Interesting Science Videos
Structure of Polio Virus
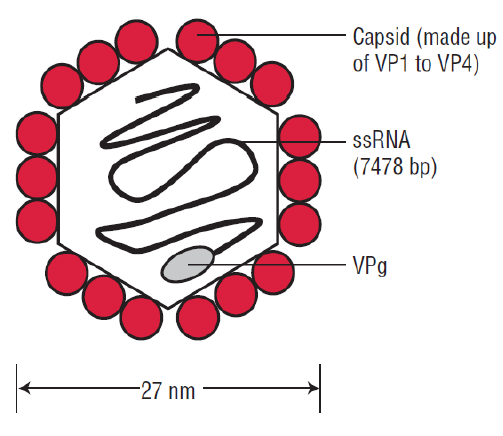
- Poliovirus is a member of a family of viruses called the Picornaviridae.
- Virions are spherical in shape with a diameter of about 27nm.
- The particles are simple in that they are composed of a protein shell surrounding the naked RNA genome.
- The genome is monopartite, linear ssRNA(+) genome of 7.2-8.5 kb, polyadenylated, composed of a single ORF encoding a polyprotein.
- The capsids are composed of four structural proteins: VP1, VP2, VP3, and VP4.
- The basic building block of the picornavirus capsid is the protomer, which contains one copy each of VP1, VP2, VP3, and VP4.
- The shell is formed by VP1 to VP3, and VP4 lies on its inner surface.
- The virus particles lack a lipid envelope, and their infectivity is insensitive to organic solvents.
Genome of Polio Virus
- Polio virus genome can be divided into three parts
- a 5′ noncoding region (NCR) that comprises approximately 10% of the genome, is uncapped, and is covalently linked at the 5′ terminus to viral protein VPg
- a single open reading frame that appears to encode all of the viral proteins, with regions designated as P1 for capsid proteins and P2 and P3 for nonstructural proteins
- a short 3′ NCR terminating in a polyA tail.
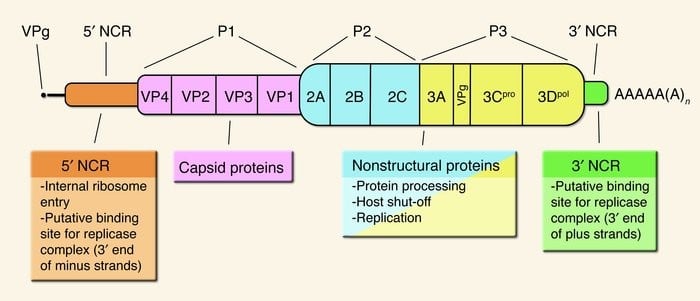
- The genomes vary in length from 7,209 to 8,450 bases.
- The 5′-noncoding region contains the internal ribosome entry site (IRES), an element that directs translation of the mRNA by internal ribosome binding.
- The regions P1 contains four segments for structural proteins which make up the capsid protein; 1A-VP4, 1B- VP2, 1C-VP3, 1D-VP1.
- P2 comprises of three non structural proteins; 2A, 2B, 2C which play a role in viral replication.
- P3 makes up four non structural proteins
- 3A- anchors the replication complex to cell membrane
- 3B- it is VPg protein
- 3C- it is cysteine protease that cleaves the protein from polypeptides
- 3D- it is RNA dependent RNA Polymerase.
