Tuberculosis (TB) is an infectious disease caused by a group of different Mycobacterium species known as the Mycobacterium tuberculosis complex. TB is one of the most deadliest and most common infectious diseases that is held responsible for more than 1.5 million death per year and is supposed to have infected about a third of the world’s population in latent form (according to the WHO). Among these latently infected ones, about 10% are expected to develop clinical disease. Pulmonary tuberculosis caused by M. tuberculosis is the most common form of TB prevalent globally.
A specific treatment regimen is developed to treat TB. Rifampicin, Isoniazid, Pyrazinamide, Ethambutol, and Streptomycin, either in a different form of combinations of each other or in monotherapy form are used as first-line treatment. Resistant to at least rifampicin and isoniazid or all antibiotics of the first-line treatment is reported as MDR-TB.
For MDR-TB treatment, the second line of treatment was designed. The major drugs of the second line include fluoroquinolones (preferably moxifloxacin, and others like ofloxacin and levofloxacin) and injectable aminoglycosides including amikacin, kanamycin, and capreomycin. Besides, other drugs like ethionamide, cycloserine, para-aminosalicylic acid, clofazimine, linezolid, and delamind are other second-line anti-TB drugs.
If the MDR-TB pathogen is resistant to at least one fluoroquinolone and an injectable aminoglycoside, then the MDR-TB is now defined as XDR-TB. A combination of pretomanid, bedaquiline, and linezolid is recommended for treating the XDR-TB.
However, even the treatment options available for XDR-TB are now seen as resistant in many clinical isolates of the M. tuberculosis complex. The major mechanisms of resistance developed by TB pathogens are modification of target sites, overexpression of effluxes, and enzymatic modification of the drugs making them ineffective.
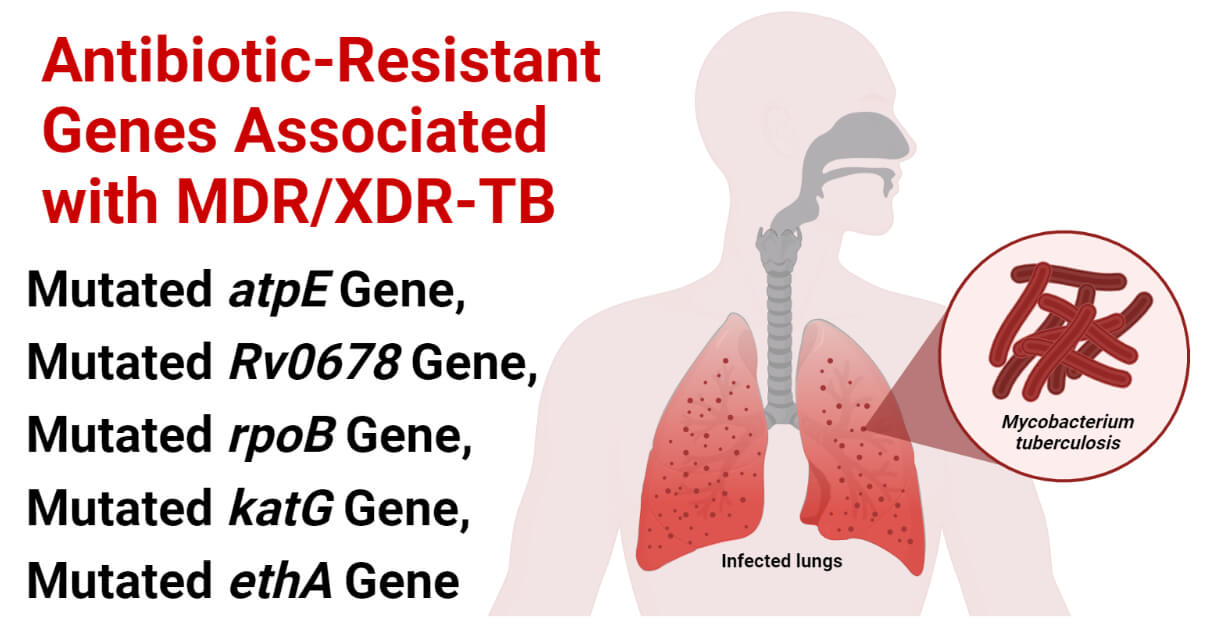
Several genes are responsible for the development of such AMR mechanism; some of the important genes responsible for drug resistance in tubercle bacilli are described in this note.
