Enterobacteriaceae is a family of Gram-negative rod-shaped Gammaproteobacteria in the order Enterobacterales in the phylum Pseudomonadota. These bacteria are commensals of the intestine of animals, including humans; however, some are pathogenic to humans and even cause severe infections.
They are held accountable for several infectious diseases like urinary tract infections (UTIs), respiratory tract infections (RTIs), blood-stream infections (BSIs), gastrointestinal infections, wounds, and soft tissue infections. For the treatment of such Enterobacterales-associated infections, β-lactam antibiotics are the most preferred antibiotics. Besides β-lactams, tetracyclines, colistin, and aminoglycosides are also widely used in case β-lactams have lower sensitivity.
However, the emergence of antibiotic resistance has made most of the available and preferred treatments useless against Enterobacterales. Antibiotic resistantance genes such as Beta-lactamase genes (bla genes), colistin-resistant genes, tetracycline-resistant genes, and aminoglycoside-resistant genes are the most important antibiotic-resistant genes in Enterobacterales.
Some of the most important members of these antibiotic-resistant gene families are briefly described in this article.
Interesting Science Videos
Beta-lactamase (bla) Genes
- Beta-lactamase genes (bla genes) are the largest group of antibiotic-resistant genes found in Enterobacteriaceae and other bacteria that confer resistance against the β-lactam antibiotics. These genes encode for β-lactamase enzymes that hydrolyze the β-lactam ring of β-lactam antibiotics such as penicillins, cephalosporins, carbapenems, aztreonam, etc.
- Mechanism of Conferring Resistance: bla genes encode for the synthesis of β-lactamase enzymes. These enzymes are capable of hydrolyzing β-lactam ring of β-lactam antibiotics. Hydrolysis of the β-lactam ring disrupts their molecular structure and the antibiotics can’t interrupt the process of crosslinking during bacterial cell wall synthesis.
- Different types of bla genes code for different variants of β-lactamase enzymes, and each of them may have different activity toward different members of β-lactam antibiotic class. Some can hydrolyze β-lactam ring of penicillins only, while some can hydrolyze the β-lactam ring of penicillins, cephalosporins, monobactams, carbapenems, and even β-lactamase inhibitors.
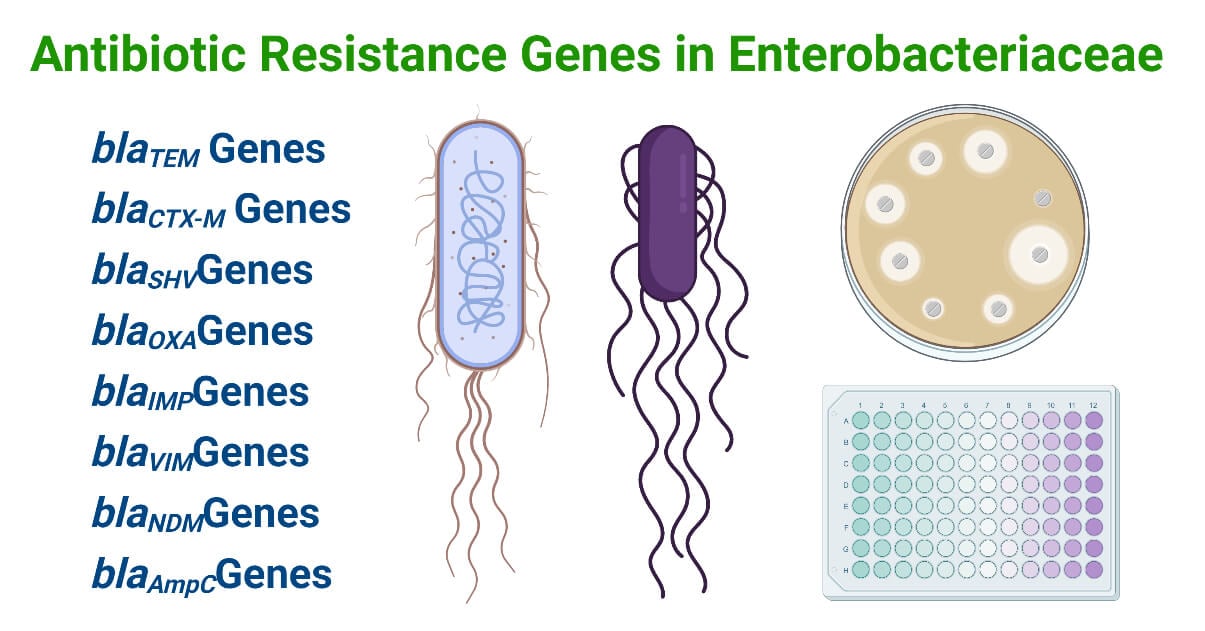
Some of the most important bla genes found in clinical isolates of Enterobacteriaceae are listed below.
1. blaTEM Genes
- blaTEM genes are antibiotic-resistant genes in the bla gene class which confer resistance against β-lactam antibiotics, mostly ampicillin and penicillins, to the bacteria containing the genes. blaTEM gene family contains the most prevalent bla genes in Enterobacteriaceae.
- TEM is the abbreviated form of Temoniera, an Athenian patient from which this gene and its gene product were isolated. TEM-1 enzyme encoded by the blaTEM-1 gene was the first plasmid-mediated β-lactamase enzyme identified in 1963.
- Currently, there are 170 types of TEM β-lactamases each encoded by a variant of the blaTEM gene. The blaTEM-1 gene is the most commonly isolated variant in Enterobacteriaceae. blaTEM-1 gene variants are referred to as Extended Spectrum Beta-Lactamases and show hydrolyzing activity against a wide range of β-lactam antibiotics like penicillins and cephalosporins. They are mainly reported in ESBL-producing E. coli and K. pneumoniae strains. Other variants of blaTEM genes are also reported to encode enzymes that can hydrolyze aztreonam, monobactam, the 3rd and 4th generation cephalosporins, and some β-lactamase inhibitors.
Mechanism of Conferring Resistance of blaTEM Genes
- blaTEM genes are β-lactamase enzyme encoding genes. They encode for TEM- β-lactamase enzymes, Class-A β-lactamases. These enzymes are capable of hydrolyzing β-lactam ring of aminopenicillins (like amoxicillin and ampicillin) and early cephalosporins (mostly the first and second-generation cephalosporins).
Detection Method of blaTEM Genes
- The presence of bla genes can be phenotypically presumed by performing antimicrobial sensitivity testing using different groups of beta-lactam antibiotics, but, for the identification of actual genes involved in the process, molecular detection methods are very effective. PCR, DNA probe method, DNA microarray, etc. can be used. Polymerase chain reaction (PCR) remains superior over all available molecular detection methods and is widely used in clinical and research laboratories.
- Primers that are used in some research to identify blaTEM genes are:
| Primers | References |
| F: 5′-GAGACAATAACCCTGGTAAAT-3′ R: 5′-AGAAGTAAGTTGGCAGCAGTG-3′ | Prasad Sah, R. S., Dhungel, B., Yadav, B. K., Adhikari, N., Shrestha, U. T., Lekhak, B., Banjara, M. R., Adhikari, B., Ghimire, P., & Rijal, K. R. (2021). Detection of TEM and CTX-M Genes in Escherichia coli Isolated from Clinical Specimens at Tertiary Care Heart Hospital, Kathmandu, Nepal. Diseases, 9(1). https://doi.org/10.3390/diseases9010015 |
| F: 5′-TATGTGGTGCGGTATTATCC-3′ R: 5′-AGTTAATAGTTTGCGCAACG-3′ | Saif Jabbar ALzubaidi, and Marwa Hameed Alkhafaji. Molecular Detection of bla TEM and bla CTX-M Genes in Clinical and Food-Borne Klebsiella pneumoniae Isolates. J. Med. Chem. Sci. 2023, 6(7) 1706-1713. Manuscript ID: JMCS-2211-1869. DOI:10.26655/JMCHEMSCI.2023.7.20 |
Nucleic acid sequencing of the isolated TEM gene must be done in order to classify the gene up to the level of its gene variants.
