- Rickettsia is small-sized intracellular bacteria about 0.3 to 2 µm and because of its small size, it was thought to be a virus.
- These bacteria multiply in the cytoplasm of eukaryotic cells by binary fission and contain both DNA and RNA as genetic material.
- These small gram-negative bacteria are found in the intestinal tract of ticks, fleas, mites, and chiggers and cause Rocky Mountain spotted fever, rickettsialpox, epidemic typhus, and murine typhus.
- It belongs to the Rickettsiaceae family and consists of three genera namely Rickettsia, Orientia, and Candidatus Cryptoprodotis.
- Rickettsia and Orientia are closely related to each other while Candidatus Cryptoprodotis are detected in ticks and do not cause human infection.
- In the genus Rickettsia, 25 species are recognized to date and are classified into four groups.

- The typhus group includes the flea-borne Rickettsia typhi and the louse-borne Rickettsia prowazekii, the spotted fever group is caused by 21 Rickettsiae species, the third is Rickettsia bellii and the fourth Rickettsia Canadensis group.
- R. rickettsii rickettsiosis is the most prevalent tick-borne disease in the United States that causes Rocky Mountain spotted fever.
- It has a high fatality rate of about 30% in untreated cases but even with proper treatment 72% are hospitalized and the fatality rate is 4% according to the report of the Center for Disease Control and Prevention.
Interesting Science Videos
Characteristics of Rickettsia
- Gram-negative bacteria
- Non-spore forming
- Non-motile
- Pleomorphic bacteria
- Cocci (~0.1µm), bacilli (1 to 4µm) or thread (upto 10µm)
- Circular genome (1 to 2.1 Mb)
- Replicates by binary fission
- Contains a microcapsular protein layer above the outer membrane
- Cannot survive in an artificial nutrient environment
- Can grow in tissue cells or chicken embryo culture
Ecology and Epidemiology of Rickettsia
- Rickettsia is globally distributed throughout tropical, subtropical, and temperate regions based on the availability of small blood-sucking anthropods.
- Rats are the primary reservoir of R. typhi which are transmitted to mammals by the vector rat flea and are responsible for causing murine typhus.
- Ticks are also hematophagous arthropod vector that transmits tropical rickettsioses by biting humans and are transmitted through saliva.
- The infection period takes 6 hours of attachment and feeding on the host skin surface before transmission.
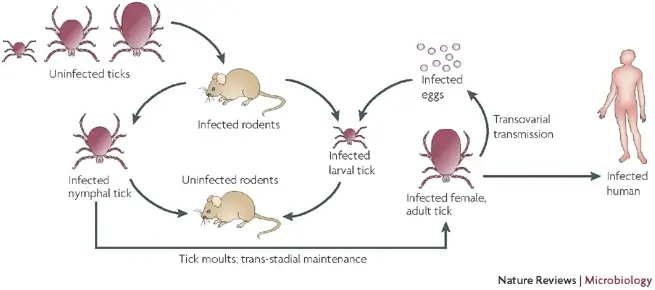
- Tick-borne rickettsioses and spotted fever groups are transmitted in ticks in two ways either by transtadially (stage to stage transmission) or transovarially (transfer of bacteria from adult female to eggs).
- The infection can also be spread by scratching, itching, and rubbing the infectious tick feces into the skin.
- Rickettsioses are emerging zoonotic diseases during international travel as the ticks are being carried out by birds, Northern American flying squirrels, and their ectoparasites.
- It has been discovered that the alternative zoonotic cycle also plays an important role in the life cycle of typhus rickettsiae.
- Most cases of human spotted fever rickettsioses occur in summer due to high exposure activity between humans and ticks.
- Children aged 5 to 9 years old and older adults aged 40 to 64 years old are high-risk groups for Rocky Mountain spotted fever.
- According to the analysis of the GeoSentinel database, about 3.1% of travelers have rickettsiosis.
- An increase in the number of rickettsiosis infections and northward expansion of several tick species might be due to the cause of global warming.
Pathogenesis of Rickettsioses
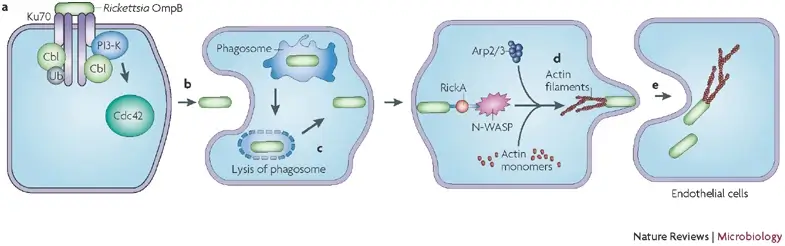
- Human rickettsiosis occurs when an infected tick or mite bites on the surface of the skin or through the fecal-oral route from the ingestion of infected louse or flea feces.
