Connective tissue is one of the tissue systems in animals composed of different types of cells, all of which work together to provide internal support, adhesion, and cohesion between tissues to form organs and systems. The cells of connective tissue provide a matrix that gives metabolic support to cells as well as a medium for the transport of nutrient and waste products between organs. There are different types of connective tissues that vary in density, cellularity, and specialized variants.
Interesting Science Videos
Characteristics of Connective Tissue
Connective tissues are of different types and might have different characteristics that are unique to each type. However, there are some characteristics that are common in all connective tissues. Some of such characteristics are given below:
- Connective tissues are the group of cells that work together to provide support and adhesion in order to form organs.
- All connective tissues originate from the embryonic mesenchyme or mesoderm. The mesenchymal cells have large nuclei which later differentiate to form different cells of connective tissues.
- Connective tissues are composed of cells and an extracellular matrix. The extracellular matrix consists of protein fibers and ground substances.
- Connective tissues are found in and around body organs and help connect the organs or diffuse nutrients and waste materials between the organs.
- Connective tissues are classified into different types on the basis of differences in composition and the concentration of cells, fibers, and ground substance.
- Connective tissue is highly vascular, except for cartilage, as it is provided with a large number of blood vessels for the transport of nutrients, oxygen, water, and waste materials.
Structure of Connective Tissue
- Connective tissues are composed of cells and the extracellular matrix. The cells are of different types and determine the type of connective tissues.
- The extracellular matrix of the connective tissues is composed of ground substance and fibers.
- It is present between the widely spaced cells that are often suspended in the ground substance. The matrix is responsible for the specific structure and function of the tissues as the matrix of bone is rigid and inflexible, but that of cartilage is firm but pliable.
- The extracellular fibers of the matrix are secreted by the connective tissue cells and are responsible for the functional properties of the tissue.
- The ground substance is a clear, colorless, and viscous fluid that fills the space between the cells and the fibers.
- The ground substance is composed of proteoglycans and cell adhesion proteins. The ground substance is responsible for the adhesion function of the connective tissue.
- The ground substance also served as a molecular sieve that can travel between blood capillaries and the cells, thus helping is the movement of nutrients, oxygen, and waste materials between the two.
- The cells and fibers of connective tissues are of different types and perform different functions.
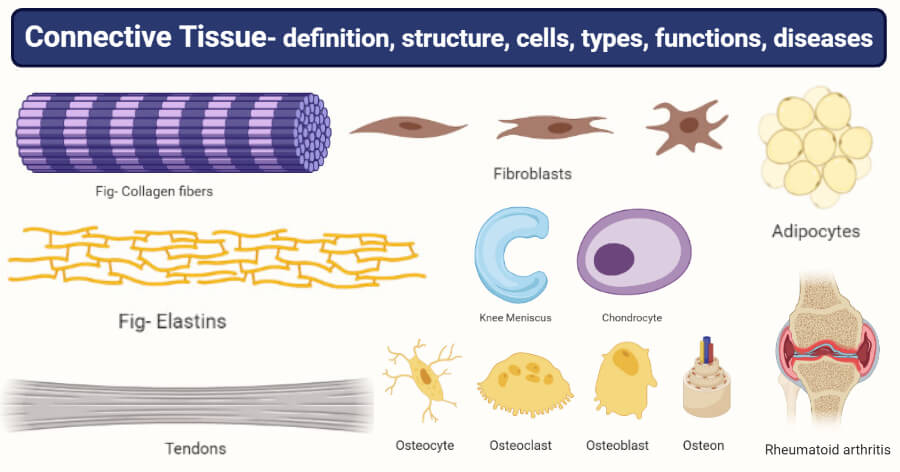
Connective tissue fibers
- Connective tissue fibers are elongated proteins that polymerize to both fibrous components of the tissue after secretion from fibroblasts.
- These fibers remain embedded in the extracellular matrix between the connective tissue cells—these function to strengthen and support the connective tissues.
- There are three different types of connective tissue fibers; collagen, reticular and elastic fibers. The proportion of each fiber in different connective tissue might differ, and the predominant fiber determines the characteristics of the tissue.
1. Collagen fibers
- Collagen fibers are composed of collagen protein which is the most abundant protein in the human body.
- Collagen fibers are defined by their ability to form extracellular fibers, sheets, and networks with strong resistance to normal shearing and tearing forces.