2. blaCTX-M Genes
- blaCTX-M gene is another family of bla genes that encode for CTX-M type β-lactamase synthesis. blaCTX-M genes are identified predominantly in ESBL strains of E. coli and Klebsiella pneumoniae globally. These are found in the plasmid of Salmonella enterica serovar Typhimurium, E. coli, Klebsiella spp., and Proteus spp. These genes are usually found in the larger plasmid, IncFII plasmids, containing other antibiotic-resistance genes. These genes are capable of horizontal gene transfer and hence the blaCTX-M genes can be easily disseminated in other Enterobacterales.
- CTX-M is an abbreviated form of cefotaximase and Munich (CTX for cefotaximase and M for Munich) as CTX-M type β-lactamases are capable of hydrolyzing cefotaxime and first identified in E. coli isolated from ear discharge of a 4-month child in 1989 in Munich, Germany. This enzyme was called CTX-M-1, and the gene encoding the enzyme is blaCTX-M-1.
- Currently, 172 CTX-M types enzymes are identified suggesting that there are more than 172 variants of blaCTX-M genes. blaCTX-M-1 and blaCTX-M-15 genes are the most predominant types of the blaCTX-M gene family.
Mechanism of Conferring Resistance of blaCTX-M Genes
- blaCTX-M genes encode for the synthesis of CTX-M (cefotaximase ) beta-lactamase enzymes. These enzymes hydrolyze the β-lactam ring of oxyimino-thiazolyl cephalosporins (like the 3rd and the 4th generation cephalosporins such as cefotaxime, ceftazidime, ceftriaxone, etc.). Most of them have greater activity against Cefotaxime, while some have higher activity against ceftazidime.
Detection Method of blaCTX-M Genes
- PCR remains the superior method for the detection of blaCTX-M genes. Some primers that can be used for their detection are:
| Primers | References |
| F: 5′-TTTGCGATGTGCAGTACCAGTAA-3′ R: 5′-CGATATCGTTGGTGGTGCCATA-3′ | Prasad Sah, R. S., Dhungel, B., Yadav, B. K., Adhikari, N., Shrestha, U. T., Lekhak, B., Banjara, M. R., Adhikari, B., Ghimire, P., & Rijal, K. R. (2021). Detection of TEM and CTX-M Genes in Escherichia coli Isolated from Clinical Specimens at Tertiary Care Heart Hospital, Kathmandu, Nepal. Diseases, 9(1). https://doi.org/10.3390/diseases9010015 |
| F: 5′-GCTTTCTGCCTTAGGTTGA-3′ R: 5′-AATCAGCGAGTTGAGATCAA-3′ | Saif Jabbar ALzubaidi, and Marwa Hameed Alkhafaji. Molecular Detection of bla TEM and bla CTX-M Genes in Clinical and Food-Borne Klebsiella pneumoniae Isolates. J. Med. Chem. Sci. 2023, 6(7) 1706-1713. Manuscript ID: JMCS-2211-1869. DOI:10.26655/JMCHEMSCI.2023.7.20 |
CTX-M consensus primers can be used to differentiate the identified blaCTX-M genes into several variants. However, PCR alone can’t be enough to promptly differentiate the blaCTX-M genes, hence, nucleic acid sequencing of the amplicons must be done for complete identification of the gene variants.
3. blaSHV Genes
- blaSHV gene family is another group of bla genes that encodes for the synthesis of SHV-type β-lactamases that can hydrolyze cephalosporins and other β-lactam antibiotics. These genes were originally found in chromosomal DNA; however, they are now widely reported to be found in the plasmid DNA of several clinically isolated Enterobacterales. These genes are mainly found in Klebsiella pneumoniae, E. coli, Shigella spp., and Enterobacter cloacae.
- SHV is the abbreviated form of the ‘Sulfhydryl variant’.
- The first blaSHV gene was identified in the early 1970s in E. coli and was called the blaSHV -1 gene. Since then, more than 215 blaSHV gene variants are identified. These variants encode several SHV-type beta-lactamase enzymes. Some of them have activity against a wide variety of cephalosporins (including the oxyimino cephalosporins), penicillins, and monobactam; hence are called ESBL SHV variants. Whereas, others are active against penicillins, ampicillin, and earlier cephalosporins. These are called non-ESBL SHV variants.
- blaSHV-1, blaSHV-11, and blaSHV-2 are the most predominantly reported variants of the blaSHV genes.
Mechanism of Conferring Resistance of blaSHV Genes
- blaSHV genes encode for SHV-type beta-lactamase enzymes that hydrolyze the beta-lactam ring of several susceptible beta-lactam antibiotics. They are mainly responsible for ampicillin and amoxicillin resistance in Klebsiella and E. coli. But, they can even hydrolyze the beta-lactam ring of the extended cephalosporins, aztreonam, monobactam, and even carbapenems.
Detection Method of blaSHV Genes
- PCR is the most helpful tool to isolate, amplify and identify the blaSHV genes. Nucleic acid sequencing of the isolated blaSHV gene is done to know which variant it is. The primers that can be used to amplify the blaSHV genes are:
| Primer | References |
| F: 5′-CAGCAGGATCTGGTGGACTACT-3′ R: 5′-GTCAAGGCGGGTGACGTT-3′ | Perovic, Olga & Singh-Moodley, Ashika & Duse, Adriano & Bamford, Colleen & Elliott, G & Swe Swe, Khine & Kularatne, Ranmini & Lowman, Warren & Whitelaw, Andrew & Nana, Trusha & Wadula, Jeannette & Lekalakala, Molebogeng & Saif, Adrienne & De-Smit, Melony & Marais, Else. (2014). National sentinel site surveillance for antimicrobial resistance in Klebsiella pneumoniae isolates in South Africa, 2010 – 2012. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 104. 10.7196/samj.7617. |
| F: 5′-GTGGACTACTCGCCGGTCA-3′ R: 5′-GGCGTATCCCGCAGATAAATCACCA-3′ | Dong, Yuanyuan; Sheng, Haihui; Zeng, Xainting; Yan, Jufen; Li, Haiyan; Xiao, Huasheng; Li, Xiaokun; Yang, Shulin (2012). Investigation of Genetic Diversity of the <i>bla</i> <sub/>SHV</sub> Gene and Development of an Oligonucleotide Microarray to Detect Mutations in the <i>bla</i> <sub/>SHV</sub> Gene. Microbial Drug Resistance, 18(6), 539–545. doi:10.1089/mdr.2012.0057 |
4. blaOXA Genes
- blaOXA genes (Oxacillinase genes) are another type of bla genes that encode for the production of Oxacillinase enzymes. These genes have been reported in E. coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Acinetobacter baumannii, etc.
- Most of the blaOXA genes are plasmid-encoded while some are also found in chromosomes and transposons of several Gram-negative bacteria.
- Some blaOXA genes encode for ESBLs and carbapenemases, while some are responsible for non-ESBL Oxacillinases. Currently, more than 127 variants of OXA enzymes, each with several sub-variants, are discovered globally. Accordingly, more than 127 blaOXA variants, each with multiple sub-variants are estimated to exist.
