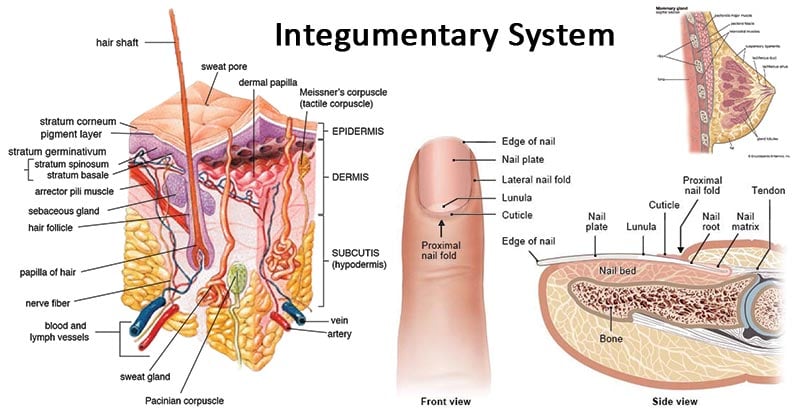
Figure: The Integumentary System. Image Source: Wikipedia, InformedHealth.org and Encyclopædia Britannica, Inc.
Interesting Science Videos
Integumentary System definition
The integumentary system is a system comprised of organs that are the outermost protective covering of the animal body, the skin, and its various derivatives. The integumentary system protects against many threats such as infection, desiccation, abrasion, chemical assault, and radiation damage. In humans, the primary organ of the integumentary system is the skin. Along with skin, several other glands and different sensory units like somatosensory receptors and nociceptors are also a part of this organ system.
Organs of the Integumentary System (structure and functions)
The integumentary system is composed of skin and its appendages, subcutaneous tissue, deep fascia, mucocutaneous junctions, and breasts.
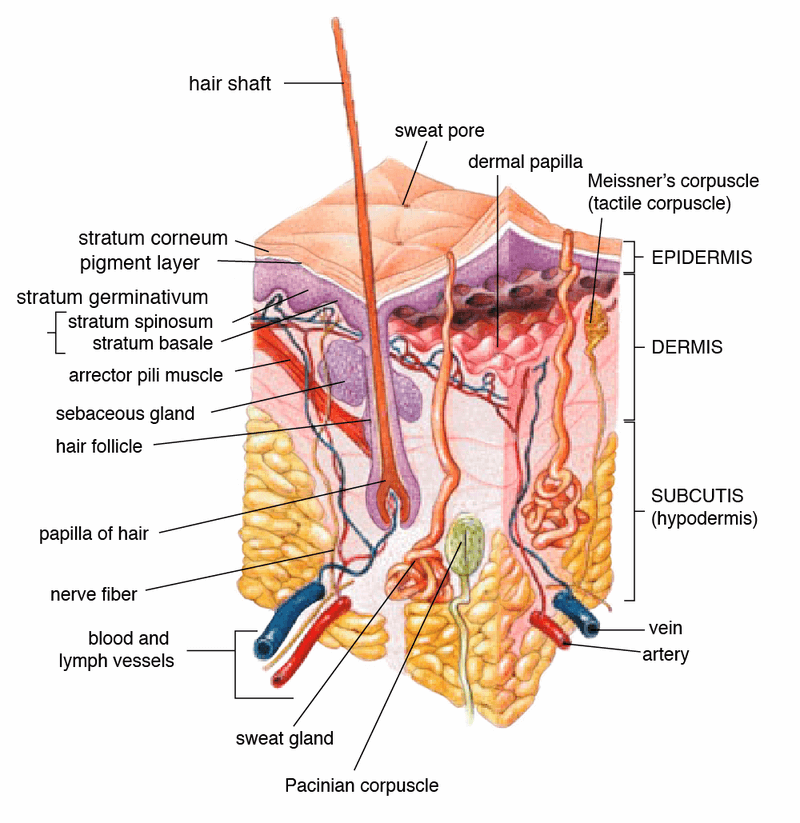
Figure: Anatomy of the human skin. Image Source: Wikipedia.
1. Skin
- Skin is the largest organ in our body.
- It covers up to 2m2 of the body surface area and contains numerous glands and sensory units.
- The skin is continuous but structurally different from the mucous membrane that lines the buccal cavity.
Structure
- Structurally, the skin is a multicellular organ composed of two distinct layers of tissues; an outer epidermis developed from ectoderm, and (ii) an inner dermis derived from the mesoderm.
- The related abundance of the two layers differs according to the environment.
a. Epidermis
- The epidermis is a stratified epithelium and usually quite thin in comparison to the dermis.