- Collagens are secreted by fibroblasts and several other cell types distinguished by their molecular composition, morphological characteristics, and distribution.
- Collagen fibers occur in bundles that add to the great tensile strength and flexibility. In collagen fibers, fibrillar collagens are present that form large eosinophilic bundles.
- These fibers densely fill the connective tissue matrix, forming structures like tendons, organ capsules, ligaments, and even the dermis.
- During the synthesis of collagen fibers, initial procollagen α chains are formed which are then selected, aligned, and stabilized by disulfide bonds at the carboxyl terminals, folded as a triple helix structure.
- The triple helix is then cleaved to form rod-like procollagen molecules that form the basic subunit of the collagen fibers.
- Depending on the composition of procollagen α chains, different collagen has different structures and functions.
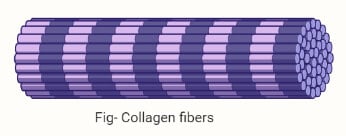
2. Elastic fibers
- Elastic fibers are smaller than collagen fibers and form a sparse network in between collagen bundles in some tissues that are subject to regular stretching or bending.
- Elastic fibers have rubber-like properties that allow the fibers to be stretched and return to their original shape.
- Elastic fibers commonly occur in the stroma of the lungs, the walls of large blood vessels, mostly arteries, and skin.
- An elastic fiber consists of molecules of protein elastin which is surrounded by a glycoprotein named fibrillin.
- Both the proteins are secreted by fibroblasts beginning with the secretion of microfibrils onto which elastin protein is deposited.
- The elastic property of elastic fibers is due to the structure of the elastin subunits and the cross-links holding them together.
- The elastin molecules have lysine-rich regions that are interspersed with hydrophobic domains rich in lysine and proline which are responsible for extensible, random-coil conformations.
3. Reticular fibers
- Reticular fibers are composed of collagen proteins arranged in bundles with an outer coating of glycoprotein, commonly found in the wall of blood vessels and forms a network around the cells in some tissues.
- Reticular fibers consist of collagen Type III which forms an extensive network of thin fibers that supports various cells.
- These are also produced by fibroblasts and usually occur in the reticular lamina of the basement membranes and surround cells like adipocytes, smooth muscle cells, and nerve fibers.
- The reticular fibers are much thinner than collagen fibers and usually occur in the form of branching networks.
- Reticular networks are delicate and occur abundantly in the stroma of hemopoietic tissue, the spleen, and lymph nodes.
Connective Tissue Cells
- Connective tissue consists of cells that are often characteristic of a particular type of connective tissue.
- All of these cells are developed during the embryonic life from the mesenchyme of the mesodermal layer of the embryonic germ layers.
- The cells of the mesenchyme have the ability to differentiate along different lines depending on the local condition of the body.
- In adults, it is believed that some number of mesenchymal cells persist in the walls of blood vessels that retain the capacity to differentiate into different connective tissue cells as the need arises.
- The cells of connective tissues are of two types; fixed or stationary or resident cells and transient or motile or wandering cells.
A. Fixed cells (or resident cells)
- Fixed or resident connective tissue cells are the cells that originate from local mesenchyme and are permanent residents of connective tissues.
- The following are the two types of resident connective cells;
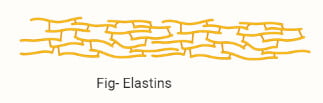
1. Fibroblasts

- Fibroblasts are the most abundant and common cells of connective tissue that is present in all the general connective tissues.
- Fibroblasts are large cells with irregular processes that produce most of the extracellular components of the connective tissues.
- Fibroblasts secrete essential proteins like collagen, elastin, as well as other glycoproteins that comprise the ground substance of the extracellular matrix.
- Fibroblasts are active cells, whereas the quiescent cells are termed fibrocytes, fibroblasts consist of irregularly branched cytoplasm with rough endoplasmic reticulum and well developed Golgi apparatus.
- Fibroblasts are mostly active in tissue repair where they bind cut surfaces by forming granulation tissue after tissue destruction.
2. Adipocytes

- Adipocytes, also called fat cells, are derived from large mesenchymal cells and are specialized for cytoplasmic storage of lipids.
- These cells occur in many types of connective tissue in small numbers but are most abundant in adipose tissues.