- These genes encode for OXA-type enzymes that can primarily hydrolyze isoxazolylpenicillines like oxacillin, cloxacillin, dicloxacillin, etc., and other similar penicillins. Some variants can also hydrolyze cephalosporins, aztreonam, carbapenems, etc.
- blaOXA-1 types are most common in Enterobacterales and blaOXA-48 gene variants are the most important variants as they are ESBL type and can even hydrolyze carbapenems.
Mechanism of Conferring Resistance of blaOXA Genes
- blaOXA genes encode for class-D beta-lactamases called the Oxacillinases enzymes. These enzymes hydrolyze the beta-lactam ring of oxacillin (isoxazolylpenicillines) and other susceptible beta-lactam antibiotics.
Detection Method of blaOXA Genes
- PCR and gene sequencing methods are the primary methods for the detection and identification of the blaOXA genes. The primers that can be used during the process are:
| blaOXA gene types | Primers | References |
| blaOXA-48 | F: 5′-GTAGCAAAGGAATGGCAA-3′ R: 5′-CCTTGCTGCTTATTGTCA-3′ | Thierry Naas, Garance Cotellon, Ayla Ergani, Patrice Nordmann, Real-time PCR for detection of blaOXA-48 genes from stools, Journal of Antimicrobial Chemotherapy, Volume 68, Issue 1, January 2013, Pages 101–104, https://doi.org/10.1093/jac/dks340 |
| blaOXA-48 | F: 5ʹ-GCTTGATCGCCCTCGATT-3ʹ R: 5ʹ-GATTTGCTCCGTGGCCGAAA-3ʹ | Gurung, S., Kafle, S., Dhungel, B., Adhikari, N., Shrestha, U. T., Adhikari, B., Banjara, M. R., Rijal, K. R., & Ghimire, P. (2020). Detection of OXA-48 Gene in Carbapenem-Resistant Escherichia coli and Klebsiella pneumoniae from Urine Samples. Infection and Drug Resistance, 13, 2311-2321. https://doi.org/10.2147/IDR.S259967 |
| blaOXA-1 | F: 5ʹ-TTTTCTGTTGTTTGGGTTTT-3ʹ R: 5ʹ-TTTCTTGGCTTTTATGCTTG-3ʹ | Sugumar, M., Kumar, K. M., Manoharan, A., Anbarasu, A., & Ramaiah, S. (2014). Detection of OXA-1 β-Lactamase Gene of Klebsiella pneumoniae from Blood Stream Infections (BSI) by Conventional PCR and In-Silico Analysis to Understand the Mechanism of OXA Mediated Resistance. PLOS ONE, 9(3), e91800. https://doi.org/10.1371/journal.pone.0091800 |
| blaOXA-1 | F: 5ʹ-ACACAATACATATCAACTTCGC-3ʹ R: 5ʹ-AGTGTGTTTAGAATGGTGATC-3ʹ | Tabbouche, Sana & Rami, Khudary & Beyrouthy, Racha & Dabboussi, Fouad & Marcel, Achkar & Hassan, Mallat & Hlais, Sani & Monzer, Hilana. (2011). Detection of genes TEM, OXA, SHV and CTX-M in 73 clinical isolates of Escherichia coli producers of extended spectrum Beta-lactamases and determination of their susceptibility to antibiotics. International Arabic Journal of Antimicrobial Agents. 1. |
| blaOXA-2 | F: 5ʹ-AAGAAACGCTACTCGCCTGC-3ʹ R: 5ʹ-CCACTCAACCCATCCTACCC-3ʹ | Bhattacharjee, Amitabha & Sen, Malay & Anupurba, Shampa & Prakash, Pradyot & Nath, Gopal. (2007). Detection of OXA-2 group extended-spectrum-β-lactamase-producing clinical isolates of Escherichia coli from India. The Journal of antimicrobial chemotherapy. 60. 703-4. 10.1093/jac/dkm267. |
5. blaIMP Genes
- blaIMP (Imipenemase) genes are another group of bla genes that code for the synthesis of Imipenemases enzymes in bacteria. These genes are found in a wide variety of carbapenem-resistant species of Gram-negative bacteria including a variety of Enterobacterales (mainly, several strains of E.coli, Klebsiella pneumoniae, and Serratia marcescens).
- Most of these genes are found in the integron of plasmid or chromosomal DNA and hence can be transferable with related bacteria.
- 19 different types of Imipenemase enzymes are clearly known to date suggesting about at least 19 different variants of the blaIMP genes.
Mechanism of Conferring Resistance of blaIMP Genes
- blaIMP genes encode for Imipenemase enzymes, Metallo-beta-lactamase enzymes capable of hydrolyzing broad-spectrum beta-lactam antibiotics like broad-spectrum penicillins and cephalosporins, monobactam, and carbapenems. Enzymes coded by the blaIMP genes can hydrolyze the beta-lactam ring of carbapenems making them clinically very important bla genes.
Detection Method of blaIMP Genes
- PCR method is used to detect the presence of the blaIMP genes in suspected bacteria. Some of the PCR primers used in the process are:
| Primers | References |
| F: 5ʹ-CTACCGCAGCAGAGTCTTTG-3ʹ R: 5ʹ-AACCAGTTTTGCCTTACCAT-3ʹ | Senda, K., Arakawa, Y., Ichiyama, S., Nakashima, K., Ito, H., Ohsuka, S., Shimokata, K., Kato, N., & Ohta, M. (1996). PCR detection of metallo-beta-lactamase gene (blaIMP) in gram-negative rods resistant to broad-spectrum beta-lactams. Journal of Clinical Microbiology, 34(12), 2909-2913. https://doi.org/10.1128/jcm.34.12.2909-2913.1996 |
| F: 5ʹ-GAAGGCGTTTATGTTCATAC-3ʹ R: 5ʹ-CTTCACTGTGACTTGGAAC-3ʹ | Saad, Alyaa & Abdulhussein, Taif. (2019). MOLECULAR GENOTYPING SURVEY FOR BLAIMP VIRULENCE GENE OF ACINETOBACTER BAUMANNII ISOLATES, IRAQ. Plant Archives. 19. 3862-3864. |
| F: 5ʹ-GGAATAGAGTGGCTTAAYTCTC-3ʹ R: 5ʹ-CCAAACYACTASGTTATCT-3ʹ | Poirel L, Walsh TR, Cuvillier V, Nordmann P. Multiplex polymerase chain reaction for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis 2011;70:119–23. doi: 10.1016/j.diagmicrobio.2010.12.002 |
6. blaVIM Genes
- blaVIM genes are a group of bla genes that encodes for the production of VIM (Verona integron encoded Metallo-beta-lactamase) type beta-lactamase enzymes. These genes are plasmid-encoded genes reported in several members of Enterobacteriaceae, primarily Klebsiella pneumoniae, E. coli, Serratia marcescens, Citrobacter spp., etc. Besides, they are very important in carbapenem-resistant strains of Acinetobacter baumannii and Pseudomonas aeruginosa.
- More than 40 types of VIM enzymes are described indicating the presence of more than 40 variants (46 reported variants) of the blaVIM genes. The blaVIM-2 and blaVIM-1 type genes are the two most commonly reported variants of the blaVIM genes.
Mechanism of Conferring Resistance of blaVIM Genes
- blaVIM genes encode for Verona integron-encoded Metallo-beta-lactamase enzymes. These enzymes can hydrolyze the beta-lactam ring of penicillins, extended-spectrum cephalosporins, carbapenems, and other beta-lactam antibiotics.