Interesting Science Videos
Mutated atpE Gene
- atpE gene is a Mycobacterium gene that encodes for the synthesis of subunit ‘C’ of the ATP synthase protein. It is present in the H37Rv genome of Mycobacterium spp. and is found in all the members of the Mycobacterium tuberculosis complex.
- The atpE gene product, subunit C of ATP synthase, is a target for a novel antimycobacterial antibiotic: bedaquiline. Bedaquiline binds to the c-subunit and inhibits the action of the ATP synthase enzyme resulting in the deficiency of energy molecules, the ATP molecules. Scarcity of the ATP molecules will result in energy deficiency for biochemical processes and eventually cause the death of the bacterium.
Mechanism of Conferring Resistance of Mutated atpE Gene
- Mutation in the atpE gene results in the synthesis of modified subunit C of the ATP synthase enzyme. Bedaquiline has a very low affinity with the modified form of subunit C and hence can’t bind with them and can’t disturb the process of ATP synthesis. This results in an increase in the MIC of bedaquiline and higher survival of the infecting Mycobacterium.
Detection Method of Mutated atpE Gene
- Complete genome analysis and PCR are the available molecular techniques that can be used to detect the mutated atpE gene. The atpE gene is first detected and amplified using PCR. After amplification, it is subjected to gene sequencing to draw its complete nucleotide sequence and the nucleotide sequence is cross-referred with the reference M. tuberculosis H37Rv genome sequence (NCBI Reference Sequence: NC_000962.3) to detect the mutation.
- Primers that can be used for the amplification of the atpE gene are:
| Primers | References |
| F: 5’- TGT ACT TCA GCC AAG CGA TGG -3’ R: 5’- CCG TTG GGA ATG AGG AAG TTG -3’ | Singh BK, Soneja M, Sharma R, Chaubey J, Kodan P, Jorwal P, Nischa N, Chandra S, Ramachandran R, Wig N. Mutation in atpE and Rv0678 genes associated with bedaquiline resistance among drug-resistant tuberculosis patients: A pilot study from a high-burden setting in Northern India. Int J Mycobacteriol [serial online] 2020 [[cited 2023 Jan 3];9:212-5. |
Mutated Rv0678 Gene
- Rv0678 gene is a Mycobacterial gene responsible for the expression of the MmpS5 – MmpL5 efflux pumps in the Mycobacterium tuberculosis complex.
- These genes are naturally found in different bacteria and archaea including the Mycobacterium species; however, a mutation in the Rv0678 gene results in overexpression of the efflux pumps like Mycobacterial membrane protein Large (mmpL) and Mycobacterial membrane protein Small (mmpS).
Mechanism of Conferring Resistance of Mutated Rv0678 Gene
- Mutations in the Rv0678 gene result in the overexpression of the mmpL and mmpS type efflux pumps, particularly MmpL5 and MmpS5 are the efflux pump of concern. These efflux pumps provide efflux-associated resistance to Bedaquiline. Overexpression of the MmpL5/MmpS5 efflux pumps is associated with the increase of the MIC value of the Bedaquiline antibiotic by 2- to 16- folds.
Detection Method of Mutated Rv0678 Gene
- There is no unique sequence to read and identify the mutation in the Rv0678 gene. The only available and used method to know about the mutation is to do the complete nucleotide sequencing of the Rv0678 gene from the suspected isolate and map it with the nucleotide sequence of the Rv0678 gene from the reference M. tuberculosis H37Rv genome sequence.
- The primer that can be used to amplify the Rv0678 gene is tabulated below.