- Adipocytes receive glucose from the blood, which is then converted into lipid. The lipid is accumulated in the cytoplasm of the cell as a large oil droplet.
- Adipocytes are of different shapes and sizes according to the amount of fat they store, but they have major metabolic significance and considerable medical importance.
B. Transient cells (or wandering cells)
- Transient or wandering cells are free cells that are present in the interstices of loose connective tissues and can migrate through the extracellular spaces.
- The following are four transient cells found in connective tissues;
1. Macrophages
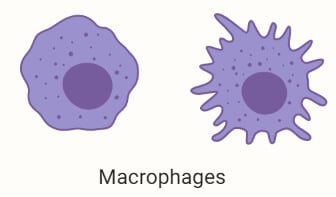
- Macrophages are irregularly shaped cells with granules in the cytoplasm that have the phagocytic ability and are specialized in the turnover of protein fibers and removal of dead cells and tissues.
- The shape and size of macrophages vary according to their state of functional activity, but they typically measure between 10 to 30 µm in diameter with a centrally placed kidney-shaped nucleus.
- These are found in the connective tissue of most organs and are often referred to as histiocytes.
- Macrophages are derived from bone marrow precursor cells called monocytes that cross the epithelial wall of blood vessels, reach the connective tissue, and differentiate to form phagocytic cells.
- Macrophages are important cells of the immune system as they play an important role in the early stages of repair and inflammation after tissue damage.
2. Mast cells
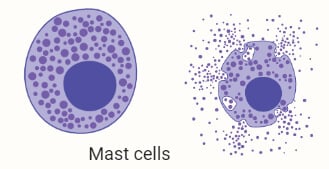
- Mast cells are oval cells that are between 7-20 µm in diameter with basophilic secretory granules in the cytoplasm.
- Mast cells usually occur in loose connective tissue in the fibrous capsule of organs like the liver and spleen.
- The granules in the cytoplasm contain heparin and histamine that are released when the cells are damaged by injury.
- Besides, these cells also release other bioactive substances that are essential in a local inflammatory response, innate immunity, and tissue repair.
- The origin of mast cells is similar to that of macrophages as these are also developed from the progenitor cells of the bone marrow.
- Mast cells occur in the connective tissue of small blood vessels, skin, and tissues of the digestive and respiratory tracts.
3. Plasma cells
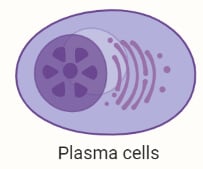
- Plasma cells are antibody-producing cells that are derived from lymphocytes.
- The cells are large, ovoid with basophilic cytoplasm rich in the rough endoplasmic reticulum and large Golgi apparatus.
- Few plasma cells are present in almost all connective tissue, and they have an average lifespan of about 10-20 days.
4. Leukocytes
- Leukocytes or white blood cells are usually found in small numbers in healthy connective tissues, but the number is significantly higher during infection.
- These cells are derived from circulating blood cells where they leave the blood and migrate to endothelial cells to enter the connective tissues finally.
- Most leukocytes remain in connective tissues for a few hours, after which they undergo apoptosis.
Types of Connective Tissue
There are different types of connective tissues with varied histological structure as a result of different combinations and concentrations of cells, fibers, and other extracellular components. The name and classification designated to different types of connective tissues denote either the structural characteristics or a major component.
Connective tissue proper
- Connective tissue proper is a type of connective tissue that is flexible and has a viscous ground substance with large proportions of fibers.
- Connective tissue proper is broadly classified as loose or dense connective tissue which refers to the amount of collagen present in the tissue.
a. Loose connective tissue
- Loose connective tissue is a common tissue that forms a layer beneath the epithelial lining of many organs and fills the spaces between the muscle and nerve fibers.
- The term loose connective tissue indicates the loose arrangement of fibers in the extracellular matrix of the tissue.
- Loose connective tissue is mostly delicate and flexible due to the limited amount of ground substance, and it is not very resistant to stress.
- Loose connective tissues are further classified into three different types;
i. Areolar connective tissue
- Areolar tissue is one of the most widely distributed connective tissues commonly found in nearly each body structure.
- This tissue consists of cells, fibers, and ground substances in roughly equal parts. The most abundant cells are fibroblasts, but other types of cells are also found in limited concentration.
- The predominant fibers in the extracellular matrix are the collagen fibers, but some amount of elastic and reticular fibers might also be present.