Detection Method of blaVIM Genes
- PCR is the widely used tool for the detection of the blaVIM genes. The followings are some of the primers that can be used during PCR of blaVIM genes.
| Primers | References |
| F: 5ʹ-GATGGTGTTTGGTCGCATA-3ʹ R: 5ʹ-CGAATGCGCAGCACCAG-3ʹ | Poirel L, Walsh TR, Cuvillier V, Nordmann P. Multiplex polymerase chain reaction for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis 2011;70:119–23. doi: 10.1016/j.diagmicrobio.2010.12.002 |
| F: 5ʹ-AGTGGTGAGTATCCGACA-3ʹ R: 5ʹ-ATGAAAGTGCGTGGAGAC-3ʹ | Ghazaei C. Molecular Detection of Metallo-β-lactamase Genes blaIMP, blaVIM, and blaSPM-1 in Bacillus cereus Strains Isolated from Infant Milk Powder Samples. Int J Infect.6(3):e95266. Doi:10.5812/iji.95266 |
7. blaNDM Genes
- blaNDM genes are novel types of bla genes that are responsible for the production of NDM (New Delhi Metallo-beta-lactamase) type beta-lactamase enzymes. These genes are plasmid-encoded genes found in the transposon region of several large plasmids making them readily disseminated in a wide range of bacteria. They are reported in 20 different types of plasmid, extensively in IncFIB, IncA/C, IncFII, IncX3, IncL/M, and IncH type plasmids, and also in bacterial chromosomes.
- The first blaNDM gene detected was the blaNDM-1 gene found in E. coli and Klebsiella pneumoniae of a Swedish patient in 2008. Since then this gene is globally reported in several Enterobacterales, Pseudomonas aeruginosa, and Acinetobacter baumannii.
- 29 different variants of the blaNDM genes are known, but the blaNDM-1 type gene is most commonly reported. These genes are most prevalent in East Asia, South East Asia, and South Asia, but are also frequently reported in Europe and the USA.
Mechanism of Conferring Resistance of blaNDM Genes
- The blaNDM genes encode for New Delhi Metallo-beta-lactamase enzymes capable of hydrolyzing beta-lactam ring of penicillins, extended-spectrum cephalosporins, aztreonam, carbapenems, and other beta-lactams. These enzymes are Metallo-beta-lactamases having two zinc ions on the active site that helps in hydrolytically cleaving the beta-lactam rings of carbapenems.
Detection Method of blaNDM Genes
- The molecular detection method using the PCR technique is the most widely used gene detection method used to identify and amplify the blaNDM genes. The primers that can be used during the process are tabulated below.
| blaNDM genes | Primers | References |
| blaNDM-1 | F: 5ʹ-ATGGAATTGCCCAATATTATGC-3ʹ R: 5ʹ-CGAAAGTCAGGCTGTGTTG-3ʹ | AL-Harmoosh, Raad & Jarallah, Eman. (2015). FIRST DETECTION OF THE blaNDM-1 and blaNDM-2 GENES IN A CLINICAL ISOLATES OF Acinetobacter baumannii IN HILLAH HOSPITALS-IRAQ. International Journal of Advanced Research. 3. 1407-1416. |
| blaNDM-2 | F: 5ʹ-CACCTCATGTTTGAATTCGCC-3ʹ R: 5ʹ-CTCTGTCACATCGAAATCGC-3ʹ | AL-Harmoosh, Raad & Jarallah, Eman. (2015). FIRST DETECTION OF THE blaNDM-1 and blaNDM-2 GENES IN A CLINICAL ISOLATES OF Acinetobacter baumannii IN HILLAH HOSPITALS-IRAQ. International Journal of Advanced Research. 3. 1407-1416. |
| blaNDM-1 | F: 5ʹ-GGGCAGTCGCTTCCAACGGT-3ʹ R: 5ʹ-GTAGTGCTCAGTGTCGGCAT-3ʹ | Naeem, Sohni & Bilal, Hazrat & Muhammad, Hafsah & Khan, Muhammad Asif & Hameed, Fareeha & Bahadur, Sher & Rehman, Tayyab. (2021). Detection of blaNDM-1 gene in ESBL producing Escherichia coli and Klebsiella pneumoniae isolated from urine samples, 2020.. The Journal of Infection in Developing Countries. 15. 10.3855/jidc.12850. |
8. blaAmpC Genes
- blaAmpC genes are a group of antibiotic-resistant (bla) genes that encode for AmpC-beta-lactamase enzymes. These genes were originally considered to be chromosomal genes; however, diverse types of plasmid-mediated blaAmpC genes (pMAmpC genes) are discovered since the first detection of pMAMPC in 1989.
- These genes are among less studied bla genes but have very great importance in conferring resistance against -methoxy-β-lactam antibiotics, extended-spectrum cephalosporins, and monobactam. Additionally, the AmpC-type beta-lactamases encoded by the blaAmpC genes are poorly inhibited by several beta-lactamase inhibitors, so they are very potent Cephalosporinases.
- These genes are extensively reported in Enterobacterales, Pseudomonas, and Acinetobacter species. Among the Enterobacterales, E. coli, Klebsiella spp. (mainly K. pneumoniae and K. oxytoca), Citrobacter spp., Enterobacter spp., Proteus spp., and Serratia spp. are mostly found to have the blaAmpC genes.
Mechanism of Conferring Resistance of blaAmpC Genes
- These genes encode for AmpC-type beta-lactamase enzymes, a class of Cephalosporinases, which hydrolyze the beta-lactam ring of earlier as well as extended-spectrum cephalosporins. These enzymes hydrolyze the beta-lactam ring of most of the cephalosporins; hence making them ineffective against the bacteria containing the blaAmpC genes.
Detection Method of blaAmpC Genes
- The PCR is the superior tool used in the detection of the blaAmpC genes. Some of the primers used during the PCR amplification processes are:
| Primers | References |
| F: 5´- CTCGACCTCGCGACCTATAC-3´ R: 5´- CTGCCACTGGCGGTAGTAGT-3´ | Detection of ESBL and MBL Antibiotic Resistance Genes in 100 Clinical Isolates of Escherichia Coli by Multiplex PCR. bahman Ghadami Petroudi,R ahman Shokri, Davoud Esmaeili. Research Square. Doi: https://doi.org/10.21203/rs.3.rs-679205/v2 |
| F: 5´- ACTTACTTCAACTCGCGACG -3´ R: 5´- TAAACACCACATATGTTCCG-3´ | Abbas-Al-Khafaji ZK, Aubais-aljelehawy Qh (2021) Evaluation of antibiotic resistance and prevalence of multi-antibiotic resistant genes among Acinetobacter baumannii strains isolated from patients admitted to al-yarmouk hospital. Cellular, Molecular and Biomedical Reports 1(2):60-68. doi:10.55705/cmbr.2021.142761.1015 |
| F: 5´- CTTCCACACTGCTGTTCGCCTTGGCC-3´ R: 5´- AGGATCACCAGTCC-3´ | Kohan, Shirin & Asadpour, Leila & Houshmand, Elham. (2020). The Study of Frequency of SIM and AmpC Genes in Clinical Isolates of Pseudomonas aeruginosa in Gilan, Iran. Infection Epidemiology and Microbiology. 6. 117-125. 10.29252/iem.6.2.117. |
Other bla Genes
Besides the 8 most common and clinically very important bla genes described above, there are several types of the bla genes responsible for beta-lactam resistance in several species of the Enterobacteriaceae family. Some of them are:
| blaSEM blaKPC blaGES blaOXM blaSFO | blaVEB blaCMY blaSEM blaPER blaCIT | blaADC blaLEN blaSFC blaSEM blaACC | blaBEL blaSIP blaTLA blaBIC blaEBC |
aac(6′)-Ib Genes
- The Aminoglycoside 6′-N-Acyltransferase type Ib genes (aac(6′)-Ib genes) are the antibiotic-resistant genes that confer resistance against aminoglycoside antibiotics. Its variant the aac(6′)-Ib-cr gene also confers resistance to fluoroquinolones to some extent. Most of the aac(6′)-Ib genes isolated from pathogens are reported in the plasmid in the transposons; however, these genes are also present as chromosomal genes in a few bacteria.