- It is the outer layer of skin that has no blood vessels supply, and the cells in the squamous epithelium receive blood via diffusion.
- It is further distinguished into two regions— The outermost region of many layers of dead usually flattened (squamous) cells forms a horny, resistant covering or stratum corneum on the skin surface.
- Its cells accumulate a horny protein, called keratin, gradually die and eventually wear off in the form of scurf or dandruff.
- The innermost or basal region of epidermis includes a single row of living columnar cells, the Malpighian layer, or stratum germinativum, which is separated from the underlying dermis by a basement membrane.
- Its cells actively divide and continually replace the worn-out cells of the cornified layer.
- Besides, the epithelium also contains few cells like melanocytes which are responsible for the pigmentation on the skin.
Functions
- Since keratin is tough and insoluble in water, the keratinized stratum corneum protects against mechanical injuries, fungal and bacterial attacks, and loss of body moisture.
- Melanin in the epidermis protects dermis and other internal organs against exposure to ultraviolet rays and its damaging effects.
- The epidermis is also responsible for the synthesis of Vitamin D under the exposure of UV rays from the sunlight.
- The Langerhans cells found in the epidermis are a part of the skin immune system and protect against foreign antigens.
- The sensory cells and receptors in the epidermis are responsible for sensation in the skin.
b. Dermis
- Dermis or corium, which is the inner layer of skin, is comparatively thicker than the epidermis.
- It is composed of fibrous connective tissue and contains many blood capillaries, lymph vessels, muscle fibers, nerve fibers, sense organs, and elastic fibers which bring the skin back to its normal shape.
- Pigment cells or melanocytes are mostly located in the dermis, although sometimes pigment granules are also found in the epidermis.
- Fat may accumulate as reserve food in specialized cells, called adipocytes, in deeper parts of the dermis and the subcutaneous tissue.
- Different glands like sweat glands and sebaceous glands are also present in the dermis.
Functions
- The blood vessels present in the dermis provide nourishment and waste removal from its cells as well as from the base of the epidermis.
- Dermis helps in thermoregulation as the sweat glands promote evaporation, resulting in a loss of excessive body heat.
- Dermis also provides support to the epidermis and allows the base for the cells.
c. Hypodermis
- The hypodermis is the innermost and thickest layer of the skin instead is the deeper subcutaneous tissue made of fat and connective tissue.
- This layer consists of cells like fibroblasts, fat cells, connective tissue, larger nerves and blood vessels, and macrophages.
- The purpose of hypodermis is to attach the skin to underlying bone and muscle as well as supplying the other layers of skin with blood vessels and nerves.
- The hypodermis is made up of loose connective tissue and elastin protein.
- The thickness of this layer differs in different parts of our body and is also significantly different in males and females.
- It is thickest in the shoulders and abdomen in men while in females, it is thicker in the hips and thighs.
Functions
- Hypodermis contains a large amount of fat which function as energy storage.
- The thick layer protects the external agents and also acts as an insulator, protecting against cold.
- This layer provides attachment between the epidermis and dermis to the internal organs in the body.
- An appetite-regulating hormone called leptin is also synthesized by fat cells in the hypodermis layer.
Skin Anatomy and Physiology Video Animation

2. Appendages of the skin
- The skin itself is relatively simple, but its derivatives are numerous and complex.
- These derivatives are termed appendages of the skin and are formed form derived epidermal cells.
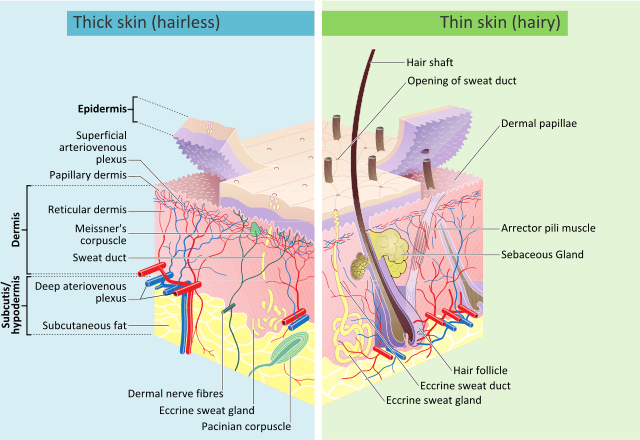
Image Source: Wikimedia.
a. Epidermal glands
- Integumental or epidermal glands are formed by the Malpighian layer of epidermis that arise in the epidermis but often invade the dermis.
- They may be unicellular or multicellular, tubular or alveolar in shape, and simple, compound or branched.
- They are lined by cuboidal cells or columnar epithelium and are usually named after their nature or function.