- Areolar tissue is distributed in areas like a subcutaneous layer of skin, the papillary region of the dermis of the skin, lamina propria of the mucous membrane, and around blood vessels.
ii. Adipose connective tissue
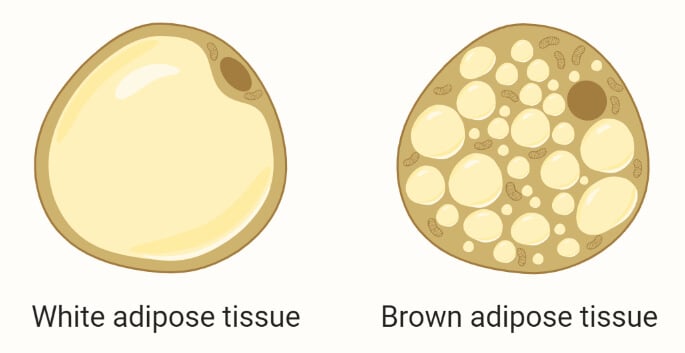
- Adipose tissue is a connective tissue composed of adipocytes that are specialized for the storage of fat in the form of oil droplets.
- Adipose tissue makes up about 15-20% of the total body weight in men and somewhat more in women.
- In addition to serving as storage deposits for fat, adipose tissue also functions as a key regulator of the body’s energy metabolism. The tissue is also an excellent source of stem cells that are essential in the repair and replacement of damaged tissue.
- Adipose tissues have a rich supply of blood vessels and unlike other connective tissues, are surrounded by a thin external lamina containing type IV collagen.
- There are two types of adipose tissue with different structures, colors, and functions; white adipose tissue and brown adipose tissue.
- White adipose tissue is the more common type of adipose tissue that is specialized for fat storage. The tissue consists of adipocytes, each of which contains a large cytoplasmic droplet of whitish-yellow fat.
- The brown adipose tissue consists of adipocytes with multiple lipid droplets that are interspersed among the mitochondria of the cell. The presence of multiple droplets results in a darker appearance.
- The brown adipose tissue is involved in the release of heat and functions to maintain the temperature of the blood.
iii. Reticular connective tissue
- Reticular tissue is defined by the presence of abundant reticular or Type III collagen fibers that form a delicate network to support various cells.
- Reticular tissue consists of the protein reticulin produced by modified fibroblasts often termed as reticular cells.
- The extracellular matrix of the tissue consists of loose deposition of glycosylated reticular fibers that form a network of microenvironments for cells in hemopoietic tissue and lymphoid organs.
- Reticular tissues are found in the stroma of the liver, spleen, lymph nodes, bone marrow, and the reticular lamina of the basement membrane.
b. Dense connective tissue
- Dense connective tissue is another type of connective tissue proper that contains more fibers and the fibers are thicker and more densely packed with considerably fewer cells than in loose connective tissue.
- Dense connective tissue provides strength to the tissue, and the tissue is less flexible.
- Dense connective tissue is further classified into three types;
i. Dense regular connective tissue
- Dense regular connective tissue consists of Type I collagen bundles and fibroblasts arranged in parallel to provide resistance to repeated stresses from the same direction.
- The tissue consists of a shiny white extracellular matrix with dead fibroblast cells and fibers.
- As the cells are dead, damaged tendons and ligaments require a long period of time for healing.
- These tissues are found in tendons, most ligaments, and aponeuroses and have the primary function of providing strength and strong attachment between structures.
ii. Dense irregular connective tissue
- Dense irregular connective tissue consists of collagen fibers that are randomly interwoven with no definite orientation.
- The three-dimensional collagen network in the dense irregular connective tissue provides resistance against stress.
- The tissue is found in different areas like the deep dermis layer of skin and capsules of most organs.
iii. Elastic connective tissue
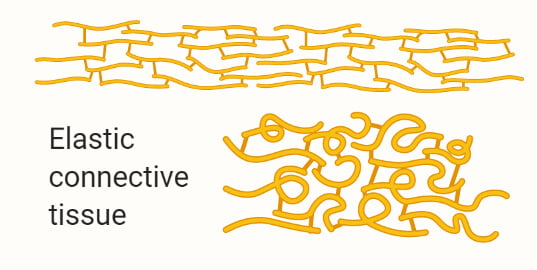
- Elastic connective tissue consists mainly of elastic fibers in the extracellular matrix, which provides considerable extension and recoil to the tissue.