- Among the aminoglycoside acetyltransferase (aac) genes that enzymatically modify the aminoglycosides, the aac(6′)-Ib genes are the most prevalent and clinically important acc genes. Over 50 variants of the aminoglycoside 6′-N-acyltransferase type Ib enzymes are known indicating the presence of more than 50 variants of the aac(6′)-Ib genes.
- The aac(6′)-Ib genes are the major genes in Enterobacterales like E. coli, Serratia marcescens, Proteus mirabilis, and Enterobacter spp. and in Pseudomonas aeruginosa. In such bacteria, the aac(6′)-Ib genes are mainly provide higher resistance against amikacin, kanamycin, tobramycin, etc., and comparatively lower resistance against gentamycin and streptomycin.
Mechanism of Conferring Resistance of aac(6′)-Ib Genes
- The aac(6′)-Ib genes encode for the aminoglycoside 6′-N-acyltransferase type Ib enzyme that causes acylation of the aminoglycoside antibiotics. These genes are capable of acetylation at the multiple sites of aminoglycosides using the acetyl CoA as a substrate donor. These acetylated aminoglycosides are inactivated and can’t disturb the protein synthesis (amino-acid elongation step) process in bacteria.
Detection Method of aac(6′)-Ib Genes
- As in the detection of other antibiotic-resistant genes, the PCR remains the most important tool to detect the aac(6′)-Ib genes. Some of the primers used for the amplification of the aac(6′)-Ib genes are tabulated below.
| Primers | References |
| F: 5′-ATGACTGAGCATGACCTTG-3′ R: 5′-AACCATGTACACGGCTGG-3′ | Frasson, I., Cavallaro, A., Bergo, C. et al. Prevalence of aac(6′)-Ib-cr plasmid-mediated and chromosome-encoded fluoroquinolone resistance in Enterobacteriaceae in Italy. Gut Pathog 3, 12 (2011). https://doi.org/10.1186/1757-4749-3-12 |
| F: 5`-TATGAGTGGCTAAATCGAT-3` R: 5`-CCCGCTTTCTCGTAGCA-3` | The aac(6`)Ib gene in Proteus mirabilis strains resistant to aminoglycosides. Folia Histochem Cytobiol. 2008:46(4): 531 (531-533) doi: 10.2478/v10042-008-0068-6 |
aph(3’) Genes
- Aminoglycoside phosphotransferase type 3 genes (the aph(3’) genes) are antibiotic-resistant genes that phosphorylate the aminoglycosides and confer resistance against such antibiotics to the bacteria-harboring such genes. These genes are primarily plasmid-encoded genes; however, some variants of the aph(3’) genes are also reported in a few bacteria.
- The aph(3’)-Ib type genes are found in Enterobacterales like E. coli, Klebsiella pneumoniae, K. quasipneumoniae, and Serratia marcescens. This gene encodes for aminoglycoside phosphotransferase type Ib enzyme in these bacteria making them resistant to aminoglycoside antibiotics like gentamicin, kanamycin, and tobramycin.
Mechanism of Conferring Resistance of aph(3’) Genes
- The aph(3’) genes code for the production of aminoglycoside 3-phosphotransferase (APH(3’)) enzymes that phosphorylate aminoglycosides making them unable to affect the bacterial protein synthesis process.
- The APH(3’) enzyme, also called the aminoglycoside kinase, catalyzes the transfer of phosphate from an ATP molecule to the 3’ hydroxyl group of aminoglycosides like Kanamycin through a dissociative mechanism. Thus phosphorylated aminoglycosides lose their ability to disturb the peptide elongation process.
Detection Method of aph(3’) Genes
- The molecular detection method using a PCR is the most important tool in identifying the aph(3’)-Ib type genes. Primers that can be used in the process are:
| aph(3’) genes types | Primers | References |
| aph(3’)-Ib gene | F: 5ʹ-CCTTGGTGATAACGGCAATTC -3′ R: 5ʹ-CCAATCGCAGATAGAAGGC-3′ | Ojdana, Dominika; Sieńko, Anna; Sacha, Paweł; Majewski, Piotr; Wieczorek, Piotr; Wieczorek, Anna; Tryniszewska, Elżbieta (2018). Genetic basis of enzymatic resistance of E. coli to aminoglycosides. Advances in Medical Sciences, 63(1), 9–13. doi:10.1016/j.advms.2017.05.004 |
Mobilized Colistin Resistance (mcr) Genes
- Mobilized colistin resistance genes (mcr genes) are a class of antibiotic-resistant genes that confer resistance to the bacteria against polymixin E (colistin) antibiotic. These are plasmid-encoded antibiotic-resistance genes (except the mcr-6 genes that are reported in bacterial chromosomes) and can be easily transferred to other bacteria of clinical concern. So far, these genes are most commonly reported in E. coli and Klebsiella pneumoniae, but considering the ability of the mcr genes to rapidly transfer from one bacterium to another, it is very likely that several other pathogenic bacteria also harbor these genes.
- To date, 10 different mcr gene types (mcr-1 to mcr-10), each with multiple variants, have been known. Among these mcr gene types, the mcr-1 type genes are the most predominant. The mcr-1 gene was first identified in November 2015 in China in E. coli and K. pneumoniae. A total of 27 different variants of the mcr-1 gene have been recorded so far in a dozen of pathogenic bacterial strains.
- The mcr genes are reported in E. coli, Klebsiella pneumoniae, K. oxytoca, Salmonella enterica, Enterobacter spp., Shigella spp., Citrobacter freundii, Cronobacter spp., and Aeromonas spp.
Mechanism of Conferring Resistance
- The mcr genes confer resistance by modifying the antibiotic (colistin) target site. Colistin binds to the lipopolysaccharide and phospholipid of the bacterial cell membrane and replaces the Ca2+ and Mg+2 leading to the disruption of the cell membrane and leaking of the internal contents causing bacteria to die.
- The mcr genes encode for Mobilized Colistin Resistant proteins (MCR proteins). These proteins are phosphoethanolamine (PEA) transferase enzymes that catalyze the addition of the phosphoethanolamine moiety from a phospholipid found in the bacterial membrane, called the phosphatidylethanolamine, to the head of lipid A. This modification of lipid A reduces the affinity of colistin to the lipopolysaccharide (LPS) rending the bacterium resistance against colistin.
