Interesting Science Videos
Introduction
- Clostridium perfringens are gram-positive rod-shaped bacteria that cause frequent foodborne diarrheal disease reported every year.
- It is one of the most commonly occurring foodborne diseases mainly in industrialized nations.
- Clostridium perfringens is ubiquitous in the environment and is pathogenic to humans as well as animals.
- Human enteritis necroticans (pigbel) is a deadly life-threatening disease that causes ulceration of the small bowel.
- Being a spore-forming anaerobic bacterium, they form C. perfringens enterotoxin (CPE) during sporulation of Type A to E associated with a different disease.
- The biological properties of CPE-producing strains induce CPE cytotoxicity.
- A rapid multiplication on a short period, the ability of vegetative cells to grow at a relatively high-temperature range, spores from harsh environmental conditions, the aerotolerant ability even though being an anaerobe are some of the biological abilities of the organism.
- Other pathogenic species are Clostridium tetani, Clostridium botulinum, Clostridium baratii, Clostridium argentinese, and Clostridium difficile.
Source of contamination of Clostridium perfringens
- The common habitat of C. perfringens is soil, water, sludge, sewage, foods mainly raw and frozen meats, contaminated equipment.
- Meat especially pork, beef and poultry products cooked with sauce are at high risk of contamination.
- Usually, school canteens, hospitals, restaurants, prisons, and gatherings are at high risk of Clostridium outbreak.
- C. perfringens is also found in the intestinal tract of humans and animals, especially in the feces of the elderly.
- C. perfringens require various amino acids and vitamins and grow well at 43-45°C, protein-rich foods such as meat are an excellent reservoir for its growth.
- In midst of heating and cooling, if the food is allowed at room temperature without adequate cooling temperature it proliferates and produces toxins.
Clostridium perfringens enterotoxins
- C. perfringens produces enterotoxin during sporulation under stressed environmental conditions.
- Fourteen different toxins and 5 enterotoxins are produced namely Type A to E.
- Clostridium perfringens also produce four types of extracellular toxins: alpha (α), beta (β), epsilon (ε), and iota (Ϊ).
- Type A CPE causes gas gangrene and antibiotic-associated infectious diarrhea in humans and enterotoxemia, necrotic enteritis, and acute gastric dilation in animals.
- Disease-associated with Type B, D and E have not yet been identified in humans but in animals, it causes enteritis and enterotoxemia.
- Type C CPE leads to necrotizing enteritis (jejunitis) in humans and enterotoxemia and necrotic enteritis in piglets, lambs, calves, and birds.
- C. perfringens also forms perfringolysin O (theta toxin) and collagenase (kappa toxin).
Epidemiology of Clostridium perfringens food poisoning
- C. perfringens outbreak has mostly occurred in the United States, Europe, and Japan with the average outbreak size being ~50 to 100.
- The factors associated with the outbreak are preparing food in large amounts, cooking without sufficient temperature (core region of the food not cooked properly), contamination in between prepared food and serving period.
- The outbreak often occurs in places where a large number of foods are prepared in advance such as hospitals and schools canteen, prisons, parties and seminars, gatherings.
- The foodborne diarrheal outbreak occurred in a mental hospital affecting 170 patients and the death of 3 patients.
- From the investigation, it was found that the source was the lamb dish cooked and stored at room temperature for 20 hours and served without reheating the meat.
- C. perfringens was isolated from the lamb meat, infected feces sample, and post mortem samples.
- Another outbreak that occurred in the school canteen was due to the consumption of C. perfringens contaminated milkshake.
- The milkshake was left at room temperature after preparation which caused 77 diarrheal cases.
Pathogensis of Clostridium perfringens
- C. perfringens causes infection only when viable cells are consumed with a portion of food containing about 107 to 109 vegetative cells per gram.
- These vegetative cells resist the stomach acid, grow, multiply and sporulate in the small intestine.
- Then a large number of CPE toxins are produced that binds to the host cell claudin protein located at the tight junction of enterocyte cells.
- It then binds to a host membrane protein and forms a CPE complex after some conformational changes.
- This causes cells to disintegrate and dissociate that damages the intestinal villi tips, shedding of epithelial cells, and shortening of villi.
- Pores form on the membrane and excess leakage of electrolytes occurs from the host cell that leads to cell lysis, decreasing the capacity of intestinal absorption and cytoskeletal collapse.
- A high concentration of CPE (>10µg/ml) causes necrosis (oncosis).
- The beta-toxin causes cytotoxic necrotic enteritis that affects the autonomic nervous system leading to hemorrhagic necrosis of the intestinal mucosa forming pores in eukaryotic membranes.
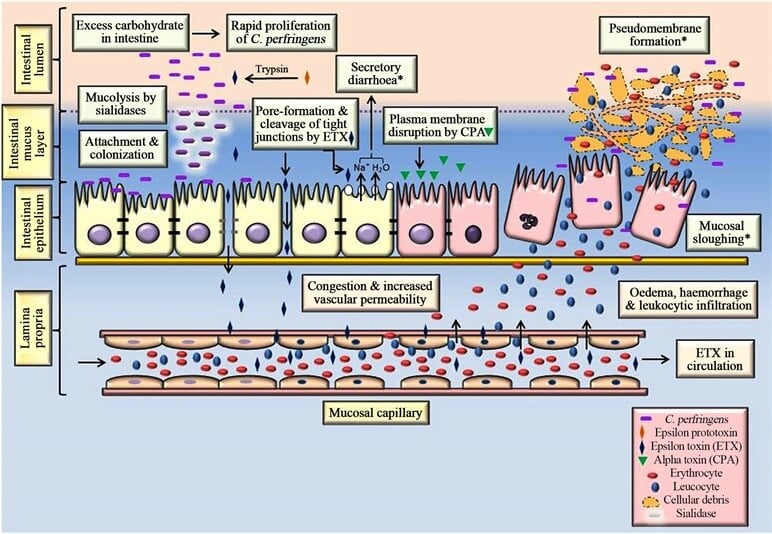
Figure: Pathogenesis of C. perfringens type D enterotoxaemia in small ruminants. Image Source: Rajveer Singh Pawaiya et al. 2020.