- The tissue is composed of few cells and a large number of elastic fibers secreted by fibroblasts.
- Elastic tissue is found in structures where stretching or change in shape is required, like the lungs and large blood vessels.
Special connective tissue
A. Cartilage
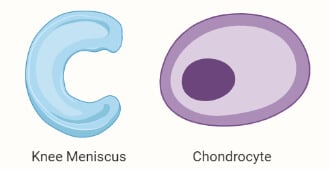
- Cartilage is a tough supporting connective tissue that is characterized by the extracellular matrix with a high concentration of proteins, proteoglycans, and fibers secreted by chondrocytes.
- Cartilage consists of a dense network of collagen fibers and elastic fibers embedded in the ground substance’s gel-like component.
- The strength of cartilage is provided by the collagen fibers, and the resistance is due to the chondroitin sulfate extracellular matrix.
- Cartilage is stronger and more resilient than loose and dense connective tissues, but it doesn’t have blood or nerve supply. Chondrocytes receive nutrients from the capillaries of the surrounding tissue by diffusion.
- The resilience and the smooth, lubricated surface of cartilage provide cushioning and sliding regions within skeletal joints that facilitate bone movement.
- Cartilage consists of cells called chondrocytes and no other cells. Chondrocytes alone synthesize and maintain all the components of the extracellular matrix in matrix cavities called lacunae.
- The semi-rigid consistency of cartilage is due to the water bound to the negatively charged hyaluronan and groups on proteoglycan chains. The water bound to the structure enables the cartilage to act as a shock absorber.
- Cartilage is further classified into three main groups on the basis of the composition of the matrix.
a. Hyaline Cartilage
- Hyaline cartilage is the most common cartilage found in animals that is homogenous and semitransparent when fresh.
- The extracellular matrix of hyaline cartilage is homogenous with type II collagen and aggrecan proteins.
- The primary connective tissue cell is chondroblasts and chondrocytes, which remain either isolated in the matrix or forms small isogenous groups.
- Collagen accounts for about 40% of the dry weight of hyaline cartilage and the collagen fibers are embedded in the hydrated gels of proteoglycans and glycoproteins.
- Hyaline cartilage is found in the articular surfaces of movable joints, in the walls of larger respiratory passages, and in the ventral ends of ribs.
- Hyaline cartilage forms the temporary skeleton in the embryonic stage which is then replaced by bone.
- Hyaline cartilage is covered with a perichondrium except at the epiphyses and articular cartilage.
b. Elastic Cartilage
- Elastic cartilage is similar to hyaline cartilage in structure except for abundant networks of elastic fibers and collagen and aggrecan.
- The structure of elastic cartilage consists of elastic fibers lying in the solid matric with chondrocytes lying between the fibers.
- The chondrocytes are distributed in the matrix in the form of small isogenous groups.
- Elastic cartilage is more flexible than hyaline cartilage due to the presence of elastic fibers that provides flexibility in the movement of the cartilage.
- Elastic cartilage is found in different areas of the body like the auricle of the ear, walls of the external auditory canal, the epiglottis, and the upper respiratory tract.
- Like hyaline cartilage, elastic cartilage also contains an outer perichondrium.
c. Fibrocartilage
- Fibrocartilage is found in different forms in different structures, and its structure lies somewhere between the hyaline cartilage and the dense connective tissue.
- The extracellular matrix of fibrocartilage is composed of dense masses of white collagen fibers that are secreted by the chondrocytes.
- The chondrocytes occur either singly or in aligned isogenous aggregates in the matrix along with other extracellular matrix components.
- Fibrocartilage does not have an outer covering of the perichondrium, but the structure of fibrocartilage is essentially a mixture of hyaline and dense connective tissue.
- Fibrocartilage is found in the intervertebral discs of the spinal column, pubic symphysis, and portions of tendons.