| Primers | References |
| F: 5’- AGC CGG AAA CTT CGT ACT CCAC -3’ R: 5’- GCT GGA CAA CAC GGT CAC CT -3’ | Singh BK, Soneja M, Sharma R, Chaubey J, Kodan P, Jorwal P, Nischa N, Chandra S, Ramachandran R, Wig N. Mutation in atpE and Rv0678 genes associated with bedaquiline resistance among drug-resistant tuberculosis patients: A pilot study from a high-burden setting in Northern India. Int J Mycobaceriol [serial online] 2020 [[cited 2023 Jan 3];9:212-5. |
| F: 5’- CTT CGG AAC CAA AGA AAG TG -3’ R: 5’- CCA ACC GAG TCA AAC TCC TG -3’ | Crystal Structure of the Transcriptional Regulator Rv0678 of Mycobacterium tuberculosis. THE JOURNAL OF BIOLOGICAL CHEMISTRY VOL. 289, NO. 23, pp. 16526 –16540, June 6, 2014. DOI:https://doi.org/10.1074/jbc.M113.538959 |
Mutated rpoB Gene
- The rpoB gene is a bacterial gene encoding for the -subunit of bacterial RNA polymerase enzyme. It has been extensively used in the identification and phylogenetic analysis of bacteria. In Mycobacterium tuberculosis also, the rpoB gene encodes for the -subunit of DNA-dependent RNA polymerase. This -subunit is the target site of rifampicin antibiotic i.e. rifampicin binds at the -subunit of RNA polymerase and physically blocks amino-acid elongation step and prevents bacteria from synthesizing the required proteins.
- In about 70 – 90% of rifampicin-resistant M. tuberculosis, mutations are reported in the rpoB gene, mainly in three codons: 531, 526, and 516 codons.
Mechanism of Conferring Resistance of Mutated rpoB Gene
- Mutated rpoB gene encodes for the synthesis of modified -subunit of DNA-dependent RNA polymerase (‘-subunit). Rifampicin can’t bind with this modified ‘-subunit and fails to prevent the protein elongation step in the bacterium ensuring an increase in the MIC value of rifampicin and a higher chance of treatment failure.
Detection Method of Mutated rpoB Gene
- PCR is first used to identify and amplify the rpoB gene from isolates followed by gene sequencing to identify the complete nucleotide sequence. The obtained nucleotide sequence of the rpoB gene is then compared with the reference nucleotide sequence of the rpoB gene of M. tuberculosis H37Rv. The primers that can be used in the process are:
| Primers | References |
| F: 5′- GAG GCG ATC ACA CCG CAG ACGT-3′ R: 5′- GAT GTT GGG CCC CTC AGG GGTT-3′ | (2014). Mutation pattern in rifampicin resistance determining region of rpoB gene in multidrug-resistant Mycobacterium tuberculosis isolates from Pakistan. International Journal of Mycobacteriology, 3(3), 173-177. https://doi.org/10.1016/j.ijmyco.2014.06.004 |
| F: 5′- GTC GCC GCG ATC AAG GA -3′ R: 5′- TGA CCC GCG CGT ACA C -3′ | Gupta, Anamika & Prakash, Pradyot & Singh, Surya & Anupurba, Shampa. (2013). Rapid Genotypic Detection of rpoB and katG Gene Mutations in Mycobacterium tuberculosis Clinical Isolates from Northern India as Determined by MAS-PCR. Journal of clinical laboratory analysis. 27. 31-7. 10.1002/jcla.21558. |
| F: 5′- CGA ATA TCT GGT CCG CTT G -3′ R: 5′- GGT CAG GTA CAC GAT CTC -3′ | Motavaf, B., Keshavarz, N., Ghorbanian, F., Firuzabadi, S., Hosseini, F., & Bostanabad, S. Z. (2021). Detection of genomic mutations in katG and rpoB genes among multidrug-resistant Mycobacterium tuberculosis isolates from Tehran, Iran. New Microbes and New Infections, 41. https://doi.org/10.1016/j.nmni.2021.100879 |
Mutated katG Gene
- katG gene (Rv1908c gene) is a mycobacterial gene that encodes for the synthesis of the catalase-peroxidase enzyme (KatG). KatG is a catalase enzyme that catalyzes the decomposition of hydrogen peroxide into oxygen and water molecules and thus prevents the bacteria from oxidative damage.
- Besides this cellular function, the KatG enzyme is responsible for activating a pro-anti-TB-drug, isoniazid.
- The katG gene encodes for the KatG type catalase enzyme that catalyzed the formation of isonicotinic acyl radical from the isoniazid molecule. Thus formed isonicotinic acyl radical spontaneously combines with the NADH molecule forming an Isonicotinic acyl-NADH complex which combines with InhA, the enoyl-acyl carrier protein reductase enzyme. This binding will prevent the formation of mycolic acid; hence disrupting the bacterial cell wall resulting in cell lysis.
- Mutation in the katG gene has been associated with the majority of isoniazid-resistant Mycobacterium tuberculosis. In about 94% of isoniazid-resistant clinical isolates of mycobacteria, the S315T variant of the KatG catalase-peroxidase enzyme has been observed.
