- Two groups of E. coli are responsible for enteric disease: Enteropathogenic E. coli [EPEC] and some Shiga toxin–producing E. coli [STEC]. They both possess a cluster of virulence genes located on a chromosomal pathogenicity island called the locus of enterocyte effacement (LEE).
- The EPEC are however, defined by:
- Presence of LEE and
- Absence of Shiga toxin.
- Enteropathogenic Escherichia coli (EPEC), one of the diarrheagenic E. coli pathotypes, are among the most important pathogens infecting children worldwide because of their high prevalence in both the community and hospital setting, and because they are one of the main causes of persistent diarrhea.
- EPEC are subdivided into typical and atypical strains based on the presence or absence of the E. coli adherence factor (EAF) plasmid.
Interesting Science Videos
Disease Caused
EPEC frequently causes infantile diarrhea (outbreaks) and occasionally cause sporadic diarrhea in adults.
- It is a common cause of diarrhea in children < 5 years old, especially in developing countries.
- After rotavirus infections, EPEC is one of the leading causes of death in children in developing countries.
Mode of Transmission of EPEC
- As with other diarrheagenic E. coli strains, transmission of EPEC is fecal-oral, with contaminated hands, contaminated weaning foods or formula, or contaminated fomites serving as vehicles.
- Humans are the only source of typical strains, whereas both humans and a variety of animal hosts are reservoirs of atypical strains. Person-to-person spread is seen.
Pathogenesis of EPEC
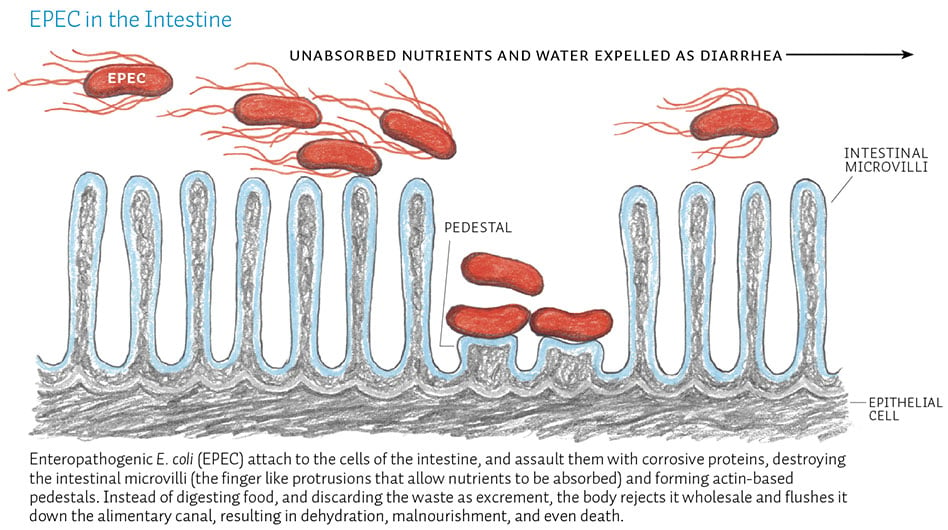
Plasmid-mediated A/E histopathology, with disruption of normal microvillus structure resulting in malabsorption and diarrhea.
- It is non-toxigenic and non-invasive.
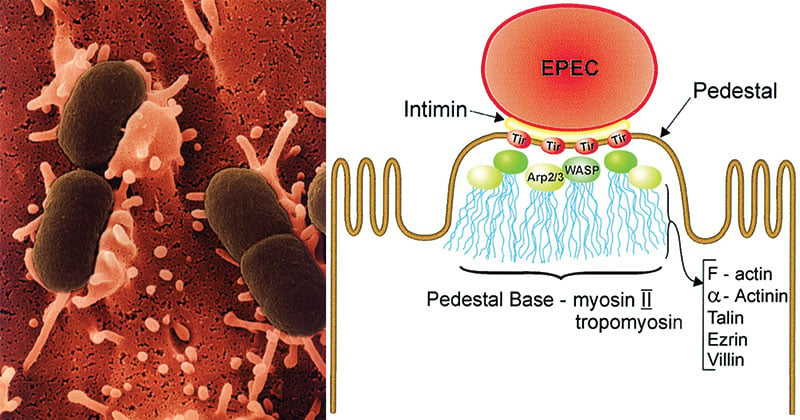
- Infection is initiated by bacterial attachment to epithelial cells of the small intestine, with subsequent effacement (destruction) of the microvillus.