Some of the common epidermal glands found in humans and other mammals are:
i. Sudoriferous Glands
- Sweat glands or sudoriferous glands (sudor = sweat) are abundant in the skin of most mammals.
- Sudoriferous glands are either of two types of secretory skin glands, eccrine or apocrine.
- Eccrine glands open directly onto the skin surface whereas apocrine glands open onto associated hair follicles.
- Eccrine glands can be found almost anywhere on the human body, with the highest concentration found on the palms and soles.
- However, apocrine glands are found in more restricted areas of the body including the axilla, anogenital region, external ear canal, and areola.
Structure
- They are slender coiled tubes embedded deep in the dermis, with their long ducts opening on the skin surface.
- The sweat glands consist of a secretory unit called a glomerulus and a long duct that takes the sweat to the target surfaces.
- These glands are embedded in the dermis or hypodermis, which are surrounded by adipose tissue.
- The secretory unit is surrounded by myoepithelial cells that facilitate the excretion of sweat.
- Ciliary glands in eyelashes and along margins of eyelids are modified sweat glands.
Function
- An essential function of the sweat gland is in the regulation of body temperature. Evaporation of watery perspiration also helps to cool and regulate body temperature in hot environments.
- Also, a little urea and some salts are eliminated dissolved in water in the sweat produced by these glands which help in excretion.
ii. Sebaceous gland
- The sebaceous gland consists of secretory epithelial cells derived from the same tissue as the hair follicles.
- These glands secrete an oily antimicrobial substance, sebum, into the hair follicles.
- Sebaceous glands are present in all parts of the body except the palms of the hands and the soles of the feet.
- The number of these glands is higher in the scalp, face, axillae, and groins.
Structure
- Most sebaceous glands are attached to hair follicles, and the size of the gland varies inversely with the diameter of the associated hair.
- A large-diameter hair has a small gland and vice versa.
- These are true holocrine glands, in that a gland in which the secretion is formed by the degeneration of the entire glandular cell.
- They open to the surface of the skin by way of the pilosebaceous canal.
- This holocrine type of gland has multiple acinar components. The acinus of each gland converges toward a common excretory duct.
Function
- Sebum helps to keep the hair soft and pliable and gives it a shiny appearance.
- It provides some waterproofing on the surface of the skin and acts as a bactericidal and fungicidal agent, preventing infection.
- The sebum also prevents drying and cracking of the skin, especially on exposure to heat and sunlight.
iii. Ceruminous Gland
- Ceruminous glands are modified apocrine glands, which together with sebaceous glands, produce the yellowish‐brown wax secretion called cerumen or ear-wax.
- The ceruminous glands in humans are located in the cartilaginous section of the external auditory canal with the number ranging from 1,000 and 2,000 ceruminous glands in the normal ear.
Structure
- The ducts of the coiled tubules of the ceruminous gland pass through the dermis to empty into a hair follicle or onto the epidermal surface.
- The coiled ceruminous gland has a large lumen, and the cells are either cuboidal (inactive) or columnar (active).
- The gland is lined by a layer of secretory cells present on the myoepithelial cells.
- The secretion is first drained into respective ducts of the glandular cells which then flows into larger ducts and finally at the base of guard cells present in the auditory canal.
Function
- Cerumen plays an essential role in the protection of the ear canal against physical damage and microbial invasion.
- The pH of the ear canal is maintained by the secretions around 5.7 in the inner/medial aspects of the canal.
iv. Mammary glands
- Characteristic of mammals, these are compound tubular glands that produce milk during lactation period for feeding the young ones.
- These glands are present in all mammals and are rudimentary and non-functional in men.
- In humans, these glands develop at puberty by the action of growth hormone and estrogen; however, in other primates, breast development usually happens after the pregnancy.