B. Bone
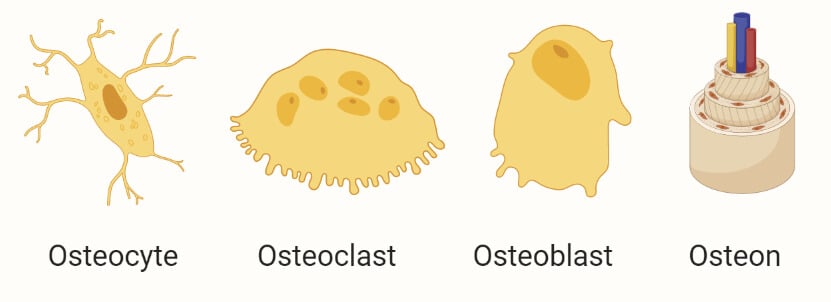
- Bone is a specialized connective tissue composed of a calcified extracellular matrix and osteocytes.
- The matrix of bone tissue is calcified and the movement of nutrients and other substances between osteocytes and blood capillaries through a thin cylindrical space of the canaliculi.
- The matrix is composed of about 15% water, 30% collagen fibers and 55% crystallized mineral salts. The most abundant mineral salt is calcium phosphate, followed by calcium hydroxide.
- The hardness of bone depends on the crystallized inorganic mineral salts, whereas the flexibility of the bone depends on the collagen fibers.
- The cells of the bone tissue are of three types; osteocytes, osteoblasts, and osteoclasts.
- Osteoblasts are found in lacunae between the bone matrix with cytoplasmic processes in small canaliculi.
- Osteoblasts are growing cells that synthesize and secrete the organic component of the matrix.
- Osteoclasts are giant, multinucleated cells that are involved in the removal of calcified bone matrix.
- The osteoblasts produce various components of the bone matrix, including Type I collagen fibers, proteoglycans, and matricellular glycoproteins.
- The activity of osteoblast is regulated by osteoclast cells which remove the calcified matric components.
- Depending on the size and distribution of the spaces in the matrix, regions of the bone can be either compact or spongy.
- Compact bone tissue contains few spaces and is the strongest form of bone tissue. Spongy bone tissue has numerous spaces with some spaces filled with red bone marrow.
C. Blood
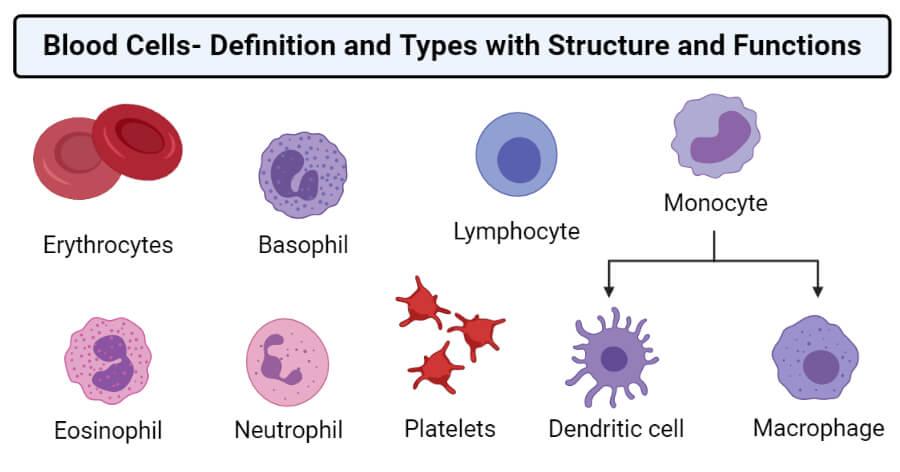
- Blood is a specialized fluid connective tissue consisting of cells and extracellular fluid material called plasma.
- The plasma is an aqueous solution that makes up about 55% of the total volume of blood. It consists of water, nutrients, respiratory gases, nitrogenous waste products, and hormones.
- Important plasma proteins are albumin and globulins that are important in the maintenance of osmotic pressure of the blood and the transport of various materials.
- Blood cells comprise most of the composition of blood and are synthesized by the red bone marrow.
- Three different types of cells occur in the blood; red blood cells, white blood cells, and platelets.
- The cells are formed in the bone marrow, and these originate from stem cells followed by their maturation into different types of cells.
- The concentration of different blood cells in blood differs from the condition of the body and the individual’s age.
- The primary function of blood is the transport of respiratory gases and nutrients from one cell to another.
Other Types
a. Fibrous connective tissue
- Fibrous tissue is mainly composed of closely packed bundles of collagen fibers, and the structure of the tissue is similar to that of dense connective tissue.
- Few fibrocytes are present in rows between the bundle of fibers, and the tissue is commonly found in ligaments, periosteum, and outer covering of other organs like the kidney and the brain.