Detection Method
- Although several methods have been devised to detect colistin resistance in bacteria, the detection of the mcr genes primarily depends on the PCR method. For the PCR, different primers have been used, some of which are tabulated below.
| mcr gene types | Primers | References |
| mcr-1 gene | F: 5′‐AGTCCGTTTGTTCTTGTGGC‐3′ R: 5′‐AGATCCTTGGTCTCGGCTTG‐3′ | Rebelo, A. R. , Bortolaia, V. , Kjeldgaard, J. S. , Pedersen, S. K. , Leekitcharoenphon, P. , Hansen, I. M. , … Hendriksen, R. S. (2018). Multiplex PCR for detection of plasmid‐mediated mcr‐4 and mcr‐5 for surveillance purposes. Eurosurveillance Weekly, 23, pii: 17‐00672 10.2807/1560-7917.es.2018.23.6.17-00672 |
| mcr-1 gene | F: 5′‐ACGCCATCTGCAACACCAA‐3′ R: 5′‐ GCCAACGAGCATACCGACAT‐3′ | Dona, V. , Bernasconi, O. J. , Kasraian, S. , Tinguely, R. , & Endimiani, A. (2017). A SYBR(R) Green‐based real‐time PCR method for improved detection of mcr‐1‐mediated colistin resistance in human stool samples. Journal of Global Antimicrobial Resistance, 9, 57–60. 10.1016/j.jgar.2017.01.007 |
| mcr-1 gene | F: 5′‐ATGATGCAGCATACTTCTGTGTG‐3′ R: 5′‐TCAGCGGATGAATGCGGTGC‐3′ | Bontron, S. , Poirel, L. , & Nordmann, P. (2016). Real‐time PCR for detection of plasmid‐mediated polymyxin resistance (mcr‐1) from cultured bacteria and stools. Journal of Antimicrobial Chemotherapy, 71, 2318–2320. 10.1093/jac/dkw139 |
| mcr-2 gene | F: 5′‐CAAGTGTGTTGGTCGCAGTT‐3′ R: 5′‐TCTAGCCCGACAAGCATACC‐3′ | Rebelo, A. R. , Bortolaia, V. , Kjeldgaard, J. S. , Pedersen, S. K. , Leekitcharoenphon, P. , Hansen, I. M. , … Hendriksen, R. S. (2018). Multiplex PCR for detection of plasmid‐mediated mcr‐4 and mcr‐5 for surveillance purposes. Eurosurveillance Weekly, 23, pii: 17‐00672 10.2807/1560-7917.es.2018.23.6.17-00672 |
| mcr-3 gene | F: 5′‐AAATAAAAATTGTTCCGCTTATG‐3′ R: 5′‐AATGGAGATCCCCGTTTTT‐3′ | Sekyere, J. O. (2019). Mcr colistin resistance gene: a systematic review of current diagnostics and detection methods. MicrobiologyOpen, 8(4). https://doi.org/10.1002/mbo3.682 |
| mcr-4 gene | F: 5′‐TCACTTTCATCACTGCGTTG‐3′ R: 5′‐TTGGTCCATGACTACCAATG‐3′ | Sekyere, J. O. (2019). Mcr colistin resistance gene: a systematic review of current diagnostics and detection methods. MicrobiologyOpen, 8(4). https://doi.org/10.1002/mbo3.682 |
References
- Prasad Sah, R. S., Dhungel, B., Yadav, B. K., Adhikari, N., Shrestha, U. T., Lekhak, B., Banjara, M. R., Adhikari, B., Ghimire, P., & Rijal, K. R. (2021). Detection of TEM and CTX-M Genes in Escherichia coli Isolated from Clinical Specimens at Tertiary Care Heart Hospital, Kathmandu, Nepal. Diseases, 9(1). https://doi.org/10.3390/diseases9010015
- Saif Jabbar ALzubaidi, and Marwa Hameed Alkhafaji. Molecular Detection of bla TEM and bla CTX-M Genes in Clinical and Food-Borne Klebsiella pneumoniae Isolates. J. Med. Chem. Sci. 2023, 6(7) 1706-1713. Manuscript ID: JMCS-2211-1869. DOI:10.26655/JMCHEMSCI.2023.7.20
- Salverda ML, De Visser JA, Barlow M. Natural evolution of TEM-1 β-lactamase: experimental reconstruction and clinical relevance. FEMS Microbiol Rev. 2010 Nov;34(6):1015-36. doi: 10.1111/j.1574-6976.2010.00222.x. PMID: 20412308.
- National Center for Biotechnology Information (2022). PubChem Protein Summary for ProteinBlob P62593, Beta-lactamase TEM (E. coli). Retrieved December 28, 2022 from https://pubchem.ncbi.nlm.nih.gov/protein/P62593.
- Tamma, P. D., Smith, T. T., Adebayo, A., Karaba, S. M., Jacobs, E., Wakefield, T., Nguyen, K., Whitfield, N. N., & Simner, P. J. (2021). Prevalence of blaCTX-M Genes in Gram-Negative Bloodstream Isolates across 66 Hospitals in the United States. Journal of Clinical Microbiology, 59(6). https://doi.org/10.1128/JCM.00127-21
- Girlich, D., Bonnin, R. A., & Naas, T. (2020). Occurrence and Diversity of CTX-M-Producing Escherichia coli From the Seine River. Frontiers in Microbiology, 11. https://doi.org/10.3389/fmicb.2020.603578
- Microsoft Word – ctx-m-beta-lactamases.doc (microrao.com)
- Nuno Mendonça; Marie-Hélène Nicolas-Chanoine; Manuela Caniça (2009). Diversity of the blaSHV genes. , 65(4), 0–446. doi:10.1016/j.diagmicrobio.2009.08.005
- Hammond, D. S., Schooneveldt, J. M., Nimmo, G. R., Huygens, F., & Giffard, P. M. (2005). blaSHV Genes in Klebsiella pneumoniae: Different Allele Distributions Are Associated with Different Promoters within Individual Isolates. Antimicrobial Agents and Chemotherapy, 49(1), 256-263. https://doi.org/10.1128/AAC.49.1.256-263.2005
- Liakopoulos, A., Mevius, D., & Ceccarelli, D. (2016). A Review of SHV Extended-Spectrum β-Lactamases: Neglected Yet Ubiquitous. Frontiers in Microbiology, 7. https://doi.org/10.3389/fmicb.2016.01374
- Dong, Yuanyuan; Sheng, Haihui; Zeng, Xainting; Yan, Jufen; Li, Haiyan; Xiao, Huasheng; Li, Xiaokun; Yang, Shulin (2012). Investigation of Genetic Diversity of the bla SHV Gene and Development of an Oligonucleotide Microarray to Detect Mutations in the bla SHV Gene. Microbial Drug Resistance, 18(6), 539–545. doi:10.1089/mdr.2012.0057
- Perovic, Olga & Singh-Moodley, Ashika & Duse, Adriano & Bamford, Colleen & Elliott, G & Swe Swe, Khine & Kularatne, Ranmini & Lowman, Warren & Whitelaw, Andrew & Nana, Trusha & Wadula, Jeannette & Lekalakala, Molebogeng & Saif, Adrienne & De-Smit, Melony & Marais, Else. (2014). National sentinel site surveillance for antimicrobial resistance in Klebsiella pneumoniae isolates in South Africa, 2010 – 2012. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 104. 10.7196/samj.7617.
- Nowak P, Paluchowska P, Budak A. Distribution of blaOXA genes among carbapenem-resistant Acinetobacter baumannii nosocomial strains in Poland. New Microbiol. 2012 Jul;35(3):317-25. Epub 2012 Jun 30. PMID: 22842601.
- Evans, B. A., & Amyes, G. B. (2014). OXA β-Lactamases. Clinical Microbiology Reviews, 27(2), 241-263. https://doi.org/10.1128/CMR.00117-13
- Thierry Naas, Garance Cotellon, Ayla Ergani, Patrice Nordmann, Real-time PCR for detection of blaOXA-48 genes from stools, Journal of Antimicrobial Chemotherapy, Volume 68, Issue 1, January 2013, Pages 101–104, https://doi.org/10.1093/jac/dks340
- Gurung, S., Kafle, S., Dhungel, B., Adhikari, N., Shrestha, U. T., Adhikari, B., Banjara, M. R., Rijal, K. R., & Ghimire, P. (2020). Detection of OXA-48 Gene in Carbapenem-Resistant Escherichia coli and Klebsiella pneumoniae from Urine Samples. Infection and Drug Resistance, 13, 2311-2321. https://doi.org/10.2147/IDR.S259967
- Tabbouche, Sana & Rami, Khudary & Beyrouthy, Racha & Dabboussi, Fouad & Marcel, Achkar & Hassan, Mallat & Hlais, Sani & Monzer, Hilana. (2011). Detection of genes TEM, OXA, SHV and CTX-M in 73 clinical isolates of Escherichia coli producers of extended spectrum Beta-lactamases and determination of their susceptibility to antibiotics. International Arabic Journal of Antimicrobial Agents. 1.