Mechanism of Conferring Resistance of Mutated katG Gene
- The mutated katG gene encodes for the modified type of KatG enzyme, mainly the S315T variant. These modified KatG enzymes can’t catalyze the formation of the Isonicotinic acyl-NADH complex and the prodrug isoniazid remains in its inactive prodrug stage. The isoniazid can’t prevent the formation of mycolic acid and can’t induce cell wall degradation-associated mycobacterial cell lysis.
Detection Method of Mutated katG Gene
- Getting the complete nucleotide sequence of the katG gene and comparing the sequence with the katG gene of M. tuberculosis H37Rv is the ideal method to detect the mutation in the katG gene. Some of the primers that can be used to amplify the katG gene via the PCR method are:
| Primers | References |
| F: 5′- GCG ACG CGT GAT CCG CTC ATA G-3′ R: 3′-TCG GCG GTC ACA CTT T-5′ | Samad, Gusai H.Abdel, Solima M. A. Sabeel, Walaa A. Abuelgassim, Abeer E. Abdelltif, Wisam M. Osman, Mona A. Haroun, Somaya M. Soliman, Sami. A. B. Salam, Hamid. A. Hamdan, and Mohamed A. Hassan. “Molecular Characteristic and Insilico Analysis of KatG Gene in Isoniazid Resistance Mycobacterium Tuberculosis Isolate from Sudan.” American Journal of Microbiological Research 2, no. 6 (2014): 227-233. |
| F: 5′- GCA GAT GGG GCT GAT CTA CG -3′ R: 5′- AAC GGG TCC GGG ATG GTG -3′ | Gupta, Anamika & Prakash, Pradyot & Singh, Surya & Anupurba, Shampa. (2013). Rapid Genotypic Detection of rpoB and katG Gene Mutations in Mycobacterium tuberculosis Clinical Isolates from Northern India as Determined by MAS-PCR. Journal of clinical laboratory analysis. 27. 31-7. 10.1002/jcla.21558. |
| F: 5′- CTC GGC GAT GAG CGT TAC -3′ R: 5′- TCC TTG GCG GTG TAT TGC -3′ | Kardan Yamchi J., Haeili M., Gizaw Feyisa S., Kazemian H., Hashemi Shahraki A., Zahednamazi F. Evaluation of efflux pump gene expression among drug susceptible and drug resistant strains of Mycobacterium tuberculosis from Iran. Inf Genetic Evol. 2015;36:23–26 |
Mutated ethA Gene
- ethA gene is a mycobacterial gene that encodes for the production of the Baeyer Villiger monooxygenase EthA enzyme. This enzyme activates the pro-anti-TB-drug ethionamide into an active radical which then couples with the NADH molecule making it an active toxic complex. Thus activated complex then inhibits the enoyl-acyl carrier protein reductase InhA which ultimately prevents the formation of mycolic acid and induces the disruption of the mycolic acid in the mycobacterial cell wall inducing the cell lysis.
- In the majority of the ethionamide-resistant clinical isolates of Mycobacterium spp., a mutation in the ethA gene, particularly loss-of-function frameshift mutation and nonsense mutation, has been recorded.
- Ethionamide is an important anti-TB drug used widely to treat MDR-TB as a second-line drug. And, the mutation in the ethA gene has rendered this drug ineffective against a significant number of MDR-TB pathogens.
Mechanism of Conferring Resistance of Mutated ethA Gene
- The mutated ethA genes encode for modified EthA enzymes which can’t activate the prodrug ethionamide. Thus unactivated ethionamide can’t disrupt the mycolic acid and the bacterium can survive.
