They are also known as Group A Streptococcus (GAS) or Group A (beta-hemolytic) Streptococcus (GABHS).
Interesting Science Videos
Habitat of Streptococcus pyogenes
- They are found in the throat and skin of humans.
- They are commensals of the upper respiratory tract.
- The Carrier rate of S. pyogenes in the respiratory tract is only few in adults, over 10% in children attending kindergarten.
- Opportunistic pathogens
- May survive in dust for some time.
Morphology of Streptococcus pyogenes
- Gram +ve bacteria
- Spherical or oval cocci in chains.
- 5 to 1 μm in diameter.
- Non-motile
- Non-sporing
- Some of the strains are capsulated, best seen in young cultures.
- The cell wall contains the important component, group-specific carbohydrates.
- Fimbriated
- It has a protein called Protein F.
Genome of Streptococcus pyogenes
- Base pair: 1,852,442
- Protein encoding genes: 1752
- G+C Content: 38.5%
Cultural Characteristics of Streptococcus pyogenes
- Like most Streptococcus species, Streptococcus pyogenes also don’t grow well on a simple medium with basic nutrients. The growth, however, occurs well on agar media supplemented with blood.
- The use of blood agar facilitates the observation of β-hemolysis, which differentiates S. pyogenes from other Streptococcus species.
- S. pyogenes isolated from oral swabs grow well on sucrose-containing agar medium like Trypticase Yeast Extract Cystine with 5% sucrose.
- Other selective media for S. pyogenes include the agar medium like Columbia agar with colistin commonly used for the culture of Gram-positive bacteria.
- In the case of clinical samples, ample growth of typical S. pyogenes typical colonies can be seen after 24 hours at 35-37°C.
- The incubation of blood agar plates in anaerobic or CO2-rich environment often leads to the isolation of non-S. pyogenes β-hemolytic streptococci.
- Strep Selective agar is best for the suppression of commensal respiratory microbiota, including the species of the same genus.
- The optimum temperature for the growth of S. pyogenes is at 37°C, but growth can be seen between 15°C to 40°C.
- The inability of the bacteria to grow at 10°c and 45°C as well as at 6.5% NaCl and 40% bile helps differentiate S. pyogenes from other Streptococcus species.
- The bacteria is an aerobic or facultatively anaerobic bacteria that can tolerate comparatively higher levels of oxygen and can also grow at a low level of oxygen. About 5-10% CO2 during incubation promotes hemolysis on blood agar.
- S. pyogenes also grows well in liquid culture media like Nutrient agar and Glucose broth. The growth is observed in the form of granular turbidity with a powdery deposit as a result of heavy bacterial chains that settle down and form powdery deposits.

Figure: Streptococcus pyogenes inoculated on trypticase soy agar containing 5% defibrinated sheep’s blood. Image Source: CDC/ Richard R. Facklam, Ph.D.
The following are some cultural characteristics of S. pyogenes on different culture media:
1. Nutrient Agar
- The colonies of S. pyogenes on NA appear circular pinpoint with an average diameter of 0.5-1 mm.
- The colonies are light yellow to yellow colored semi-transparent to opaque with low convex or convex elevation with matt surface (in the case of virulent strains) or glossy (in the case of non-virulent strains) and mucoid (in the case of capsule producing strains).
2. Blood Agar
- On blood agar, S. pyogenes form circular pinpoint colonies that are similar in morphology to the colonies formed on other solid agar media.
- Light golden yellow colonies are formed that are surrounded by a clear zone exhibiting β-hemolysis.
- The surface of the colonies differs in different species based on their virulence and production of the capsule.
3. PNF medium
- Circular pinpoint colonies of S. pyogenes are observed on PNF medium that are yellow-colored.
- Like on blood agar, S. pyogenes also produces β-hemolysis around the colonies on the PNF medium.
Virulence factors of Streptococcus pyogenes
A. Antigenic structure
- M protein: rod-like coiled structure with two major structural classes; Class I and Class II; major virulence factor; resist phagocytosis and intracellular killing by polymorphonuclear leukocytes in the absence of antibodies.
