Interesting Science Videos
What is Sterilization?
- Sterilization is the complete removal of microorganisms from an object or surfaces.
- Sterilization is obtained when microorganisms are subjected to antimicrobial agents for sufficient time and at optimum conditions.
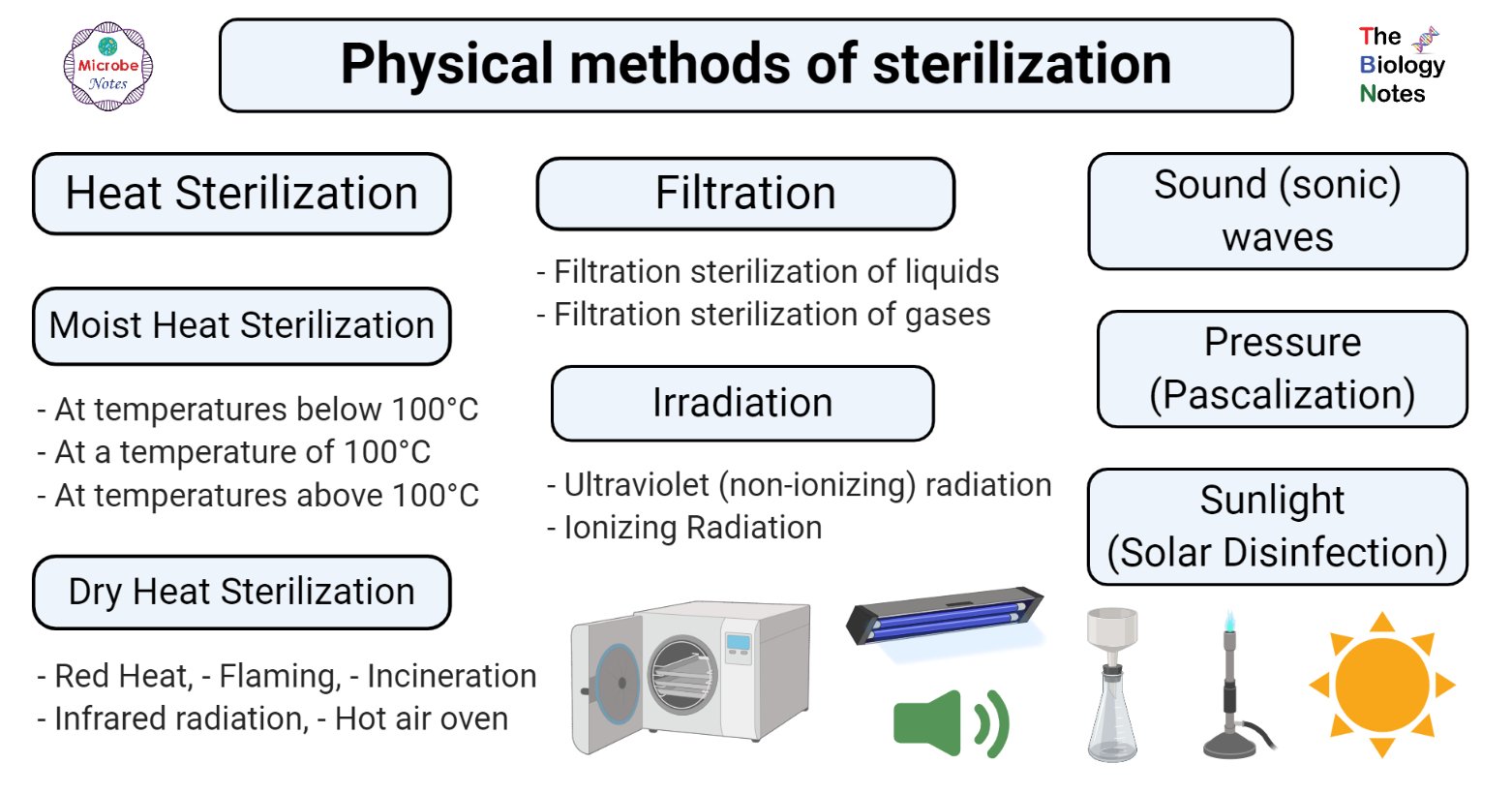
Figure: Physical methods of sterilization. Image created using biorender.com
Some physical methods associated with sterilization are explained below:
Heat Sterilization
- Heat sterilization is the most effective and widely used method of sterilization, where the bactericidal activity results through the destruction of enzymes and other essential cell constituents.
- The effects of heat sterilization occur more rapidly in a fully hydrated state, as it requires a lower heat input, with low temperature and less time, under high humidity conditions where the denaturation and hydrolysis reactions are predominant, rather than in the dry state where oxidative changes take place.
- Under circumstances where thermal degradation of a product is possible, it can usually be minimized by adopting a higher temperature range, as the shorter exposure times generally result in a lower partial degradation.
- This method of sterilization is applicable to thermostable products. Still, it can be applied to both moisture-sensitive and moisture-resistant products, for which dry (160–180°C) and moist (121–134°C) heat sterilization procedures are respectively used.