Detection Method of Mutated ethA Gene
- For the detection of mutation in the ethA gene, the ethA gene must be sequenced and compared with the reference nucleotide sequence of the ethA gene of the reference of M. tuberculosis H37Rv. The PCR primers that can be used for the identification and amplification of the ethA gene are:
| Primers | References |
| F: 5′- ATC ATC GTC GTC TGA CTA TGG -3′ R: 5′- ACT ACA ACC CCT GGG ACC -3′ | Moazemi, S., Arjomandzadegan, M., Ahmadi, A., Tayebun, M., & Shojapor, M. (2015). Study of ethA gene sequence in Ethionamide resistant clinical isolates of Mycobacterium tuberculosis. |
Other Genes Responsible for MDR/XDR-TB
| Types of Mutated Genes | Resistant Antibiotics | PCR Primers for Detection | References |
| Mutated rrs Genes | Aminoglycosides like streptomycin, amikacin, kanamycin, capreomycin, viomycin | F: 5’- TTA AAA GCC GGT CTC AGT TC-3’ R: 5’- TAC GCC CCA CCA GTT GGG GC-3’ | Suzuki, Y., Katsukawa, C., Tamaru, A., Abe, C., Makino, M., Mizuguchi, Y., & Taniguchi, H. (1998). Detection of Kanamycin-Resistant Mycobacterium tuberculosis by Identifying Mutations in the 16S rRNA Gene. Journal of Clinical Microbiology, 36(5), 1220-1225. https://doi.org/10.1128/jcm.36.5.1220-1225.1998 |
| Mutated rspL Gene | Aminoglycosides like streptomycin, amikacin, kanamycin, capreomycin, viomycin | F: 5’- GAA TTC GGT AGA TGC CAA CCA TCC -3’ R: 5’- TGA AGC TTG ACC AAC GGA CGC TTG GG-3’ | Katsukawa C, Tamaru A, Miyata Y, Abe C, Makino M, Suzuki Y. Characterization of the rpsL and rrs genes of streptomycin-resistant clinical isolates of Mycobacterium tuberculosis in Japan. J Appl Microbiol. 1997 Nov;83(5):634-40. doi: 10.1046/j.1365-2672.1997.00279.x. PMID: 9418025 |
| Mutated inhA Gene | Isoniazid | F: 5′-ACA TAC CTG CTG CGC AAT -3′ R: 5′-TCA CAT TCG ACG CCA AAC -3′ | Hosny AM, Shady HMA, Essawy AKE (2020) rpoB, katG and inhA Genes: The Mutations Associated with Resistance to Rifampicin and Isoniazid in Egyptian Mycobacterium tuberculosis Clinical Isolates. J Microb Biochem Technol.12:3. doi: 10.35248/1948-5948.20.12.428 |
| Mutated aphC Gene | Isoniazid | — | — |
| Mutated gyrA and gyrB Gene | Fluoroquinolones like moxifloxacin, levofloxacin, ofloxacin | — | — |
| Mutated pncA Gene | Pyrazinamide | F: 5’- AAG GCC GCG ATG ACA CCT CT -3’ R: 5’- GTG TCG TAG AAG CGG CCG AT -3’ | Juréen Pontus et al. “Pyrazinamide Resistance and PncA Gene Mutations in Mycobacterium Tuberculosis.” Antimicrobial Agents and Chemotherapy 52.5 (2008): 1852–1854. Web. |
| Mutated rpoB Gene | Rifampicin | — | — |
| Mutated embB Gene | Ethambutol | — | Lee, S. G., Khadijah Othman, S. N., Ho, Y. M., & Wong, S. Y. (2004). Novel Mutations within the embB Gene in Ethambutol-Susceptible Clinical Isolates of Mycobacterium tuberculosis. Antimicrobial Agents and Chemotherapy, 48(11), 4447-4449. https://doi.org/10.1128/AAC.48.11.4447-4449.2004 |
| Mutated gidB Gene | Kanamycin, amikacin | — | — |
| Mutated tlyA Gene | Capreomycin | — | — |
References
- Goel, D. (2014). Bedaquiline: A novel drug to combat multiple drug-resistant tuberculosis. Journal of Pharmacology & Pharmacotherapeutics, 5(1), 76-78. https://doi.org/10.4103/0976-500X.124435
- Le Ray, L. F., Aubry, A., Sougakoff, W., Revest, M., Robert, J., Bonnet, I., Veziris, N., & Morel, F. (2022). atpE Mutation in Mycobacterium tuberculosis Not Always Predictive of Bedaquiline Treatment Failure. Emerging Infectious Diseases, 28(5), 1062-1064. https://doi.org/10.3201/eid2805.212517
- Ismail, N., Ismail, N. A., Omar, S. V., & Peters, P. H. (2019). In Vitro Study of Stepwise Acquisition of rv0678 and atpE Mutations Conferring Bedaquiline Resistance. Antimicrobial Agents and Chemotherapy, 63(8). https://doi.org/10.1128/AAC.00292-19
- Radomski, N., Roguet, A., Lucas, F.S. et al. atpE gene as a new useful specific molecular target to quantify Mycobacteriumin environmental samples. BMC Microbiol 13, 277 (2013). https://doi.org/10.1186/1471-2180-13-277
- The CRyPTIC Consortium (2022) A data compendium associating the genomes of 12,289 Mycobacterium tuberculosis isolates with quantitative resistance phenotypes to 13 antibiotics. PLoS Biol 20(8): e3001721. https://doi.org/10.1371/journal.pbio.3001721
- Villellas, C., Coeck, N., Meehan, C. J., Lounis, N., Jong, B. D., Rigouts, L., & Andries, K. (2017). Unexpected high prevalence of resistance-associated Rv0678 variants in MDR-TB patients without documented prior use of clofazimine or bedaquiline. Journal of Antimicrobial Chemotherapy, 72(3), 684-690. https://doi.org/10.1093/jac/dkw502
- Clement K. M. Tsui, Flavia Sorrentino, Gagandeep Narula, Alfonso Mendoza-Losana, Ruben Gonzalez del Rio, Esther Pérez Herrán, Abraham Lopez, Adama Bojang, Xingji Zheng, Modesto Jesus Remuiñán-Blanco, Yossef Av-Gay. (2022) Hit Compounds and Associated Targets in Intracellular Mycobacterium tuberculosis. Molecules 27:14, 4446.