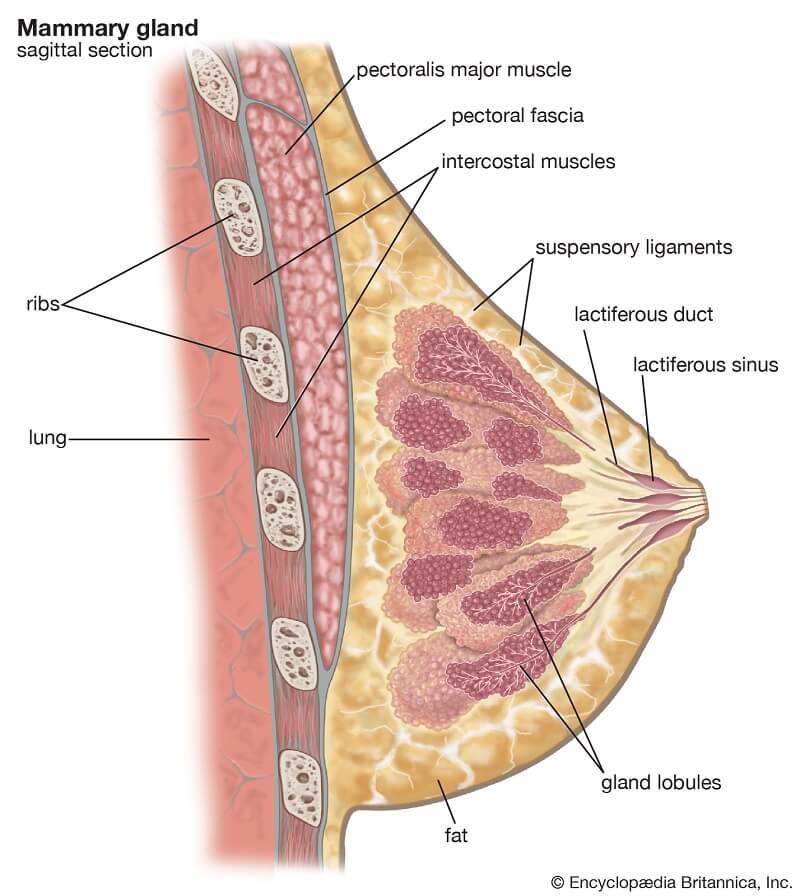
Image Source: Encyclopædia Britannica, Inc.
Structure
- Mammary glands are, structurally, tear-shaped, and are composed of glandular tissue, fibrous tissue, fatty tissue, and blood supply.
- An adult female breast consists of around 20 lobes of glandular tissue where each lobe is made up of several lobules that radiate around the nipple.
- Each of these lobules is composed of a group of alveoli that terminate into small ducts, which collectively form large excretory ducts called lactiferous ducts.
- These ducts, supported by the dense connective tissues, converge towards the center of the breasts to form reservoirs (also called lactiferous sinus) of milk. From each of these sinuses, a single duct arises that opens into the nipple.
Function
- The primary function of mammary glands is to provide nourishment to the infant through breastfeeding.
- In addition to their primary function of providing nutrients to the infant, breasts also have social and sexual prominence.
- Breasts, and especially the nipples, are an erogenous zone.
b. Hair and Hair follicles
- Hairs are characteristic of mammals. They may cover the entire body or may be reduced to patches or scattered hairs.
- Hairs are the cornified epidermal products of the integument.
- All the hairs on the surface of the skin are periodically lost by molting and are replaced by new sets of hairs.
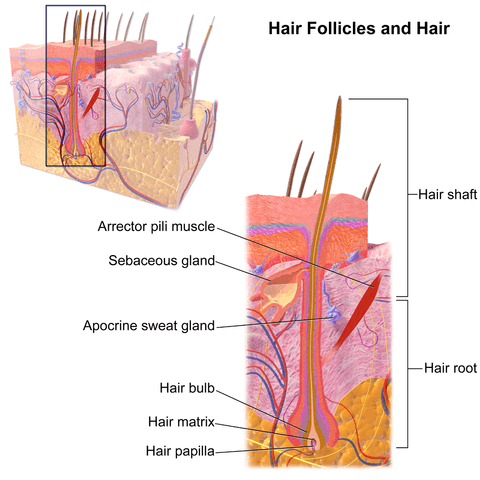
Image Source: Blausen.com staff (2014). “Medical gallery of Blausen Medical 2014”
Structure
- Each hair originates from the bottom of a tubular invagination, or hair follicle, of the germinative layer of the epidermis into the dermis.
- A cluster of cells called the hair papilla or bulb is present at the base of the follicle.
- The hair is formed by the division of cells of the bulb, and they become keratinized when the old cells are push upwards, away from their source of nutrition.
- The part of the hair above the skin is called the shaft while the remainder is termed the root.
- Typically, the hair shaft consists of three layers: an external cuticle made up of overlapping microscopic scales, the middle cortex containing shriveled cells and pigments, and an inner medulla containing air spaces in larger hairs.
Functions
- The chief functions of hairs seem to serve for insulation of body and as sensitive tactile organs (e.g. vibrissae in rabbits).
- Hairs also function in the regulation of body temperature, and the facilitation of evaporation of perspiration.
Hair and Hair Follicle Video Animation
https://www.youtube.com/watch?v=i3W3f38ZpJo
c. Nails
- Human nails are equivalent to the claws, horns, and hooves of animals.
- Derived from the same cells as epidermis and hair these are hard, horny keratin plates that protect the tips of the fingers and toes.