- Fibrous tissue is also known as scar tissue as it is involved in the repair of damaged tissue mediated by the production of a large number of fibrocytes.
- Fibrous tissue is characterized by the presence of an interwoven network of collagen fibers in the matrix and fibrocytes.
b. Lymphoid connective tissue
- Lymphoid tissue is the tissue that makes up the lymphatic system of the body, consisting of white blood cells, bone marrow, thymus, spleen, and lymph nodes.
- Lymphoid or Lymphatic tissue is a specialized form of reticular connective tissue that contains a large number of lymphocytes.
- The extracellular matrix of lymphoid tissue is similar to loose connective tissue with scattered collagen and few elastin fibers.
Functions of Connective Tissue
- Connective tissues provide adhesion as well as the connection between different tissues and organs of the body.
- Connective tissues like bones and cartilage provide structure and internal support to different parts of the body. The skeletal system provides a framework for the body.
- These tissues also protect important organs of the body like the lungs, heart, brains, and sense organs.
- Cartilage, ligaments, and tendons help in the attachment between bones and muscles, which is important for movement.
- Blood transports respiratory gases, nutrients, and water to different cells and tissues through the body.
- Cells of connective tissue like lymphocytes, macrophages, and white blood cells are immune cells that protect the body against different forms of infections.
- Connective tissues are involved in the repair and replacement of damaged tissues.
- Adipose tissue stores a large number of fats which can then be metabolized later to produce energy.
- The adipose tissue also provides insulation in the form of a layer underneath the skin, helping in maintaining the homeostasis of the body.
Examples of Connective Tissue
Tendons
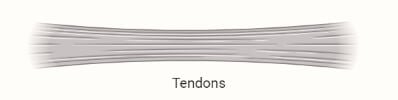
- Tendon is a fibrous connective tissue that connects muscles to bone and can withstand certain tension.
- Tendon is composed of dense connective tissue with the extracellular matrix and connective tissue cells.
- Specialized fibroblasts are found in the tendon, which is called tenocytes. The tenocytes secrete collagen fibers forming the extracellular matrix of the tissue.
- The collagen fibers are densely packed and are arranged parallel to one another in the form of fascicles.
- The fascicles are surrounded by endotendineum, which is a layer of loose connective tissue.
- The structure of tendons is similar to that of muscles, but the protein fibers present in tendons are mostly collagen fibers with few elastic fibers.
- The most important function of tendons is to create a connection between muscle and bone, which helps in the movement of bones and provides additional stability.
Lymph
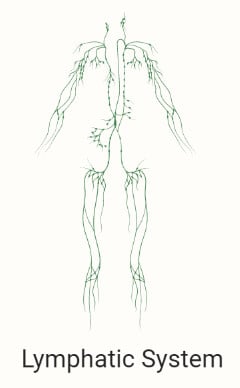
- Lymph is a fluid connective tissue that transports lymphocytes to different parts of the body.
- Lymph flows through the lymphatic system, which consists of lymph vessels and intervening lymph nodes.
- The lymph is derived from the interstitial fluid, and thus, its composition is similar to that of blood plasma.
- The lymph exchanges proteins and excess interstitial fluid with the bloodstream. It also moves the lymphocytes from the lymph nodes to other sites of the body.
- Lymph also contains chylomicrons that transport fats from the digestive system to the blood and then to other parts of the body.
Connective tissue diseases and disorders
Connective tissue disease is a condition that affects the tissue that is involved in the binding of different organs and tissues in the body. It is also known as collagenosis as the disease of connective tissue is often associated with the inflammation and weakness of collagen fibers. Many connective tissue diseases occur as a result of inflammation in tissues as a result of an immune system response. The majority of these diseases and disorders are autoimmune in nature and might even be heritable. Some of the common connective tissue diseases and disorders can be explained as;
1. Rheumatoid arthritis
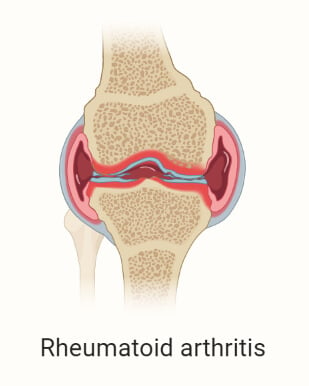
- Rheumatoid arthritis is one of the most common connective tissue diseases, which is an autoimmune disease and is heritable.