- Crystal Structure of the Transcriptional Regulator Rv0678 of Mycobacterium tuberculosis. THE JOURNAL OF BIOLOGICAL CHEMISTRY VOL. 289, NO. 23, pp. 16526 –16540, June 6, 2014.DOI:https://doi.org/10.1074/jbc.M113.538959
- Briffotaux, Julien; Huang, Wei; Wang, Xinwei; Gicquel, Brigitte (2017). MmpS5/MmpL5 as an efflux pump in Mycobacterium species. Tuberculosis, 107(), 13–19. doi:10.1016/j.tube.2017.08.001
- Treatment of Tuberculosis: Guidelines. 4th edition. Geneva: World Health Organization; 2010. A1, Essential first-line antituberculosis drugs. Available from: https://www.ncbi.nlm.nih.gov/books/NBK138747/
- Treatment for TB Disease | TB | CDC
- Gygli, Sebastian M.; Borrell, Sonia; Trauner, Andrej; Gagneux, Sebastien (2017). Antimicrobial resistance in Mycobacterium tuberculosis: mechanistic and evolutionary perspectives. FEMS Microbiology Reviews, (), –. doi:10.1093/femsre/fux011
- Second-Line Drugs for Tuberculosis (brainkart.com)
- Adékambi T, Drancourt M, Raoult D. The rpoB gene as a tool for clinical microbiologists. Trends Microbiol. 2009 Jan;17(1):37-45. doi: 10.1016/j.tim.2008.09.008. Epub 2008 Dec 10. PMID: 19081723.
- Miller, L. P., Crawford, J. T., & Shinnick, T. M. (1994). The rpoB gene of Mycobacterium tuberculosis. Antimicrobial Agents and Chemotherapy, 38(4), 805-811. https://doi.org/10.1128/aac.38.4.805
- (2014). Mutation pattern in rifampicin resistance determining region of rpoB gene in multidrug-resistant Mycobacterium tuberculosis isolates from Pakistan. International Journal of Mycobacteriology, 3(3), 173-177. https://doi.org/10.1016/j.ijmyco.2014.06.004
- Gupta, Anamika & Prakash, Pradyot & Singh, Surya & Anupurba, Shampa. (2013). Rapid Genotypic Detection of rpoB and katG Gene Mutations in Mycobacterium tuberculosis Clinical Isolates from Northern India as Determined by MAS-PCR. Journal of clinical laboratory analysis. 27. 31-7. 10.1002/jcla.21558.