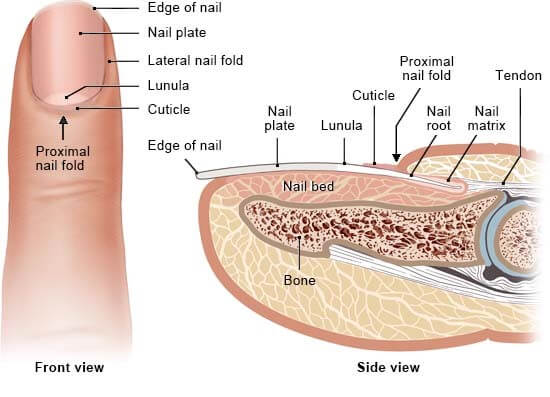
Image Source: InformedHealth.org.
Structure
- The nail organ consists of epithelial and connective tissue parts.
- The nail consists of the nail matrix that produces the nail plate and is mostly under the proximal nail wall and the nail bed epithelium, which ensures firm adhesion to the dermis of the nail bed.
- The root of the nail is embedded in the skin and covered by the cuticle, which forms the hemispherical pale area called the lunula.
- The nail plate is the exposed part that has grown out from the nail bed.
Functions
- The primary function of the nail is to protect the fingertip and the surrounding soft tissues from injuries.
- Nails also exert a counter-pressure that aids in the precise movement and touch sensitivity.
Structure and Functions of Nail Video Animation

Physiology of the Integumentary System
Development of skin color (Skin Pigmentation)
- The skin color in humans is determined by different pigments like melanin, carotene, and hemoglobin.
- Among all the pigments, melanin is the most crucial pigment for skin coloration and is formed only in the cytoplasm of the melanin-forming cell, the melanocyte.
- Melanin exists in two forms; eumelanin which gives the black and brown color and pheomelanin which gives red coloration.
- In general, there are more melanocytes per square millimeter on exposed skin than on covered areas. However, there is a high density of melanocytes about the genitalia and the nasal mucous membranes.
- Variations in skin color between racial groups and possibly between different individuals of the same race are a function of the rate and amount of melanin production by melanocytes rather than the number of melanocytes present.
- These are dendritic or branched cells that are found at the epidermal-dermal junction of the skin and mucous membranes.
- These dermal melanocytes reach the epidermis and become epidermal melanocytes. Melanocytes remaining down in the dermis in the human being gradually become inactive.
- On exposure to the UV radiation of the sun, the keratinocytes are stimulated to release chemicals which, in turn, stimulate the melanocytes to produce melanin.
- The melanin produced in the melanocytes is then transferred to the keratinocytes via a cell organelle called melanosome, which results in the accumulation of melanin in the keratinocytes.
- Melanosome contains a copper-containing enzyme called tyrosinase which catalyzes the synthesis of melanin from tyrosine.
- The accumulation of melanin results in the darkening of the skin. After the exposure to the sun, it takes about ten days for melanin synthesis to the peak.
- Similarly, as new skin is formed, epidermal cells move outward to become the stratum corneum, and the melanin granules contained within them are carried along and appear in the stratum corneum not as granules any longer but as fine irregular pigmented particles.
Hair Growth
- Hair is a component of the integumentary system and extends downward into the dermal layer where it sits in the hair follicle.
- Similar to the skin, hair forms by rapid division and differentiation of stem cells which form keratinocytes that migrate, flatten, and die, forming keratinized cells.
- The final hair product that is exposed on the surface of the skin will be composed entirely of keratin.
- The growth of the hair follicle is cyclical. This cycle can be divided into three phases: anagen(growth), catagen (transition), and telogen (rest).
- Anagengrowth is the active phase in which the hair follicle takes on its onion-like shape and works to produce the hair fiber. About 85–90% of all scalp hairs are in anagen.
- The synthesis of the hair shaft and pigmentation only takes place in the anagen phase. The axial symmetry within the hair bulb decides the curvature of the final hair structure.
- By the end of anagen, the mitotic activity of the matrix cells is reduced, and the follicle enters a highly controlled involuntary phase known as catagen.
- Catagen lasts approximately two weeks in humans, and during this phase, the proximal part of the hair shaft becomes keratinized and forms the club hair. In contrast, the distal portion of the follicle loses 1/6th of its diameter by apoptosis.
- The telogen stage is the duration between the completion of catagen and the onset of the next anagen phase.
- Telogen stage lasts for 2–3 months and approximately 10–15% of all hairs in the scalp are in this stage.
- In the telogen stage, the hair shaft is transformed into club hair and finally shed.
- This phase lasts until anagen initiating signals from the dermal papilla stimulates the hair germ to show enhanced proliferative and transcriptional activity, leading to the initiation of anagen.
