- Klebsiella pneumoniae is a gram-negative, encapsulated, non-motile bacterium that is found in the environment and has been associated with pneumonia in the alcoholic and diabetic patient population. K. pneumoniae is also a well-known cause of community-acquired pneumonia.
- The bacterium typically colonizes human mucosal surfaces of the oropharynx and gastrointestinal (GI) tract.
- K. pneumoniae is present in the respiratory tract and feces of about 5% of normal individuals.
Interesting Science Videos
Virulence Factors
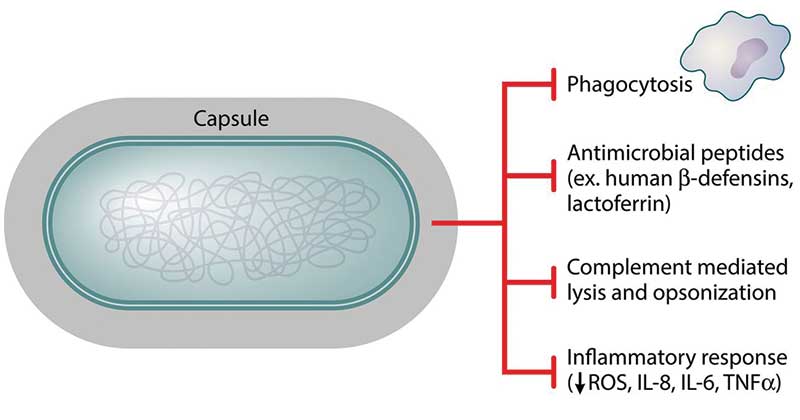
Figure: Role of a capsule in K. pneumoniae virulence, Image Source: DOI: 10.1128/MMBR.00078-15
- The polysaccharide capsule of the organism is the most important virulence factor and allows the bacteria to evade opsonophagocytosis and serum killing by the host organism. Those Klebsiella species without a capsule tend to be less virulent.
- Lipopolysaccharides coat the outer surface of a gram-negative bacteria. The sensing of lipopolysaccharides release an inflammatory cascade in the host organism and has been shown to be a major culprit of the sequela in sepsis and septic shock.
- Fimbriae, allows the organism to attach itself to host cells.
- Siderophores are another virulence factor that is needed by the organism to cause infection in hosts. Siderophores acquire iron from the host to allow propagation of the infecting organism.
Pathogenesis
- Klebsiella infections are spread through exposure to the bacteria via the respiratory tract, which causes pneumonia, or the blood to cause an infection in the bloodstream.
- Healthcare settings are most vulnerable to Klebsiella infections due to the nature of procedures that allow easy access of bacteria into the body. Patients who are on ventilators, catheters, or surgery wounds are highly prone to catching this deadly infection.
- K. pneumoniae utilizes a variety of virulence factors, especially capsule polysaccharide, lipopolysaccharide, fimbriae, outer membrane proteins and determinants for iron acquisition and nitrogen source utilization, for survival and immune evasion during infection.
- Pathogenic strains associated with the upper respiratory tract are usually heavily encapsulated. Many pathogenic strains possess fimbriae, which act as adhesins and a virulence factor that permits colonization of mucosal surfaces. The capsule also serves as a virulence factor by inhibiting phagocytosis.
- Pathogenic features of Klebsiella-induced pneumonia include cell death associated with bacterial replication, avoidance of phagocytosis by phagocytes, and the attenuation of host defense responses, chiefly the production of antimicrobial factors.
Clinical Features
- It causes 11.8% of all hospital-acquired pneumonia in the world. K. pneumoniae can produce extensive hemorrhagic necrotizing consolidation of the lung.
- It also sometimes produces urinary tract infection and bacteremia with focal lesions in debilitated patients.
A. Pneumonia
- Pneumonia caused by Klebsiella species frequently involves necrotic destruction of alveolar spaces, the formation of cavities, and production of blood-tinged sputum.
- The clinical manifestations of pneumonia caused by K. pneumoniae are similar to those seen in community-acquired pneumonia. Patients may present with a cough, fever, pleuritic chest pain and shortness of breath.
- “Currant jelly” sputum is a hallmark of infection with Klebsiella pneumoniae. The reason for this is that K. pneumoniae causes significant inflammation and necrosis of the surrounding tissue.
Complications: Pneumonia caused by K. pneumoniae can be complicated by bacteremia, lung abscesses, and the formation of an empyema.
B. Bacteremia
- If introduced into the bloodstream, K. pneumoniae has the capability of causing meningitis, which affects the CNS.
- Symptoms include sharp head pain, nausea, dizziness, and impaired memory.
C. Urinary tract infections
- UTIs alongside bacteremia are leading consequences of Klebsiella infections as well.
References
- Murray, P. R., Rosenthal, K. S., & Pfaller, M. A. (2013). Medical microbiology.
- Philadelphia: Elsevier/Saunders.
- https://www.ncbi.nlm.nih.gov/books/NBK519004/
- https://microbewiki.kenyon.edu/index.php/Klebsiella_pneumoniae_pathogenesis
- https://www.ncbi.nlm.nih.gov/pubmed/25340836
- https://cmr.asm.org/content/11/4/589
- https://www.researchgate.net/publication/267731558_Molecular_pathogenesis_of_Klebsiella_pneumoniae
- https://microbeonline.com/klebsiella-pneumoniae-properties-virulence-diseases-diagnosis/
- https://www.uptodate.com/contents/microbiology-and-pathogenesis-of-klebsiella-pneumoniae-infection
- https://www.futuremedicine.com/doi/10.2217/fmb.14.48