- Makadia, J. S., Jain, A., Patra, S. K., Sherwal, B. L., & Khanna, A. (2012). Emerging Trend of Mutation Profile of rpoB Gene in MDR Tuberculosis, North India. Indian Journal of Clinical Biochemistry, 27(4), 370-374. https://doi.org/10.1007/s12291-012-0228-5
- Rando-Segura, A., Aznar, M., Moreno, M.M. et al. Molecular characterization of rpoB gene mutations in isolates from tuberculosis patients in Cubal, Republic of Angola. BMC Infect Dis 21, 1056 (2021). https://doi.org/10.1186/s12879-021-06763-8
- Isoniazid. (2022, December 26). In Wikipedia. https://en.wikipedia.org/wiki/Isoniazid
- Samad, Gusai H.Abdel, Solima M. A. Sabeel, Walaa A. Abuelgassim, Abeer E. Abdelltif, Wisam M. Osman, Mona A. Haroun, Somaya M. Soliman, Sami. A. B. Salam, Hamid. A. Hamdan, and Mohamed A. Hassan. “Molecular Characteristic and Insilico Analysis of KatG Gene in Isoniazid Resistance Mycobacterium Tuberculosis Isolate from Sudan.” American Journal of Microbiological Research 2, no. 6 (2014): 227-233.
- Narmandakh, E., Tumenbayar, O., Borolzoi, T., Erkhembayar, B., Boldoo, T., Dambaa, N., Burneebaatar, B., Nymadawa, N., Mitarai, S., Jav, S., & Chiang, Y. (2020). Genetic Mutations Associated with Isoniazid Resistance in Mycobacterium tuberculosis in Mongolia. Antimicrobial Agents and Chemotherapy, 64(7). https://doi.org/10.1128/AAC.00537-20
- (2016). Overview on mechanisms of isoniazid action and resistance in Mycobacterium tuberculosis. Infection, Genetics and Evolution, 45, 474-492. https://doi.org/10.1016/j.meegid.2016.09.004
- Ushtanit, A., Kulagina, E., Mikhailova, Y., Makarova, M., Safonova, S., & Zimenkov, D. (2022). Molecular Determinants of Ethionamide Resistance in Clinical Isolates of Mycobacterium tuberculosis. Antibiotics, 11(2). https://doi.org/10.3390/antibiotics11020133
- Pillay, S., Steingart, K. R., Davies, G. R., Chaplin, M., Vos, M. D., Schumacher, S. G., Warren, R., & Theron, G. (2022). Xpert MTB/XDR for detection of pulmonary tuberculosis and resistance to isoniazid, fluoroquinolones, ethionamide, and amikacin. The Cochrane Database of Systematic Reviews, 2022(5). https://doi.org/10.1002/14651858.CD014841.pub2
- Katsukawa C, Tamaru A, Miyata Y, Abe C, Makino M, Suzuki Y. Characterization of the rpsL and rrs genes of streptomycin-resistant clinical isolates of Mycobacterium tuberculosis in Japan. J Appl Microbiol. 1997 Nov;83(5):634-40. doi: 10.1046/j.1365-2672.1997.00279.x. PMID: 9418025.
- Suzuki, Y., Katsukawa, C., Tamaru, A., Abe, C., Makino, M., Mizuguchi, Y., & Taniguchi, H. (1998). Detection of Kanamycin-Resistant Mycobacterium tuberculosis by Identifying Mutations in the 16S rRNA Gene. Journal of Clinical Microbiology, 36(5), 1220-1225. https://doi.org/10.1128/jcm.36.5.1220-1225.1998
- Maus, C. E., Plikaytis, B. B., & Shinnick, T. M. (2005). Molecular Analysis of Cross-Resistance to Capreomycin, Kanamycin, Amikacin, and Viomycin in Mycobacterium tuberculosis. Antimicrobial Agents and Chemotherapy, 49(8), 3192-3197. https://doi.org/10.1128/AAC.49.8.3192-3197.2005
- Jain, A. (2016). Novel mutations conferring resistance to kanamycin in Mycobacterium tuberculosis clinical isolates from Northern India. Tuberculosis, 96, 96-101. https://doi.org/10.1016/j.tube.2015.10.012
- Juréen Pontus et al. “Pyrazinamide Resistance and PncA Gene Mutations in Mycobacterium Tuberculosis.” Antimicrobial Agents and Chemotherapy 52.5 (2008): 1852–1854. Web.
- Somoskovi, A., Dormandy, J., Parsons, L. M., Kaswa, M., Goh, K. S., Rastogi, N., & Salfinger, M. (2007). Sequencing of the pncA Gene in Members of the Mycobacterium tuberculosis Complex Has Important Diagnostic Applications: Identification of a Species-Specific pncA Mutation in “Mycobacterium canettii” and the Reliable and Rapid Predictor of Pyrazinamide Resistance. Journal of Clinical Microbiology, 45(2), 595-599. https://doi.org/10.1128/JCM.01454-06
