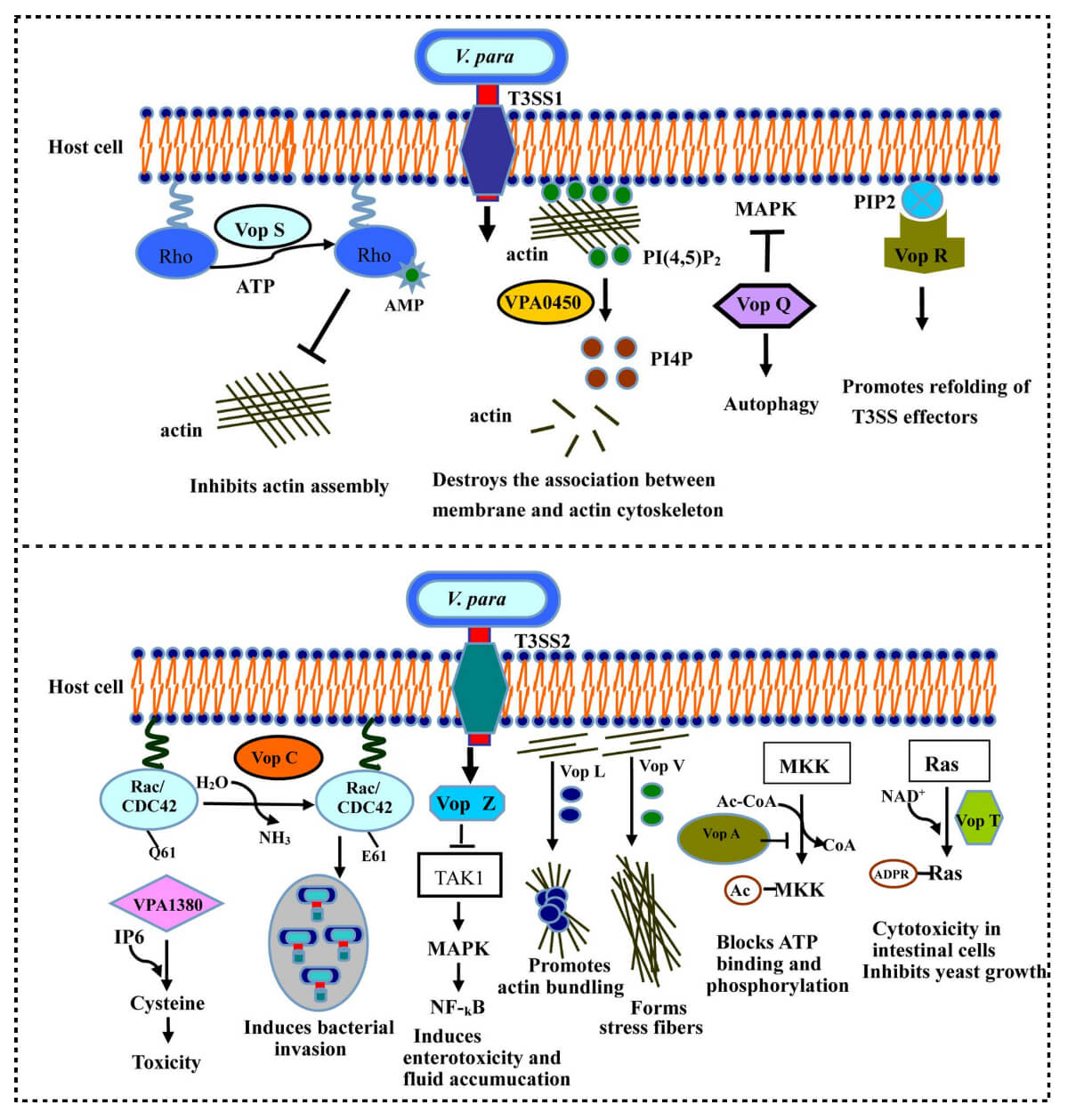
- It also produces different virulence factors such as adhesins, thermostable direct hemolysin (tdh), TDH-related hemolysin (trh), and Type III secretion systems (T3SS1 and T3SS2).