Moist Heat Sterilization
- Moist heat sterilization is one of the most effective methods of sterilization where the steam under pressure acts as a bactericidal agent.
- Moist heat sterilization usually involves the use of steam at temperatures in the range 121–134°C.
- High pressure increases the boiling point of water and thus helps achieve a higher temperature for sterilization.
- High pressure also facilitates the rapid penetration of heat into deeper parts of material and moisture present in the steam causes the coagulation of proteins causing an irreversible loss of function and activity of microbes.
- The high temperature-short time cycles not only often result in lower fractional degradation, but they also provide the advantage of achieving higher levels of sterility assurance due to more significant inactivation factors.
- The most commonly used standard temperature-time cycles for clinical porous specimens (e.g. surgical dressings) and bottled fluids are 134°C for 3 minutes and 121°C for 15 minutes, respectively.
- An autoclave is a device that works on the principle of moist heat sterilization through the generation of steam under pressure.
- In this method, the microorganisms are killed by coagulating their proteins, and this method is much more effective than dry heat sterilization where microbes are killed through oxidation.
- In the pharmaceutical and medical sectors, it is used in the sterilization of dressings, sheets, surgical and diagnostic equipment, containers, and aqueous injections, ophthalmic preparations, and irrigation fluids, in addition to the processing of soiled and contaminated items.
- Moist heat can be used in sterilization at different temperatures:
At temperatures below 100°C
- The sterilization technique employed at a temperature below 100°C involves pasteurization.
- In this process, all non-spore forming microbes are killed in milk by subjecting the milk to a temperature of 63°C for 30 minutes (the holder method) or 73°C for 20 seconds (the flash method).
- In pasteurization, however, not all the pathogenic organisms are killed. The principle of pasteurization is the logarithmic reduction in the number of viable microbes so that they can no longer cause diseases.
- All mesophilic non-sporing bacteria can be killed by exposure to a moist heat at 60C for half an hour with the exception of some organisms which require different temperature-time cycles.
- The milk is not heated above its boiling point as the milk might curdle, and its nutritional value might be destroyed.
- Besides milk, other fluids and equipment like vaccines of non-sporing bacteria are also pasteurized at 60°C for 1 hour in special water baths.
- Similarly, serum and body fluids with congealable proteins are also sterilized at 56°C for 1 hour in water baths.
At a temperature of 100°C
- Boiling at 100°C is a moist heat sterilization technique that doesn’t ensure complete sterility, but is enough for the removal of pathogenic vegetative microbes and some spores.
- In this case, the items to be sterilized are immersed in boiling distilled water for 30-40 minutes.
- Distilled water is preferred because hard water might result in the formation of a film of calcium salts on the instruments.
- Tyndallization is a method that is used for sterilization of media with sugar and gelatin at 100°C for 30 minutes on three successive days so as to preserve sugar which might be decomposed at a higher temperature.
- Moist heat at 100°C is applicable for contaminated dishes, beddings, pipettes, and other instruments that are not soiled or contaminated as well as for objects that are temperature sensitive.
At temperatures above 100°C
- Moist heat sterilization above 100°C involves sterilization by steam under pressure.
- Water usually boils at 100°C under normal atmospheric pressure (760 mm of Hg); however, the boiling point of water increases if the pressure is to be increased.
- This principle is employed in an autoclave where the water boils at 121°C at the pressure of 15 psi or 775 mm of Hg.
- As a result, the steam under pressure has a higher penetrating power. When this steam comes in contact on the surface, it kills the microbes by giving off latent heat.
- The condensed liquid ensures the moist killing of the microbes.
- Autoclaves are used for the sterilization of contaminated instruments along with different culture media as it ensures complete sterility.
Dry heat sterilization
- Dry sterilization is the process of removing microorganisms by applying moisture-free heat which is appropriate for moisture-sensitive substances.
- The dry heat sterilization process is based on the principle of conduction; that is the heat is absorbed by the outer surface of an item and then passed onward to the next layer. Ultimately, the entire item reaches the proper temperature needed to achieve sterilization.
- Dry moisture-less heat destroys microorganisms by causing denaturation of proteins and also lyses the proteins in many organisms, causes oxidative free radical damage, causes drying of cells, and can even burn them to ashes, as in incineration
- Dry heat sterilization is used for the sterilization of materials which are difficult to sterilize by moist heat sterilization for several reasons.
- Substances like oil, powder, and related products cannot be sterilized by moist heat because moisture cannot penetrate into deeper parts of oily materials, and powders are destroyed by moisture.
- Similarly, laboratory equipment like Petri dishes and pipettes are challenging to sterilize by moist heat due to the penetration problem.
- The lethal effects of dry heat on microorganisms are primarily due to oxidative processes which are less effective when compared to the hydrolytic damage that results from exposure to steam in moist heat sterilization.
- Thus, in dry heat sterilization usually higher temperatures in the range 160–180°C are employed and also require exposure times of up to 2 hours depending upon the temperature employed.
- This principle is used in instruments like hot air oven and incineration, which generates very hot moisture-free air.