- During this disease, the immune cells attack the cells of the connective tissue, especially those present in the joints. However, it can affect other organs like the heart, lungs, and eyes.
2. Systemic Lupus Erythematosus
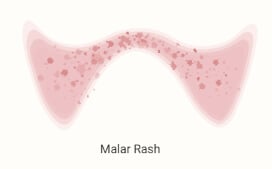
- Systemic Lupus Erythematosus is a disease of connective tissue that can cause inflammation of connective tissue present in every organ of the body.
- The most common site of inflammation during the disease include the brain, skin, blood, and lungs.
3. Scleroderma
- Scleroderma is also an autoimmune disease that causes scar tissue to form in the skin and internal organs like the gastrointestinal tract and blood vessels.
- Scleroderma is caused due to the inflammation of connective tissue cells present in the skin and epithelial tissue.
4. Mixed connective tissue disease
- Mixed connective tissue disease is a disorder where the features of various connective tissue diseases occur together or overlap.
- Some of the common diseases that make up the mixed connective tissue disease are systemic sclerosis, polymyositis, and dermatomyositis.
- The course of this disorder is chronic but milder than other connective tissue diseases. Mixed connective tissue disease is considered an intermediate stage of scleroderma or systemic lupus erythematosus.
5. Undifferentiated connective tissue disease
- Undifferentiated connective tissue disease is an autoimmune condition in which the immune system attacks its own tissues and cells.
- Undifferentiated connective tissue disease is diagnosed when the evidence of the existing autoimmune condition doesn’t meet the criteria for a specific condition.
Frequently Asked Questions (FAQs)
Question. What is connective tissue?
Answer. Connective tissue is one of the tissue systems in animals composed of different types of cells, all of which work together to provide internal support, adhesion, and cohesion between tissues to form organs and systems.
Question. Is muscle a connective tissue?
Answer. No, muscle is not a connective tissue.
Question. Is cartilage a connective tissue?
Answer. Yes, cartilage is a specialized connective tissue.
Question. What are the three main components of connective tissue?
Answer. The three main components of connective tissue are cells, protein fibers, and the ground substance. The fibers and ground substance together form the extracellular matrix.
Question. What is connective tissue disease?
Answer. A connective tissue disease is a group of conditions that affect the protein-rich tissue supporting other organs and tissues of the body.
What is the function of connective tissue?
Answer. The most important function of connective tissue is to provide internal support and adhesion to different organs and tissues of the body.
Question. What tissue connects muscles to bones?
Answer. A fibrous connective tissue called the tendon connects muscles to bones.
Question. Where are connective tissues found?
Answer. Connective tissues are found throughout the body and are present between different tissues and organs.
Question. Why is blood considered a connective tissue?
Answer. Blood is considered a connective tissue because it transports nutrients and other essential compounds throughout the body connecting different organs and systems of the body. Besides, structurally, blood consists of a closely packed extracellular matrix with blood cells.
References
- Mescher AL (2016). Junqueira’s Basic Histology. Fourteenth Edition. McGraw Hill Education. New York.
- Waugh A and Grant A. (2004) Anatomy and Physiology. Ninth Edition. Churchill Livingstone.
- Marieb EN and Hoehn K. (2013) Human Anatomy and Physiology. Ninth Edition. Pearson Education, Inc.
- Tortora GJ and Derrickson B (2017). Principles of Physiology and Anatomy. Fifteenth Edition. John Wiley & Sons, Inc.
- Kamrani P, Marston G, Jan A. Anatomy, Connective Tissue. [Updated 2020 Aug 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538534/
- Nezwek TA, Varacallo M. Physiology, Connective Tissue. [Updated 2020 Sep 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542226/
- Factor SM, Robinson TF. Comparative connective tissue structure-function relationships in biologic pumps. Lab Invest. 1988 Feb;58(2):150-6. PMID: 2448546.
- Kannus P. Structure of the tendon connective tissue. Scand J Med Sci Sports. 2000 Dec;10(6):312-20. doi: 10.1034/j.1600-0838.2000.010006312.x. PMID: 11085557.
- Stolinski, C. “Structure and composition of the outer connective tissue sheaths of peripheral nerve.” Journal of anatomy vol. 186 ( Pt 1),Pt 1 (1995): 123-30.

Notes send please