Nail growth
- The nail is the most significant skin appendage. It grows continuously through life in a non-cyclical manner; its growth is not hormone-dependent.
- The nail of the middle finger of the dominant hand grows fastest with approximately 0.1 mm /day, whereas the big toenail grows only 0.03-0.05 mm /day.
- The nails’ size and shape vary characteristically from finger to finger and from toe to toe, for which the size and shape of the bone of the terminal phalanx are responsible.
- The nail is a continuously and lifelong growing keratin plate that is biochemically identical to the hair shaft.
- The growth of nails occurs via extrusion, meaning that new growing cells are added to the base while the old cells are pushed outward to the fingertips.
- The keratin in the old cells becomes harder, and ultimately the cells become dead and just hardened structures.
- Some of the living cells are still present on the nail at the base in the form of the white moon-like lunula.
- The cell growth occurs mostly in the germinal matrix in the nail bed.
- The cells that provide shine to the nail surface are added on top of the nail fold.
- With the growth of the nail, it is forced into the concave structure.
Functions of the Integumentary System
The integumentary system of vertebrates is genuinely a ‘jack-of-all-trades’ since it performs several essential functions, some of which are:
Protection
- The integument or skin separates the animal from its external environment and helps to maintain a constant internal environment.
- The inflammatory cells in the skin provide defense against intruding antigens.
- The pigment melanin protects against harmful ultraviolet rays in sunlight.
- The lipid and oil-like secretion of different glands acts as another barrier against chemicals and also prevent heat loss.
Thermoregulation
- The average body temperature is maintained by the action of sweat glands as well as the hair on the skin of mammals.
- Evaporation of watery perspiration from the skin helps to cool and regulate body temperature in hot environments.
- Similarly, the hair also aids in the regulation of body temperature, and facilitation of evaporation of
- For the elimination of heat, integumentary blood vessels dilate so that skin becomes a radiator whereas, for the conservation of heat, the vessels constrict.
Excretion
- The secretion of sweat and sebaceous glands contains some amount of urea and other ions that aid in excretion. Excess vitamin B is also removed in the form of sweat.
- The skin is a minor excretory organ for some substances, especially when kidney function is impaired and aromatic substances, e.g. garlic and other spices.
Formation of Vitamin D
- A lipid-based substance, 7-Dehydrocholesterol, in the skin is converted to vitamin D by sunlight.
- This vitamin is used in the formation and maintenance of bone, along with calcium and phosphate.
Cutaneous Sensation
- There are sensory receptors in the dermis that are sensitive to touch, pressure, temperature, or pain.
- The stimulation generates nerve impulses in sensory nerves that are transmitted to the cerebral cortex.
Absorption
- Skin is capable of absorbing some substances which include some drugs, hormone replacement therapy during the menopause, and nicotine as an aid to smoking cessation in transdermal patches and some toxic chemicals like mercury.
Integumentary System Diseases
Bacterial infection
Impetigo
- Impetigo is a highly infectious bacterial infection commonly caused by Staphylococcus aureus.
- It begins with superficial pustules, usually around the nose and mouth. It is spread by direct contact and is common in children and immunosuppressed individuals.
Cellulitis
- Cellulitis is a spreading infection caused by some anaerobic bacteria, including Streptococcus pyogenes and Clostridium perfringens that enter through a cut in the skin.
- Their spread is facilitated by the formation of enzymes that break down the connective tissue that generally isolates an area of inflammation.
- If untreated, the bacteria may enter the blood, causing septicemia.
Fungal Infection
Ringworm and tinea pedis
- These are superficial skin infections.
- In ringworm infection, there is an outward spreading ring of inflammation, which mostly affects the scalp, feet, and groin and is easily spread to others.
- Tinea pedis (athlete’s foot) affects the skin between the toes.
Viral Infection
Human papillomavirus (HPV)
- HPV causes warts or verrucas that are spread by direct contact. This creates a proliferation of the epidermis and development of a small firm growth, which is nearly always benign.
Herpesviruses
- Rashes seen in chickenpox and shingles are caused by the herpes zoster virus.
- Other herpes viruses like HSP1 and HSP2 cause cold sores and genital herpes, respectively.
Inflammatory diseases
Eczema (Dermatitis)
- Eczema is a common inflammatory skin disease that may be either acute or chronic.
- Acute dermatitis is characterized by redness, swelling, and exudation of serous fluid usually accompanied by pruritus (itching) and finally leading to crusting and scaling.
- In the case of chronic conditions, the skin thickens and may become leathery due to longterm scratching, which may cause infection.