- Additionally. V. parahaemolyticus have two different types of flagella for motility as well as to produce a capsule that helps the pathogen to survive in harsh environmental conditions.
- Infection usually occurs through the fecal-oral route and adheres to the host cell with the help of bacterial adhesion factors, which are present at the bacterial cell surface.
- Thermostable direct hemolysin (TDH) causes lysis of human erythrocyte cells by binding on the red blood cell membrane.
- It forms a pore on the surface of the membrane, which leads to the permeation of cell components of RBCs.
- Vibrio parahaemolyticus also forms a toxin, an enzymatic activity known as cytotoxicity formed by tdh and TDH-related hemolysin (trh).
- TDH is responsible for causing toxicity of cells by forming a channel where extracellular Ca2+ concentration and Cl– secretion increase within the cell.
- As the osmotic pressure increases in the cell, its morphology, pathology, and self-regulation change causing the cell to expand and eventually die.
- Another Thermolabile hemolysin (TLH) gene is associated with stimulating intestinal infection and also causes lysis of human erythrocytes.
- Early studies showed that urease is an important virulence factor in trh+ V. parahaemolyticus strains that causes gastrointestinal inflammatory lesions.
- The type three secretion system (T3SS1) induces autophagy and cytotoxicity during tissue cell infection.
- It serially causes autophagy, cell blebbing, cell rounding, cell lysis, and finally, death.
- Type IV secretion system (T6SS1 and T6SS2) addresses toxic effector proteins in the cytoplasm of eukaryotic cells that disrupts the cell and kills it.
- T6SS is present in other Vibrio species as well and is used as a virulence marker in detecting pandemic or non-pandemic strains.
- T6SS1 gene is most active in warm conditions and can be isolated from the clinical sample as well as from the environment.
Epidemiology of Vibrio parahaemolyticus Food Poisoning
- Vibrio parahaemolyticus infection has been reported in about 40.1% of outbreaking cases in the part of coastal provinces in eastern China.
- The first outbreak of Vibrio parahaemolyticus disease occurred in Japan in 1950, with 272 cases reported of acute gastroenteritis with the death of 20 individuals.
- It had been an epidemic in eastern China, with 802 reported cases causing illness to 17,462 individuals.
- An outbreak of similar cases has been reported frequently in countries of Asia, Europe, Africa, and America.
- More than 700 cases were reported in the United States of America from 1997 to 1998 with the consumption of raw contaminated oysters.
- V. parahaemolyticus food poisoning usually occurs during summer, from June to October, when the water is warm for the organism to thrive.
- Crab, shrimp, lobster, shellfish, oyster, clam, and tuna are high-risk sea products that must be thoroughly cooked before consumption.
Signs and symptoms of Vibrio parahaemolyticus Food Poisoning
- The typical symptoms are watery diarrhea, nausea, vomiting, abdominal cramp, fever, and chills.
- The incubation period is about 12 to 24 hours of consumption of pathogen-contaminated food and resolves within 5 to 7 days.
- Immunocompromised individuals may take a long time of about 10 to 15 days to recover as the disease is self-limiting and requires no medication.
- Some patients in severe cases may face mucus or blood in stool with a decrease in blood pressure and become unconscious with pale and cyanotic skin, and even die.
- Death occurs when the patient’s internal system changes with inflammation and erosion of the jejunum and ileum, with liver, spleen, and lung damage have been reported.