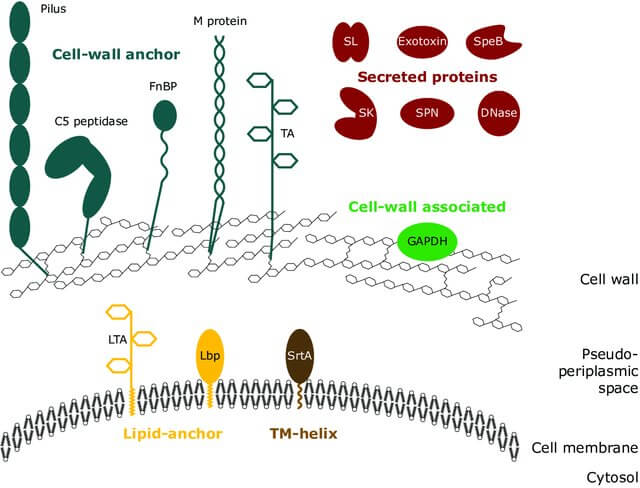
Figure: Virulence factors of Streptococcus pyogenes. Image Source: Christian Linke-Winnebeck.
B. Toxins and enzymes
- Streptokinase
- It is also called fibrinolysin.
- It transforms the plasminogen of human plasma into plasmin, an active proteolytic enzyme that digests fibrin and other proteins, allowing the bacteria to escape from blood clots.
- Deoxyribonucleases
- Streptococcal deoxyribonucleases A, B, C, and D degrades DNA (DNases) and similar to streptokinase facilitate the spread of streptococci in tissue by liquefying pus.
- Hyaluronidase
- Hyaluronidase splits hyaluronic acid, an important component of the ground substance of connective tissue. Thus, hyaluronidase aids in spreading infecting microorganisms (spreading factor).
- Pyrogenic exotoxins (Erythrogenic toxins)
- It acts as superantigens, which stimulate T cells by binding to class II MHC complex, and the activated T cell release cytokines that mediate shock and tissue injury.
- It is associated with Streptococcal toxic shock syndrome and scarlet fever.
- Hemolysins
- Two hemolysins are produced.
- Streptolysin O is oxygen labile and immunogenic in nature. It induces the production of Anti-Streptolysin O(ASO) after the infection with streptococci.
- Streptolysin S is oxygen stable and not immunogenic in nature. It s an agent responsible for the hemolytic zone around the streptococcal colonies on the surface of blood agar.
Clinical manifestation of Streptococcus pyogenes
Disease attributable to invasion by S. pyogenes
1. Erysipelas
- The Portal of entry is skin
- Raised lesion and red
- Brawny edema
2. Cellulitis
- Acute
- Spreading infection of the skin and subcutaneous tissue
- Pain, tenderness, swelling, and erythema
3. Necrotizing fasciitis
- Rapidly spreading necrosis of skin tissue and fascia
4. Puerperal fever
- If the organism enters the uterus after delivery, puerperal fever develops
- Septicemia
5. Bacteremia and sepsis
- Infection of traumatic or surgical wounds with streptococci results in bacteremia, which can rapidly be fatal.
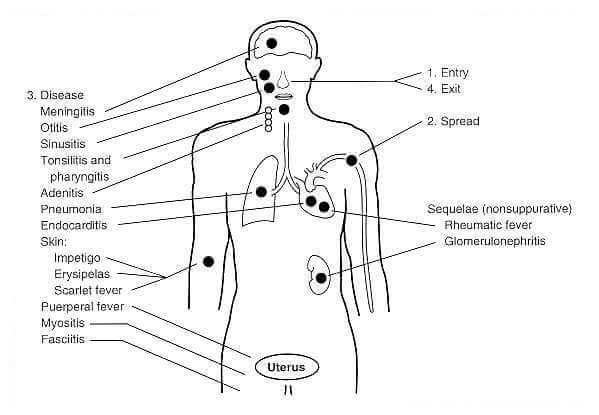
Figure: Pathogenesis of Streptococcus pyogenes infections. Image Source: Kenneth Todar.