Acne vulgaris
- Acne is commonest in adolescent males and is thought to be caused by increased levels of testosterone after puberty.
- This is caused when the sebaceous glands (in hair follicles) become blocked and then infected, leading to inflammation and pustule formation.
Malignant tumors
Basal cell carcinoma
- Basan cell carcinoma is the least malignant and most common type of skin cancer.
- This tumor is associated with long-term exposure to sunlight and is, thus, most likely to occur on sun-exposed sites, usually the head or neck.
- Cancer appears as a shiny nodule, and later this breaks down, becoming an ulcer with irregular edges, commonly called a rodent ulcer.
Malignant melanoma
- Malignant melanoma is a malignant proliferation of melanocytes, usually originating in a mole that enlarges and may have an irregular outline.
- The melanocytes may ulcerate and bleed and are observed most commonly in young and middle-aged adults.
- This tumor develops as a result of recurrent episodes of intensive exposure to sunlight, including repeated episodes of sunburn, especially in childhood.
Integumentary System Video Animation (Bozeman Science)

References
- Nagarajan P. (2018). Ceruminous Neoplasms of the Ear. Head and neck pathology, 12(3), 350–361. https://doi.org/10.1007/s12105-018-0909-3
- Stoeckelhuber, M., Matthias, C., Andratschke, M., Stoeckelhuber, B.M., Koehler, C., Herzmann, S., Sulz, A. and Welsch, U. (2006), Human ceruminous gland: Ultrastructure and histochemical analysis of antimicrobial and cytoskeletal components. Anat. Rec., 288A: 877-884. DOI:1002/ar.a.20356
- Hoover E, Alhajj M, Flores JL. Physiology, Hair. [Updated 2019 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499948/
- Bilgen Erdoğan (May 3rd 2017). Anatomy and Physiology of Hair, Hair and Scalp Disorders, Zekayi Kutlubay and Server Serdaroglu, IntechOpen, DOI: 10.5772/67269. Available from: https://www.intechopen.com/books/hair-and-scalp-disorders/anatomy-and-physiology-of-hair
- Volker, J.F. and Kenney, J.A., Jr. (1960), The Physiology and Biochemistry of Pigmentation. The Journal of Periodontology, 31: 346-355. DOI:1902/jop.1960.31.5.346
- Yamaguchi, Y., & Hearing, V. J. (2009). Physiological factors that regulate skin pigmentation. BioFactors (Oxford, England), 35(2), 193–199. https://doi.org/10.1002/biof.29
- LOBITZ, W. C. (1957). The Structure and Function of the Sebaceous Glands. Archives of Dermatology, 76(2), 162.DOI:10.1001/archderm.1957.01550200006002
- Patel BC, Treister AD, McCausland C, et al. Anatomy, Skin, Sudoriferous Gland. [Updated 2019 Oct 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513244/
- Waugh A and Grant A. (2004) Anatomy and Physiology. Ninth Edition. Churchill Livingstone.
- Marieb EN and Hoehn K. (2013) Human Anatomy and Physiology. Ninth Edition. Pearson Education, Inc.
- Kotpal RL(2010). Modern Textbook of Zoology Vertebrates (Animal Diversity – ii). Rastogi Publications.
- https://biologydictionary.net/integumentary-system/
Internet Sources
- 1% – https://www.ncbi.nlm.nih.gov/pubmed/29763123
- 1% – https://www.ncbi.nlm.nih.gov/pubmed/24718505
- 1% – https://www.createwebquest.com/integumentary
- 1% – https://reference.medscape.com/medline/abstract/24718505
- 1% – https://jamanetwork.com/HttpHandlers/ArticlePdfHandler.ashx?journal=derm&articleId=525114&pdfFileName=archderm_76_2_002.pdf
- 1% – https://doctorlib.info/anatomy/ross-wilson-anatomy-physiology-health-illness/14.html
- 1% – https://chnbaph.files.wordpress.com/2018/04/special-sensory-organs.pdf
- 1% – https://basicmedicalkey.com/the-skin-2/
- 1% – https://anatomypubs.onlinelibrary.wiley.com/doi/full/10.1002/ar.a.20356
- 1% – http://encyclopedia.kids.net.au/page/sk/Skin
- <1% – https://www.webmd.com/skin-problems-and-treatments/hair-loss/science-hair
- <1% – https://www.unitypoint.org/livewell/article.aspx?id=9a64f6ba-8855-44dd-82d7-fe32b00f4e06
- <1% – https://www.typesof.com/types-of-dendritic-cells/
- <1% – https://www.sciencedirect.com/topics/neuroscience/melanin