Epidemiology of Polio Virus
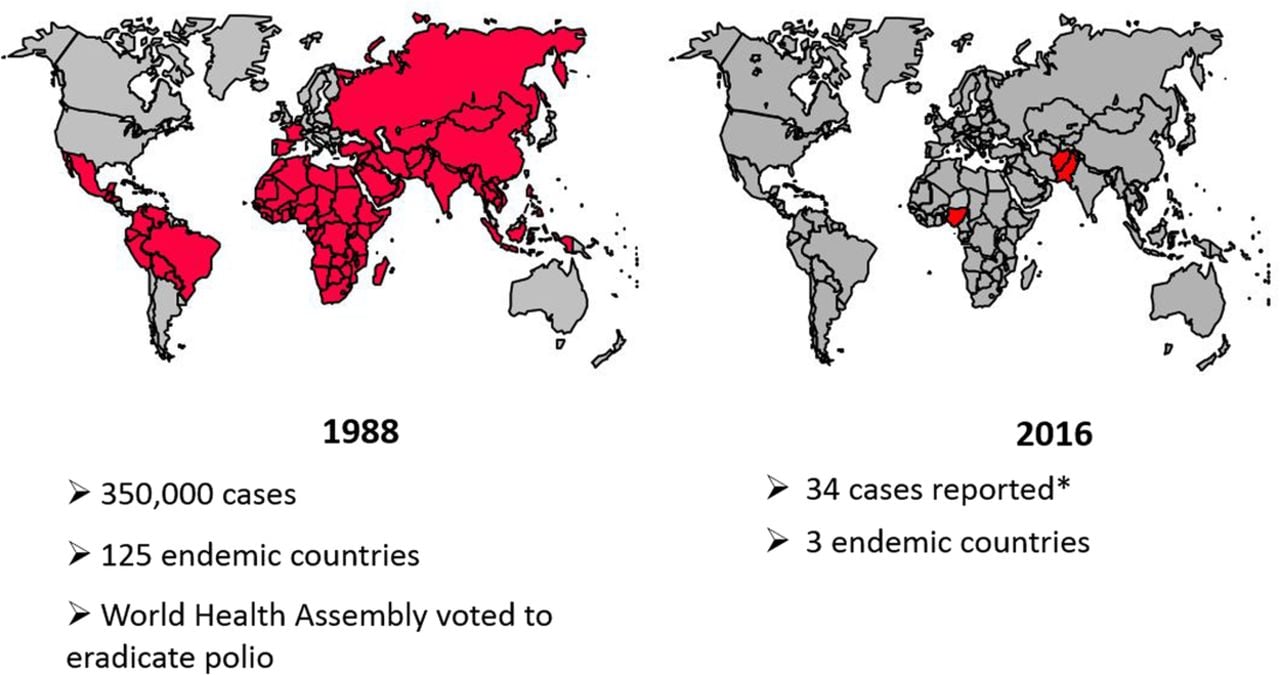
- Poliomyelitis has had three epidemiologic phases: endemic, epidemic, and the vaccine era.
- Before global eradication efforts began, poliomyelitis occurred worldwide—year-round in the tropics and during summer and fall in the temperate zones.
- Winter outbreaks were rare.
- The disease occurs in all age groups, but children are usually more susceptible than adults because of the acquired immunity of the adult population.
- In developing areas, where living conditions favor the wide dissemination of virus, poliomyelitis is a disease of infancy and early childhood (“infantile paralysis”).
- In developed countries, before the advent of vaccination, the age distribution shifted so that most patients were older than age 5 years, and 25% were older than age 15 years.
- The case fatality rate is variable and is highest in the oldest patients and may reach from 5% to 10%.
- Before the beginning of vaccination campaigns in the United States, there were about 21,000 cases of paralytic poliomyelitis per year.
- Humans are the only known reservoir of infection.
- In temperate zones with high levels of hygiene, epidemics have been followed by periods of little spread of virus until sufficient numbers of susceptible children have grown up to provide a pool for transmission in the area.