Disease attributable to local infection with S. pyogenes and their byproduct
1. Streptococcal sore throat
- Subacute nasopharyngitis
- Thin serous discharge
- Fever
- Infection extends to the middle ear or mastoid
- Enlarged cervical lymph nodes
- Tonsillitis
- Intense redness and edema of mucous membranes
- Purulent exudates
2. Streptococcal pyoderma
- Infection of the superficial layer of skin: impetigo
- Superficial vesicles
- Denuded surface covered with pus and later encrusted
Invasive Group A Streptococcal infection
1. Streptococcal toxic shock syndrome and scarlet fever
- Shock
- Bacteremia
- Respiratory failure
- Multiorgan failure
- Necrotizing fasciitis
- Myositis
- Fever
- Erythema and desquamation
Poststreptococcal disease
1. Acute glomerulonephritis
- Blood and protein in the urine
- Edema
- High blood pressure
- Urea nitrogen retention
- Low serum complement levels
- Chronic form leads to kidney failure
2. Rheumatic fever
- Most serious sequela
- Damage to heart muscles and valves
- Fever
- Malaise
- A migratory non-suppurative polyarthritis
- Inflammation of all parts of the heart ( endocardium, myocardium, and pericardium)
- Thickened and deformed valves.
Laboratory diagnosis of Streptococcus pyogenes
1. Specimens
- Throat swab
- Pus
- Cerebrospinal fluid
- Blood
- Serum for antibody determinant
2. Smear
- Gram staining
- Purple color cocci in a chain arrangement
- Not to be confused with Viridans Streptococci from throat swab sample since both have the same appearance.
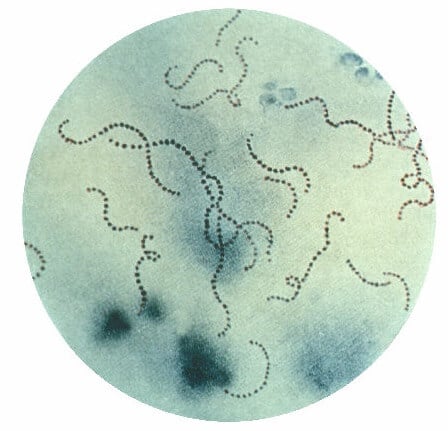
Figure: Photomicrograph of a specimen revealing numbers of chain-linked Streptococcus pyogenes bacteria. Image Source: CDC.
3. Culture
- Culture on blood agar
- Addition of bacitracin in inoculum: S pyogenes are sensitive to bacitracin
- Colonial appearance: Grayish white, transparent to translucent, matte or glossy; smooth; flat; large zone of beta hemolysis
- Catalase negative, oxidase negative, and PYR positive.
4. Antigen detection tests
- Enzyme immunoassay (EIA)
- Agglutination test
- Kits use enzymatic or chemical method to extract antigen from a throat swab and demonstrate the presence of antigen using EIA or agglutination test (visible clumping)
- More sensitive assays are DNA probes and Nucleic acid amplification techniques
5. Serologic tests
- Detection of antibody titer after 3 to 4 weeks after exposure to the organism
- Antibodies include ASO, anti-DNase B, anti- hyaluronidase, antistreptokinase, anti- M type-specific antibodies
- Anti Streptolysin O (ASO) is most widely used.
Treatment of Streptococcus pyogenes infections
- S pyogenes are susceptible to penicillin (benzylpenicillin (penicillin G) or oral phenoxymethylpenicillin (penicillin V).
- For penicillin-allergic patients, erythromycin is the drug of choice.
- In some cases, clindamycin or vancomycin is also recommended.
Prevention and control of Streptococcus pyogenes infections
- Maintenance of personal hygiene
- Chemoprophylaxis: prophylactic use of antibiotics in some streptococcal infections: rheumatic fever.

It’s very useful
It was very helpful and I enjoyed reading