- <1% – https://www.sciencedirect.com/topics/medicine-and-dentistry/apocrine-gland
- <1% – https://www.sciencedaily.com/terms/melanoma.htm
- <1% – https://www.researchgate.net/publication/6490908_Fuchs_E_Scratching_the_surface_of_skin_development_Nature_445_834-842
- <1% – https://www.researchgate.net/publication/260949719_Melanin_Transfer_The_Keratinocytes_Are_More_than_Gluttons
- <1% – https://www.nhs.uk/conditions/acne/causes/
- <1% – https://www.ncbi.nlm.nih.gov/pubmed/7449797
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6773238/
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3904096/
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3834696/
- <1% – https://www.merckmanuals.com/home/skin-disorders/biology-of-the-skin/structure-and-function-of-the-skin
- <1% – https://www.mdpi.com/2079-9284/6/4/57/htm
- <1% – https://www.kenhub.com/en/library/anatomy/histology-of-the-sweat-glands
- <1% – https://www.healthyhairplus.com/sebaceous_glands_oily_itchy_scalp_s/4175.htm
- <1% – https://www.healthline.com/human-body-maps/mammary-duct
- <1% – https://www.health.ny.gov/diseases/communicable/athletic_skin_infections/bacterial.htm
- <1% – https://www.epainassist.com/skin/function-of-sweat-glands-and-benefits-of-sweating
- <1% – https://www.dummies.com/education/science/anatomy/the-anatomy-of-skin/
- <1% – https://www.dermnetnz.org/topics/skin-immune-system
- <1% – https://www.britannica.com/science/tuberculosis
- <1% – https://www.britannica.com/science/sweat-gland
- <1% – https://www.britannica.com/science/dermatitis
- <1% – https://www.biology-today.com/general-zoology/vertebrate-zoology/comparative-account-of-integumentary-glands-in-vertebrates/
- <1% – https://www.answers.com/Q/Where_is_the_dermis_layer_of_skin
- <1% – https://www.answers.com/Q/What_are_the_names_of_the_sensory_receptors_found_in_dermis
- <1% – https://trendydamsels.com/hair-follicle/
- <1% – https://steptohealth.com/hair-masks-shiny-silky-hair/
- <1% – https://quizlet.com/6095723/mammary-gland-flash-cards/
- <1% – https://quizlet.com/4588321/nutrition-flash-cards/
- <1% – https://quizlet.com/43673323/pathophysiology-11-221-flash-cards/
- <1% – https://quizlet.com/393251171/chapter-5-the-integumentary-system-comprehensive-medical-terminology-flash-cards/
- <1% – https://quizlet.com/296970344/exam-1-questions-1-30-flash-cards/
- <1% – https://quizlet.com/28618267/ap-exam-2-flash-cards/
- <1% – https://quizlet.com/252116291/4-flash-cards/
- <1% – https://quizlet.com/14462774/skin-aids-in-temperature-regulation-flash-cards/
- <1% – https://quizlet.com/109937090/hair-structure-flash-cards/
- <1% – https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1524-4725.2006.33039.x
- <1% – https://nailbees.com/nail-structure
- <1% – https://med.libretexts.org/Courses/Sacramento_City_College/SCC%3A_Nutri_300_(Coppola)/Text/07%3A_Vitamins/7.2%3A_Fat_Soluble_Vitamins/7.2B%3A_Vitamin_D
- <1% – https://hubpages.com/education/5-Layers-And-Cells-of-the-Epidermis
- <1% – https://healthfully.com/what-makes-nails-grow-long-strong-fast-5905995.html
- <1% – https://eprints.soton.ac.uk/58862/
- <1% – https://en.wikivet.net/Ear_-_Anatomy_%26_Physiology
- <1% – https://en.wikipedia.org/wiki/Sebaceous_gland
- <1% – https://en.wikipedia.org/wiki/Nail_matrix
- <1% – https://en.wikipedia.org/wiki/Integumentary_system
- <1% – https://en.wikipedia.org/wiki/Hair_follicle
- <1% – https://en.m.wikipedia.org/wiki/Epidermis
- <1% – https://courses.lumenlearning.com/nemcc-ap/chapter/pigmentation/
- <1% – https://askthescientists.com/skin-layers/
- <1% – https://answersdrive.com/what-is-the-main-function-of-the-hair-7576656
- <1% – https://answersdrive.com/what-is-the-function-of-a-fingernail-3754455
- <1% – https://answersdrive.com/what-are-the-functions-of-adipocytes-8544022
- <1% – https://1knews.com/anatomy-and-physiology-of-the-female-breast/
- <1% – http://www.ratbehavior.org/CoatTypes.htm
- <1% – http://basskilleronline.com/tanning-sexual-peptide-melanotan-2-information-guide.shtml