Replication of Polio Virus
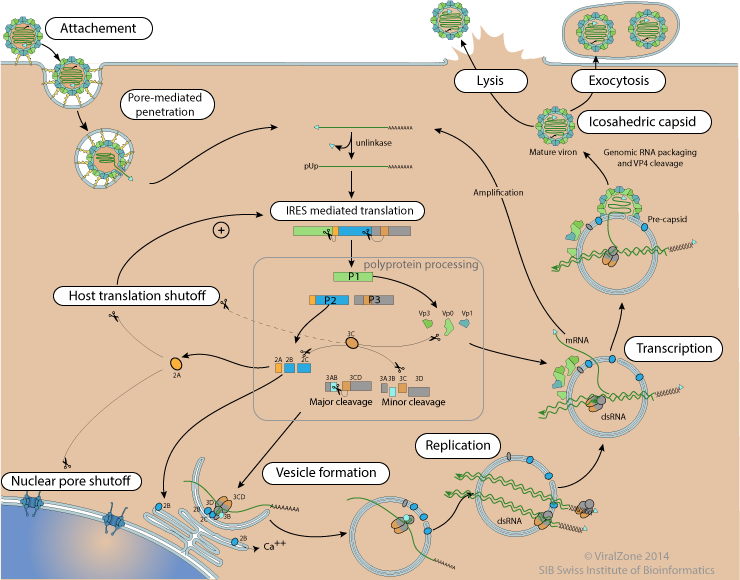
- Virus binds to a cellular receptor and the genome is uncoated.
- VPg is removed from the viral RNA, which is then translated.
- The polyprotein is cleaved nascently to produce individual viral proteins.
- RNA synthesis occurs on membrane vesicles.
- Viral (+) strand RNA is copied by the viral RNA polymerase to form full-length (–) strand RNAs, which are then copied to produce additional (+) strand RNAs.
- Early in infection, newly synthesized (+) strand RNA is translated to produce additional viral proteins.
- Later in infection, the (+) strands enter the morphogenetic pathway.
- Newly synthesized virus particles are released from the cell by lysis.
Pathogenesis of Polio Virus
- The mouth is the portal of entry for the virus, transmitted by fecal oral route on ingestion of contaminated water.
- Virus initially multiply in the oropharynx and gastrointestinal mucosa.
- The virus is regularly present in the throat and in the stools before the onset of illness.
- Virions are resistant to acidity of stomach and to lytic activities of the protease and other enzymes of the intestinal tract and bile.
- On entering the body, the virus infects and multiplies in the tonsils and Peyer’s patch of ileum.
- The incubation period is 9-12 days.
- The virus then spreads to regional lymph nodes and enters the blood causing primary viremia.
- Antibodies to the virus appear early in the disease, usually before paralysis occurs.
- The antibodies are produced to prevent infection from spreading.
- On continued infection and multiplication of virus in the ReticuloEndothelial System (RES), it invades the blood stream causing secondary viremia.
- During this period of viremia, the poliovirus crosses the blood brain barrier and gain access to the brain.
- The virus shows tissue tropism by specifically combining with neural cells.
- The virus recognizes the receptor present on the anterior horn of spinal cord, dorsal root ganglia and motor neurons.
- The destruction of motor neurons leads to paralysis.
- The virus also infects brain stem causing bulbar poliomyelitis.
Clinical Manifestations of Polio Virus
- The earliest features associated with phase of viremia consist of fever, malaise, headache, drowsiness, constipation, and sore throat and lasts for 1 to 5 days.
- Incubation period is usually 10 days but may vary from 4 days to 4 weeks.
- Asymptomatic illness
- It is caused as a result of viral infection confined to the oropharynx and the intestine.
- Abortive poliomyelitis
- It is minor illness occurring in approximately 5% of infected people.
- It is febrile illness characterized by fever, headache, sore throat, loss of appetite, vomiting, and abdominal pain.
- Neurological symptoms are typically absent.
- Non paralytic poliomyelitis
- Some people who develop symptoms from the poliovirus contract a type of polio that doesn’t lead to paralysis (abortive polio).
- This usually causes the same mild, flu-like signs and symptoms typical of other viral illnesses.
- Signs and symptoms, which can last up to 10 days, include: Fever, sore throat, headache, vomiting, fatigue, back pain or stiffness, neck pain or stiffness, pain or stiffness in the arms or legs and muscle weakness or tenderness.
- Paralytic poliomyelitis
- Initial signs and symptoms of paralytic polio, such as fever and headache, often mimic those of non-paralytic polio.