Detection methods of Vibrio parahaemolyticus Food Poisoning
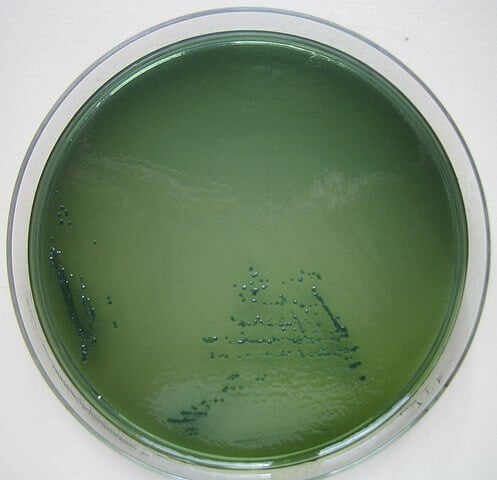
- Selective enrichment media with sodium dodecyl sulfate (SDS), alkylbenzoate sulphonate, and bile salts are used for culturing and isolation of Vibrio parahaemolyticus.
- The enrichment broth, like alkaline peptone water (APW), which has optimum pH and a relatively high concentration of NaCl, favors the growth of Vibrio species.
- The most probable number (MPN) method also determines the population density of an organism in a sample which is a conventional method mostly used in the laboratory.
- For the identification of strains of V. parahaemolyticus, molecular techniques such as conventional phenotyping, biochemical tests, PCR-based assays, DNA based methods have been used.
- Loop-mediated isothermal amplification (LAMP) assays and Random amplified polymorphic DNA (RAPD-PCR) are used for typing and differentiating the strains of organisms.
Treatment of Vibrio parahaemolyticus Food Poisoning
- However, the disease is self-limiting, but in severe cases, medication is required.
- Some of the common treatments are oral rehydration and the use of antibiotics such as tetracycline to soothe the illness.
- Drinking plenty of fluid to replace the electrolyte loss and bed rest helps to resolve the illness soon.
Prevention and Control measures of Vibrio parahaemolyticus Food Poisoning
- As V. parahaemolyticus is naturally inhabitant the seawater and the sea products, and to prevent its infection, raw and undercooked shellfish and oysters must be avoided.
- Maintaining personal hygiene while handling sea products and avoiding cross-contamination between raw and cooked shellfish.
- Do not get exposed to saltwater or brackish water if you have a cut or wound, and use a waterproof bandage if possible.
References
- Letchumanan, V., Chan, K.-G., & Lee, L.-H. (2014). Vibrio parahaemolyticus: a review on the pathogenesis, prevalence, and advance molecular identification techniques. Frontiers in Microbiology, 5.
- Wang R, Zhong Y, Gu X, Yuan J, Saeed AF, Wang S. The pathogenesis, detection, and prevention of Vibrio parahaemolyticus. Front Microbiol. 2015 Mar 5;6:144. doi: 10.3389/fmicb.2015.00144. Erratum in: Front Microbiol. 2015;6:437. PMID: 25798132; PMCID: PMC4350439.
- Risk assessment tools for Vibrio parahaemolyticus and Vibrio vulnificus associated with seafood, Food and Agriculture Organization of the Unites Nations, ISSN 1726-5274.
- Baker-Austin, C., Jenkins, C., Dadzie, J., Mestanza, O., Delgado, E., Powell, A., … Martinez-Urtaza, J. (2020). Genomic epidemiology of domestic and travel-associated Vibrio parahaemolyticus infections in the UK, 2008–2018. Food Control, 115, 107244.
- Yaashikaa, P. R., Saravanan, A., & Kumar, P. S. (2016). Isolation and identification of Vibrio cholerae and Vibrio parahaemolyticus from prawn (Penaeus monodon) seafood: Preservation strategies. Microbial Pathogenesis, 99, 5–13.
- Bolen, J. L., Zamiska, S. A., & Greenough, W. B. (1974). Clinical features in enteritis due to vibrio parahemolyticus. The American Journal of Medicine, 57(4), 638–641.
- https://www.elsevier.com/books/foodborne-diseases/dodd/978-0-12-385007-2