- Infection occurs after the Rickettsiae invade the vascular endothelium, multiply in the cytoplasm, and spread via the bloodstream to different parts of the body.
- It then infects the vascular endothelium and smooth muscle cell with an increase in immune-effector responses.
- The disseminated infection increases the permeability of vascular cells and fluids are assembled in the interstitial surroundings.
- It leads to a decrease in blood volume which might cause hypovolemic shock and death.
- Other affected vital organs are the brain, liver, lungs, heart, and adrenal glands causing diseases like meningoencephalitis and interstitial pneumonitis.
- Infection can also occur by inhalation of the organisms or their feces which mainly occurs in laboratory workers due to poor hygienic practices.
- When the kidney is infected, acute renal failure may occur due to a decrease in the perfusion of fluid.
- The vascular leakage of plasma into the alveolar spaces leads to gas exchange in the lungs and causes hypoxemia.
- Cellular immunity of the host cell is important for inhibition of intracellular rickettsiae by killing it in endothelial cells with the inducible nitric oxide production.
- The inducible nitric oxide is activated by the cytokines gamma interferon and tumor necrosis factor.
- Natural killer cells also produce immune responses against rickettsial disease and the humoral immune response produces antibodies against the outer membrane protein and prevents reinfection.
Clinical syndrome of Rickettsioses
- The incubation period is usually 7 days long with the early symptoms of severe headache, fever, chills, malaise, and myalgia.
- A macular rash may develop after several days and typically appears on the wrist, ankles, palm, and soles at the initial stage and spreads throughout the trunk.
- Diseases like Rocky Mountain spotted fever, rickettsialpox, epidemic typhus, and murine typhus are caused by Rickettsia species.
- The disease has many complications such as respiratory failure, encephalitis, and acute renal failure through which the patient may die within 5 days of severity.
Diagnosis of Rickettsioses
- The initial diagnosis is based on the clinical observation by immunohistochemical detection by taking skin biopsies of skin lesions for antigen detection.
- Serological tests are done to confirm the diagnosis using serum samples but the antibodies might not be detected at the initial stage of infection.
- Rickettsiosis is difficult to diagnose in an artificial culture therefore, they are isolated in viable eukaryotic host cells such as embryonated eggs, tissue cultures, antibiotic-free cell cultures, and many susceptible laboratory animals.
- Rickettsia is grown on cell lines like HeLa, Hep2, Detriot-6, and mouse fibroblasts for their maintenance, and for isolation, they are cultivated in developing 5 to 6 days old chick embryos.
- Laboratory animals like Guinea pigs and mice are used for the isolation of Rickettsia species from animal specimens.
- For the diagnosis of Rocky Mountain spotted fever, a direct fluorescent antibody test is used as it is a rapid and specific method for confirmation.
- IFA and ELISA are newly developed serological tests for the early diagnosis of Rickettsial disease.
Treatment of Rickettsioses
- Presumptive treatment of Rickettsioses is the use of antibiotics such as doxycycline, tetracycline, chloramphenicol, and fluoroquinolones.
- Doxycycline is more effective and should be administered at an early stage of infection while chloramphenicol is less effective and is prescribed during pregnancy.
Prevention and Control of Rickettsioses
- To limit the risk of infection, use protective clothing, insect repellent creams, and removal of attached ticks decreases the chance of transmission.
- Avoid activities like bushwalking and camping where direct human contact might occur with ticks, lice, mites, and fleas.
- A vaccine is not available for Rickettsial infection to date therefore it is best to prevent direct contact with these vectors.
References
- Crossley, E. C., Jordan, J. M., & Walker, D. H. (2008). Rickettsia. International Encyclopedia of Public Health, 582–590.
- Walker, D. H. (2017). Rickettsia. International Encyclopedia of Public Health, 370–377.
- Socolovschi, C., Parola, P., & Raoult, D. (2013). Tick-borne Spotted Fever Rickettsioses. Hunter’s Tropical Medicine and Emerging Infectious Disease, 546–552.
- Silva-Ramos, C. R., Hidalgo, M., & Faccini-Martínez, Á. A. (2021). Clinical, epidemiological, and laboratory features of Rickettsia parkeri rickettsiosis: A systematic review. Ticks and Tick-Borne Diseases, 12(4), 101734.
- Saito, T. B., Bechelli, J., Smalley, C., Karim, S., & Walker, D. H. (2018). Vector tick transmission model of spotted fever rickettsiosis. The American Journal of Pathology.
- Walker, D., Ismail, N. Emerging and re-emerging rickettsioses: endothelial cell infection and early disease events. Nat Rev Microbiol 6, 375–386 (2008). https://doi.org/10.1038/nrmicro1866