- Within a week, however, other signs and symptoms appear, including: Loss of reflexes, severe muscle aches or weakness and loose and floppy limbs (flaccid paralysis)
- Post poliomyelitis syndrome
- Post-polio syndrome is a cluster of disabling signs and symptoms that affect some people years after having polio.
- Common signs and symptoms include: Progressive muscle or joint weakness and pain, fatigue, muscle wasting (atrophy), breathing or swallowing problems, sleep-related breathing disorder; such as sleep apnea, and decreased tolerance of cold temperatures.
- Bulbar poliomyelitis
- This is caused due to involvement of the cranial nerves, most commonly 9th, 10th, and 12th.
- This condition tends to be more severe with involvement of the muscles of the pharynx, vocal cords and respiration.
- The condition may cause death in 75% of the patient.
Laboratory Diagnosis of Polio Virus
Specimen: stool, rectal swab, throat swab, CSF (rare)
- Microscopy
- Virus can be detected in stool specimens by direct electron microscopy or also by immune electron microscopy.
- Although virus is rarely demonstrated in CSF, microscopy of CSF demonstrates predominantly lymphocytic pleocytosis.
- Virus isolation
- Virus may be recovered from pharyangeal aspirations and feces.
- Virus isolation from feces and throat swab is carried out by cultivation on monkey kidney, human amnion, HeLa cells, Hep-2, Buffalo green monkey (BGM), MRC-5 and other cell cultures.
- Cytopathogenic effects appear in 3–6 days.
- Cytopathic effects include cell retraction, increased refractivity, cytoplasmic granularity, and nuclear pyknosis.
- An isolated virus is identified and typed by neutralization with specific antiserum.
- Serodiagnosis
- Demonstration of fourfold increase of antibody titer in the serum sample collected at the time of acute illness and time of convalescence.
- Neutralization test and complement fixation test is carried out to demonstrate antibodies presence.
- Molecular diagnosis
- Virus can also be identified more rapidly by polymerase chain reaction (PCR) assays.
Treatment of Polio Virus
- No antiviral treatments are available for the treatment of poliomyelitis.
Prevention and Control of Polio Virus
- Provision of clean water, improved hygienic practices and sanitation are important for reducing the risk of transmission in endemic countries.
- Immunization is the cornerstone of polio eradication and both live-virus and killed-virus vaccines are available.
- Formalin-inactivated vaccine (Salk) is prepared from virus grown in monkey kidney cultures.
- Killed-virus vaccine induces humoral antibodies but does not induce local intestinal immunity so that virus is still able to multiply in the gut.
- Live attenuated vaccine (Sabin) is grown in primary monkey or human diploid cell cultures and delivered orally.
- The live polio vaccine infects, multiplies, and immunizes the host against virulent strains.
- The vaccine produces not only immunoglobulin M (IgM) and IgG antibodies in the blood but also secretory IgA antibodies in the intestine, enabling mucosal immunity.
- Both killed-virus and live-virus vaccines induce antibodies and protect the CNS from subsequent invasion by wild virus.
- Oral polio vaccine has been the vaccine used predominantly in the past in global campaigns and is still used in endemic areas.
- It has the advantages of inducing both humoral and intestinal immunity and of being cheap and easy to administer.
- However, the gut develops a far greater degree of resistance after administration of live-virus vaccine indicating it as a potential limiting factor of interference for oral vaccine.
- The disadvantage is the small risk of vaccine associated paralytic poliomyelitis (VAPP), which occurs in about 4 out of every 1,000,000 vaccinated children and unvaccinated contacts.
- Inactivated poliovirus vaccine is injected intramuscularly and does not carry any risk of VAPP.
- The disadvantage of inactivated vaccine is that it does not confer intestinal immunity and is not effective for outbreak control and is more expensive and requires better trained staff for deliverance.
- European countries have gradually shifted from OPV to IPV over the last decades and today all EU Member States use IPV in their childhood immunization programmes.

neat and well defined