- The initial aggregation of typical EPEC leading to the formation of microcolonies on the epithelial cell surface is mediated by plasmid-encoded bundle-forming pili (BFP); however, this plasmid is not present in atypical EPEC.
- The subsequent stages of attachment are regulated by genes encoded on the LEE pathogenicity island. This island of more than 40 genes is responsible for attachment and destruction of the host cell surface.
- Following the loose attachment, active secretion of bacterial proteins into the host epithelial cell occurs by the bacterial type III secretion system.
- One protein, translocated intimin receptor (Tir), is inserted into the epithelial cell membrane and functions as a receptor for an outer membrane bacterial adhesin, intimin.
- Binding of intimin to Tir results in polymerization of actin, accumulation of cytoskeletal elements beneath the attached bacteria, loss of cell surface integrity, and eventual cell death.
- Formation of A/E lesions (attaching and effacing lesions): These are typical lesions produced on the intestinal epithelium which leads to disruption of brush border epithelium causing increased secretion and watery diarrhea.
Clinical Features and Complications of EPEC
Disease occurs primarily in children younger than 2 years and is characterized by:
- Watery diarrhea
- Non-bloody stools
- Vomiting
- Fever
Watery diarrhea may be severe and protracted. The onset of disease may be as rapid as a few hours after ingestion of EPEC.
Although most infections resolve after a few days, persistent diarrhea requiring hospitalization can occur.
Diagnosis of EPEC
- Given that EPEC strains, as with other diarrheagenic E. coli strains, are defined on the basis of virulence properties, there are two approaches to the detection of EPEC in the laboratory: phenotypic and genotypic.
- The phenotypic approach requires the use of cell cultures and fluorescence microscopy, and the genotypic method requires the use of DNA hybridization or PCR.
- Attaching-and-effacing histopathology. The hallmark of infections due to EPEC is the attaching-and-effacing (A/E) histopathology, which can be observed in intestinal biopsy specimens from patients or infected animals and can be reproduced in cell culture.
- Probes and amplification assays developed for the plasmid encoded bundle-forming pili and gene targets on the “locus of enterocyte effacement” pathogenicity island.
Fecal leukocytes are seen only occasionally, but more sensitive tests for inflammatory diarrhea such as an anti-lactoferrin latex bead agglutination test are frequently positive with EPEC infection.
Treatment of EPEC
- As with other diarrheal pathogens, the primary goal of treatment of EPEC diarrhea is to prevent dehydration by correcting fluid and electrolyte imbalances.
- Oral rehydration may be sufficient for milder cases, but more severe cases require parenteral rehydration. Correction of nutritional imbalance with lactose-free formula or breast milk may be insufficient for some severely ill patients, and total parenteral nutrition may be required.
- A variety of antibiotics have been used to treat EPEC and have proved useful in many cases, but multiple antibiotic resistances are common for EPEC.
- Other therapies such as bismuth subsalicylat and specific bovine anti-EPEC milk Igs have also proven useful. There are no vaccines currently available or in clinical trials to prevent disease due to EPEC.
References
- Murray, P. R., Rosenthal, K. S., & Pfaller, M. A. (2013). Medical microbiology. Philadelphia: Elsevier/Saunders
- Parija S.C. (2012). Textbook of Microbiology & Immunology.(2 ed.). India: Elsevier India.
- Sastry A.S. & Bhat S.K. (2016). Essentials of Medical Microbiology. New Delhi : Jaypee Brothers Medical Publishers.
- Ochoa, T. J., & Contreras, C. A. (2011). Enteropathogenic escherichia coli infection in children. Current opinion in infectious diseases, 24(5), 478-83.
- https://cmr.asm.org/content/11/1/142
- https://www.amboss.com/us/knowledge/Diarrheagenic_E._coli

Nice I understood easily