Disease and symptoms of Clostridium perfringens food poisoning
- The primary clinical symptoms develop after 8 to 24 hours of ingestion of heavily contaminated food.
- Common symptoms include abdominal cramps, watery diarrhea, vomiting, nausea, and fever, which usually resolves within 12 to 24 hours in most cases.
- The fatality rate is less than 0.05% but very young and elderly people, people with chronic illness are at high risk.
- The organism may invade and cause severe ulceration and eventually death of the person due to acute dehydration.
- Sudden infant death syndrome (SIDS) is also caused by C. perfringens which is associated with defects in the brain during sleep.
Lab Diagnosis of Clostridium perfringens
C. perfringens food poisoning is detected by its enterotoxin and the number of vegetative cells and spores in feces sample.
Enterotoxin assays
- C. perfringens culture is prepared in cooked meat medium and inoculated in 10ml fluid thioglycollate medium and again transferred to Duncan-strong sporulation medium where spores are observed and CPE is detected by centrifugation process.
- Biological methods such as mouse lethality and Vero cell cytotoxicity have also been used.
Immunological tests
- Single gel diffusion and double gel diffusion (Ouchterlony test) are done based on immunoprecipitation of CPE.
- Agarose gel subjected to specific antibodies is used to determine the antigen.
Counterimmunoelectrophoresis
- By using an electric field, anti-CPE antibodies are used to observe the presence of CPE as precipitation.
ELISA
- Enzyme-linked immunosorbent assay (ELISA) kits are proposed for the CPE titration.
- Protocols, as mentioned, should be followed to get an effective result.
- If the sample exhibits protease activity then the sensitivity of the IgG used for coating the polystyrene surface decreases which can be prevented by using 1% serum albumin.
Other DNA-based methods such as PCR, real-time PCR, loop-mediated isothermal amplification (LAMP), multiplex PCR, duplex PCR, and DNA-DNA hybridization methods are used to identify the strains of enterotoxigenic C. perfringens.
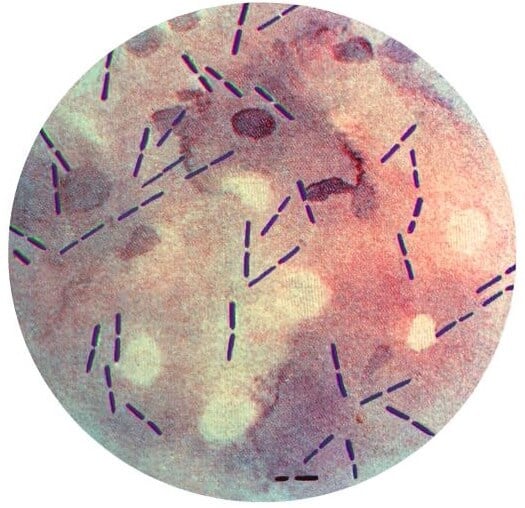
Figure: Gram stain of Clostridium perfringens. Image Source: CDC.
Treatment of Clostridium perfringens food poisoning
- The clinical course of C. perfringens food poisoning is self-limiting and requires no specific treatments.
- For treatment of antibiotic-associated and infectious diarrhea, metronidazole is recommended but other antibiotics must not be taken as it inhibits the resident microflora and produces more CPE in the colon.
- For necrotizing enteritis, rapid blood transfusion, vitamin supplements, and antibiotic treatments are suggested.
- Rehydrating drinks by oral or parenteral fluid replacement is suitable in case of dehydration.
Prevention and control measures of Clostridium perfringens food poisoning
- The best way to prevent C. perfringens food poisoning is to consume served food immediately after cooking.
- If not possible, control the time and temperature of the food during the cooking, cooling, storage, and reheating process.
- Food should be cooked in a limited amount to minimize contamination.
- Cooling should be done as soon as possible within 90 minutes and precooked food should be reheated at 70 to 100°C to kill the vegetative cells.
References
- McLauchlin, J., & Grant, K. A. (n.d.). Clostridium botulinum and Clostridium perfringens. Foodborne Diseases, 41–78.
- Popoff, M. R. (2014). CLOSTRIDIUM | Detection of Enterotoxin of Clostridium perfringens. Encyclopedia of Food Microbiology, 474–480 (https://www.sciencedirect.com/science/article/pii/B9780123847300000690)
- Miyamoto, K., & Nagahama, M. (2016). Clostridium: Food Poisoning by Clostridium perfringens. Encyclopedia of Food and Health, 149–154.
- Chukwu, E. E., Nwaokorie, F. O., Coker, A. O., Avila-Campos, M. J., Solis, R. L., Llanco, L. A., & Ogunsola, F. T. (2016). Detection of toxigenic Clostridium perfringens and Clostridium botulinum from food sold in Lagos, Nigeria. Anaerobe, 42, 176–181.