- Bhattacharjee, Amitabha & Sen, Malay & Anupurba, Shampa & Prakash, Pradyot & Nath, Gopal. (2007). Detection of OXA-2 group extended-spectrum- β-lactamase-producing clinical isolates of Escherichia coli from India. The Journal of antimicrobial chemotherapy. 60. 703-4. 10.1093/jac/dkm267.
- Senda, K., Arakawa, Y., Ichiyama, S., Nakashima, K., Ito, H., Ohsuka, S., Shimokata, K., Kato, N., & Ohta, M. (1996). PCR detection of metallo-beta-lactamase gene (blaIMP) in gram-negative rods resistant to broad-spectrum beta-lactams. Journal of Clinical Microbiology, 34(12), 2909-2913. https://doi.org/10.1128/jcm.34.12.2909-2913.1996
- Dwomoh, F. P., Kotey, C. N., Dayie, K. D., Osei, M., Amoa-Owusu, F., Bannah, V., Alzahrani, F. M., Halawani, I. F., Alzahrani, K. J., Egyir, B., & Donkor, E. S. (2022). Phenotypic and genotypic detection of carbapenemase-producing Escherichia coli and Klebsiella pneumoniae in Accra, Ghana. PLOS ONE, 17(12), e0279715. https://doi.org/10.1371/journal.pone.0279715
- Ghazaei C. Molecular Detection of Metallo-β-lactamase Genes blaIMP, blaVim, and blaSPM-1 in Bacillus cereus Strains Isolated from Infant Milk Powder Samples. Int J Infect.6(3):e95266. doi: 10.5812/iji.95266.
- Abbas S, Ejaz H, Jahan S, Younas S, Alzahrani B, Farraj DAA, Alkufeidy RM. Molecular Detection of blaIMP Genes in Metallo-Beta-Lactamase Producing Clinical Gram-Negative Isolates. Clin Lab. 2019 Aug 1;65(8). doi: 10.7754/Clin.Lab.2019.190202. PMID: 31414749.
- Beta-lactamase. (2022, December 16). In Wikipedia. https://en.wikipedia.org/wiki/Beta-lactamase
- Poirel L, Walsh TR, Cuvillier V, Nordmann P. Multiplex polymerase chain reaction for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis 2011;70:119–23. doi: 10.1016/j.diagmicrobio.2010.12.002
- Kumari, M., Verma, S., Venkatesh, V., Gupta, P., Tripathi, P., Agarwal, A., Siddiqui, S. S., Arshad, Z., & Prakash, V. (2021). Emergence of blaNDM-1 and blaVIM producing Gram-negative bacilli in ventilator-associated pneumonia at AMR Surveillance Regional Reference Laboratory in India. PLoS ONE, 16(9). https://doi.org/10.1371/journal.pone.0256308
- Goudarzi, Hossein & Hashemi, Ali & Fallah, Fatemeh & Noori, Maryam & Erfanimanesh, Soroor & Yosefi, Neda & Heidary, Mohsen & Khoshnood, Saeed & Houri, Hamidreza. (2016). Detection of blaDIM, blaAIM, blaGIM, blaNDM and blaVIM Genes among Acinetobacter baumannii strains isolated from hospitalized patients in Tehran hospitals, Iran. 2-2016.
- Fatemeh Fallah, Maryam Noori, Ali Hashemi, Hossein Goudarzi, Abdollah Karimi, Soroor Erfanimanesh, Shadi Alimehr, “Prevalence of blaNDM, blaPER, blaVEB, blaIMP, and blaVIM Genes among Acinetobacter baumannii Isolated from Two Hospitals of Tehran, Iran”, Scientifica, vol. 2014, Article ID 245162, 6 pages, 2014. https://doi.org/10.1155/2014/245162
- Aruhomukama, D., Najjuka, C.F., Kajumbula, H. et al. blaVIM- and blaOXA-mediated carbapenem resistance among Acinetobacter baumannii and Pseudomonas aeruginosa isolates from the Mulago hospital intensive care unit in Kampala, Uganda. BMC Infect Dis 19, 853 (2019). https://doi.org/10.1186/s12879-019-4510-5
- Pournaras, S., Tsakris, A., Maniati, M., Tzouvelekis, L. S., & Maniatis, A. N. (2002). Novel Variant (blaVIM-4) of the Metallo-β-Lactamase Gene blaVIM-1 in a Clinical Strain of Pseudomonas aeruginosa. Antimicrobial Agents and Chemotherapy, 46(12), 4026-4028. https://doi.org/10.1128/AAC.46.12.4026-4028.2002
- Ahammad, Z. S., Sreekrishnan, T. R., Hands, C. L., Knapp, C. W., & Graham, D. W. (2014). Increased Waterborne blaNDM-1 Resistance Gene Abundances Associated with Seasonal Human Pilgrimages to the Upper Ganges River. Environmental Science & Technology, 48(5), 3014-3020. https://doi.org/10.1021/es405348h
- AL-Harmoosh, Raad & Jarallah, Eman. (2015). FIRST DETECTION OF THE blaNDM-1 and blaNDM-2 GENES IN A CLINICAL ISOLATES OF Acinetobacter baumannii IN HILLAH HOSPITALS-IRAQ. International Journal of Advanced Research. 3. 1407-1416.
- Naeem, Sohni & Bilal, Hazrat & Muhammad, Hafsah & Khan, Muhammad Asif & Hameed, Fareeha & Bahadur, Sher & Rehman, Tayyab. (2021). Detection of blaNDM-1 gene in ESBL producing Escherichia coli and Klebsiella pneumoniae isolated from urine samples, 2020.. The Journal of Infection in Developing Countries. 15. 10.3855/jidc.12850.
- Fadare, F. T., Adefisoye, M. A., & Okoh, A. I. (2020). Occurrence, identification, and antibiogram signatures of selected Enterobacteriaceae from Tsomo and Tyhume rivers in the Eastern Cape Province, Republic of South Africa. PLoS ONE, 15(12). https://doi.org/10.1371/journal.pone.0238084
- Abbas-Al-Khafaji ZK, Aubais-aljelehawy Qh (2021) Evaluation of antibiotic resistance and prevalence of multi-antibiotic resistant genes among Acinetobacter baumannii strains isolated from patients admitted to al-yarmouk hospital. Cellular, Molecular and Biomedical Reports 1(2):60-68. doi:10.55705/cmbr.2021.142761.1015
- Jacoby, G. A. (2009). AmpC β-Lactamases. Clinical Microbiology Reviews, 22(1), 161-182. https://doi.org/10.1128/CMR.00036-08
- Sana Jamali, Mohd. Shahid, Sobia Farrukh, Anuradha Singh, Haris M. Khan. Molecular characterization of genes encoding AmpC beta-lactamases in clinical isolates of Pseudomonas and Acinetobacter species. J App Pharm Sci, 2015; 5 (10): 048-051.
