Interesting Science Videos
Laboratory Diagnosis of Klebsiella pneumoniae
- In the setting of pneumonia, infection with K. pneumoniae is confirmed by either sputum culture analysis, blood culture analysis or midstream urine depending upon the illness.
- The presence of gram-negative rods in Gram-stained smears suggests Klebsiella; they maybe capsulated and non-sporing.
- Material is inoculated into blood agar and Mac Conkey agar medium and incubated aerobically.
- Blood Agar: Mucoid, non-hemolytic colonies
- MacConkey Agar: Mucoid, lactose-fermenting (pink colored) colonies
- After pure cultures have been obtained by selecting colonies from aerobically incubated plates, they are identified by biochemical reactions and colony morphology.
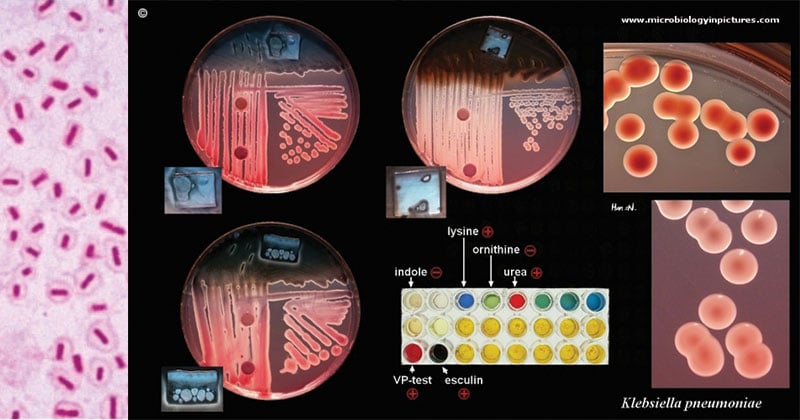
Image Source: Microbiology In Pictures
Tests/reactions
| Indole Production Test | Negative (K. oxytoca is Indole positive) |
| Methyl-Red Test | Negative |
| Voges-Proskauer Test | Positive |
| Citrate Utilization Test | Positive |
| Hydrogen Sulfide Production (TSI) |
Negative |
| Urea Hydrolysis Test | Positive |
| Lysine Decarboxylase Test | Positive |
| Arginine Dihydrolase Test | Negative |
| Ornithine decarboxylase test | Negative |
| Motility at 36 °C | Non-motile |
| D-Glucose (acid/gas) | Positive/Positive |
| D-mannitol fermentation | Positive |
| Sucrose fermentation | Positive |
| Lactose fermentation | Positive |
| D-sorbitol fermentation | Positive |
| Cellobiose | Positive |
| Esculin hydrolysis | Positive |
| Acetate Utilization Test | Positive |
| ONPG Test | Positive |
Treatment of Klebsiella pneumoniae
- Given the low occurrence of K. pneumoniae pulmonary infections in the community, treatment of pneumonia should follow standard guidelines for antibiotic therapy.
- Once infection with K. pneumoniae is either suspected or confirmed, antibiotic treatment should be tailored to local antibiotic sensitivities.
- Current regimes for community-acquired K. pneumoniae pneumonia include a 14-day treatment with either a third or fourth generation cephalosporin as monotherapy or a respiratory quinolone as monotherapy or either of the previous regimes in conjunction with an aminoglycoside.
- For nosocomial infections, a carbapenem can be used as monotherapy until sensitivities are reported.
- Surgery may be needed for patients who experience empyema, lung abscess, pulmonary gangrene, or respiratory tract obstruction following a Klebsiella infection.
- Correction of posterior urethral valves in patients with reoccurring UTIs is a possibility or other abnormalities influenced by infection.
- Nosocomial isolates of K. pneumoniae often display multidrug-resistance phenotypes that are commonly caused by the presence of extended-spectrum β-lactamases or carbapenemases, making it difficult to choose appropriate antibiotics for treatment.
Prevention of Infection
- Klebsiella infections are most well-known in hospitals spread through person-to-person contact by contaminated hands of surrounded people in the hospitals, whether it be an employee or a patient.
- Nurses who look after these patients should maintain strict infection control protocols to prevent the spread of the organism.
- Hand washing is crucial for both medical personnel and visitors.
- Nurses should only ensure that only devices are only used once to minimize transmission from contaminated devices.
- The pharmacist should ensure that empirical antibiotic prescribing is not carried out, as this only leads to the development of drug resistance.
References
- Murray, P. R., Rosenthal, K. S., & Pfaller, M. A. (2013). Medical microbiology.
- Philadelphia: Elsevier/Saunders.
- https://www.ncbi.nlm.nih.gov/books/NBK519004/
- https://microbewiki.kenyon.edu/index.php/Klebsiella_pneumoniae_pathogenesis
- https://www.ncbi.nlm.nih.gov/pubmed/25340836
- https://cmr.asm.org/content/11/4/589
- https://www.researchgate.net/publication/267731558_Molecular_pathogenesis_of_Klebsiella_pneumoniae
- https://microbeonline.com/klebsiella-pneumoniae-properties-virulence-diseases-diagnosis/
- https://www.uptodate.com/contents/microbiology-and-pathogenesis-of-klebsiella-pneumoniae-infection
- https://www.futuremedicine.com/doi/10.2217/fmb.14.48
- https://www.sciencedirect.com/topics/medicine-and-dentistry/klebsiella-pneumoniae

Can you please why to add sheep blood in blood agar