- Shahid, M., Sobia, F., Singh, A., & Khan, H. M. (2012). Concurrent Occurrence of blaampC Families and blaCTX-M Genogroups and Association with Mobile Genetic Elements ISEcp1, IS26, ISCR1, and sul1-Type Class 1 Integrons in Escherichia coli and Klebsiella pneumoniae Isolates Originating from India. Journal of Clinical Microbiology, 50(5), 1779-1782. https://doi.org/10.1128/JCM.06661-11
- Singh, N. S., Singhal, N., & Virdi, J. S. (2018). Genetic Environment of blaTEM-1, blaCTX-M-15, blaCMY-42 and Characterization of Integrons of Escherichia coli Isolated From an Indian Urban Aquatic Environment. Frontiers in Microbiology, 9. https://doi.org/10.3389/fmicb.2018.00382
- Shacheraghi, Fershteh & shakibaie, mohammad reza & Noveiri, Hanieh. (2010). Molecular identification of ESBL genes blaGES-1 blaVEB-1, blaCTX-M blaOXA-1, blaOXA-4, blaOXA-10 and blaPER-1 in pseudomonas aeruginosa strains isolated from burn patients by PCR, RFLP and sequencing techniques. International Journal Biological & Life Sciences. 6. 138-142.
- Shaw, K. J., Rather, P. N., Sabatelli, F. J., Mann, P., Munayyer, H., Mierzwa, R., Petrikkos, G. L., Hare, R. S., Miller, G. H., Bennett, P., & Downey, P. (1992). Characterization of the chromosomal aac(6′)-Ic gene from Serratia marcescens. Antimicrobial Agents and Chemotherapy, 36(7), 1447-1455. https://doi.org/10.1128/aac.36.7.1447
- WikiGenes – AAC(6′)-Ib – AAC(6′)-Ib
- Galimand, M., Lambert, T., Gerbaud, G.R., & Courvalin, P. (1993). Characterization of the aac(6′)-Ib gene encoding an aminoglycoside 6′-N-acetyltransferase in Pseudomonas aeruginosa BM2656. Antimicrobial Agents and Chemotherapy, 37, 1456 – 1462.
- Frasson, I., Cavallaro, A., Bergo, C. et al. Prevalence of aac(6′)-Ib-cr plasmid-mediated and chromosome-encoded fluoroquinolone resistance in Enterobacteriaceae in Italy. Gut Pathog 3, 12 (2011). https://doi.org/10.1186/1757-4749-3-12
- Ramirez, M. S., Nikolaidis, N., & Tolmasky, M. (2013). Rise and dissemination of aminoglycoside resistance: the aac(6′)-Ib paradigm. Frontiers in Microbiology, 4. https://doi.org/10.3389/fmicb.2013.00121
- Ojdana, Dominika; Sieńko, Anna; Sacha, Paweł; Majewski, Piotr; Wieczorek, Piotr; Wieczorek, Anna; Tryniszewska, Elżbieta (2018). Genetic basis of enzymatic resistance of E. coli to aminoglycosides. Advances in Medical Sciences, 63(1), 9–13. doi:10.1016/j.advms.2017.05.004
- Pansegrau W, et al. 1987. Plasmid 18(3): 193-204. Nucleotide sequence of the kanamycin resistance determinant of plasmid RP4: homology to other aminoglycoside 3′-phosphotransferases.
- Aminoglycoside. (2022, December 7). In Wikipedia. https://en.wikipedia.org/wiki/Aminoglycoside
- Kanamycin kinase. (2022, July 9). In Wikipedia. https://en.wikipedia.org/wiki/Kanamycin_kinase
- Zeng, L.; Jin, S. (2003). aph(3′)-IIb, a Gene Encoding an Aminoglycoside-Modifying Enzyme, Is under the Positive Control of Surrogate Regulator HpaA. Antimicrobial Agents and Chemotherapy, 47(12), 3867–3876. doi:10.1128/AAC.47.12.3867-3876.2003
- The Comprehensive Antibiotic Resistance Database (mcmaster.ca)
- Bontron, S. , Poirel, L. , & Nordmann, P. (2016). Real‐time PCR for detection of plasmid‐mediated polymyxin resistance (mcr‐1) from cultured bacteria and stools. Journal of Antimicrobial Chemotherapy, 71, 2318–2320. 10.1093/jac/dkw139
- Dona, V. , Bernasconi, O. J. , Kasraian, S. , Tinguely, R. , & Endimiani, A. (2017). A SYBR(R) Green‐based real‐time PCR method for improved detection of mcr‐1‐mediated colistin resistance in human stool samples. Journal of Global Antimicrobial Resistance, 9, 57–60. 10.1016/j.jgar.2017.01.007
- Rebelo, A. R. , Bortolaia, V. , Kjeldgaard, J. S. , Pedersen, S. K. , Leekitcharoenphon, P. , Hansen, I. M. , … Hendriksen, R. S. (2018). Multiplex PCR for detection of plasmid‐mediated mcr‐4 and mcr‐5 for surveillance purposes. Eurosurveillance Weekly, 23, pii: 17‐00672 10.2807/1560-7917.es.2018.23.6.17-00672
- Sekyere, J. O. (2019). Mcr colistin resistance gene: a systematic review of current diagnostics and detection methods. MicrobiologyOpen, 8(4). https://doi.org/10.1002/mbo3.682
- Hussein NH, Al-Kadmy IMS, Taha BM, Hussein JD. Mobilized colistin resistance (mcr) genes from 1 to 10: a comprehensive review. Mol Biol Rep. 2021 Mar;48(3):2897-2907. doi: 10.1007/s11033-021-06307-y. Epub 2021 Apr 10. PMID: 33839987.
- Du, C., Feng, Y., Wang, G., Zhang, Z., Hu, H., Yu, Y., Liu, J., Qiu, L., Liu, H., Guo, Z., Huang, J., & Qiu, J. (2020). Co-Occurrence of the mcr-1.1 and mcr-3.7 Genes in a Multidrug-Resistant Escherichia coli Isolate from China. Infection and Drug Resistance, 13, 3649-3655. https://doi.org/10.2147/IDR.S268787
- Hadjadj, L., Riziki, T., Zhu, Y., Li, J., Diene, S. M., & Rolain, M. (2017). Study of mcr-1 Gene-Mediated Colistin Resistance in Enterobacteriaceae Isolated from Humans and Animals in Different Countries. Genes, 8(12). https://doi.org/10.3390/genes8120394
- Mobilized Colistin Resistance (MCR-1) – National Collaborating Centre for Infectious Diseases (nccid.ca)
- (2020). Identification of mobile colistin resistance genes (mcr-1.1, mcr-5 and mcr-8.1) in Enterobacteriaceae and Alcaligenes faecalis of human and animal origin, Nigeria. International Journal of Antimicrobial Agents, 56(3), 106108. https://doi.org/10.1016/j.ijantimicag.2020.106108
- Zhuoren Ling, Wenjuan Yin, Zhangqi Shen, Yang Wang, Jianzhong Shen, Timothy R Walsh, Epidemiology of mobile colistin resistance genes mcr-1 to mcr-9, Journal of Antimicrobial Chemotherapy, Volume 75, Issue 11, November 2020, Pages 3087–3095,
- Newly Reported Gene, mcr-1, Threatens Last-Resort Antibiotics | CDC
- Ngbede EO, Poudel A, Kalalah A, Yang Y, Adekanmbi F, Adikwu AA, Adamu AM, Mamfe LM, Daniel ST, Useh NM, Kwaga JKP, Adah MI, Kelly P, Butaye P, Wang C. Identification of mobile colistin resistance genes (mcr-1.1, mcr-5 and mcr-8.1) in Enterobacteriaceae and Alcaligenes faecalis of human and animal origin, Nigeria. Int J Antimicrob Agents. 2020 Sep;56(3):106108. doi: 10.1016/j.ijantimicag.2020.106108. Epub 2020 Jul 25. PMID: 32721596.