- The primary industrial application of dry heat sterilization is in the sterilization of glass bottles which are to be filled aseptically.
- In addition to the fact that this method achieves an adequate sterility assurance level, this method also destroys bacterial endotoxins (which are the products of Gram-negative bacteria also called pyrogens, which cause fever when injected into the body) which are difficult to eliminate through other sterilization techniques.
- For the purposes of depyrogenation of glass, temperatures of approximately 250°C are used.
- There are different types of dry heat sterilization which are explained below:
Red Heat
- Rest heat sterilization is the process of instant sterilization by holding the instruments in a Bunsen flame till they become red hot.
- This method is based on dry heat sterilization is commonly used for sterilization of instruments like incubation loops, wires, and points of forceps.
- This process ensures effective sterilization; however, it is only limited to substances that can endure heating until redness in flame.
Flaming
- Flaming is a type of dry sterilization that involves exposure of metallic objects to flame for some time where the flame burns microbes and other dust presents in the instrument.
- In the case of flaming, the instrument is dipped in alcohol or spirit before burning it in a gas flame.
- This process doesn’t ensure sterility and is not as effective as red hot sterilization.
Incineration
- Incineration is the process of sterilization along with a significant reduction in the volume of the wastes. It is usually conducted during the final disposal of the hospital or other residues.
- The scraps are heated till they become ash which is then disposed of later.
- This process is conducted in a device called incinerator.
Infrared radiation
- Infrared radiation (IR) is a method of thermal sterilization in which the radiation is absorbed and then converted into heat energy.
- For this purpose, a tunnel containing an IR source is used. The instruments and glassware to be sterilized are kept in a tray are then passed through the tunnel on a conveyer belt, moving at a controlled speed.
- During this movement, the instruments will be exposed to the radiation, which will result in a temperature of about 180°C for about 17 minutes.
- IR is applicable for mass sterilization of packaged items like syringes and catheters.
Hot air oven
- Hot air oven is a method of dry heat sterilization which allows the sterilization of objects that cannot be sterilized by moist heat.
- It uses the principle of conduction in which the heat is first absorbed by the outer surface and is then passed into the inner layer.
- A hot air oven consists of an insulated chamber that contains a fan, thermocouples, temperature sensor, shelves and door locking controls.
- The commonly-used temperatures and time that hot air ovens need to sterilize materials are 170°C for 30 minutes, 160°C for 60 minutes, and 150°C for 150 minutes.
- These ovens have applications in the sterilization of glassware, Petri plates, and even powder samples.
Filtration
- The process of filtration is unique among sterilization techniques in that it removes, rather than destroys, microorganisms.
- Further, it is capable of preventing the passage of both viable and nonviable particles and can thus be used for both the clarification and sterilization of liquids and gases.
- The primary mechanisms involved in filtration are sieving, adsorption, and trapping within the matrix of the filter material.
- Filtration uses membranous filters that have tiny pores that let the liquid pass through but prevent bigger particles such as bacteria from passing through the filter. Therefore, the smaller the pore, the more likely the filter is to stop more things from going through it.
- Certain types of filter (membrane filters) also have an essential role in sterility testing, where they can be employed to trap and concentrate contaminating organisms from solutions under test.
- These filters are then placed in a liquid nutrient medium and incubated to encourage growth and turbidity.
- The principal application of sterilizing-grade filters is the treatment of heat-sensitive injections and ophthalmic solutions, biological products, air, and other gases for supply to aseptic areas.
- They may also be required in industrial applications where they become part of venting systems on fermenters, centrifuges, autoclaves, and freeze dryers.
Filtration sterilization of liquids
- Membrane filters, in the form of discs, can be assembled into pressure-operated filter holders for syringe mounting and in-line use or vacuum filtration tower devices for filtration of liquid.
- Filtration under pressure is generally considered most suitable, as filling at high flow rates directly into the final containers is possible without problems of foaming, solvent evaporation, or air leaks.
- Membrane filters are often used in combination with a coarse-grade fiberglass depth prefilter to improve their dirt-handling capacity.
Filtration sterilization of gases
- Filters employed for this generally consist of pleated sheets of glass microfibres separated and supported by corrugated sheets of Kraft paper or aluminum which are employed in ducts, wall or ceiling panels, or laminar air flow cabinets.
- These high-efficiency particulate air (HEPA) filters can remove up to 99.997% of particles >0.3mm in diameter and thus are acting as depth filters.
- In practice, their microorganism removal efficiency is rather better as the majority of bacteria are found associated with dust particles.
- Other applications of filters include sterilization of venting or displacement air in tissue and microbiological culture (carbon filters and hydrophobic membrane filters); decontamination of air in mechanical ventilators (glass fiber filters); treatment of exhausting air from microbiological safety cabinets (HEPA filters); and the clarification and sterilization of medical gases (glass wool depth filters and hydrophobic membrane filters).
Irradiation
- Irradiation is the process of exposing surfaces and objects to different kinds of radiation for sterilization.
- Mainly electromagnetic radiation is used for sterilization.
- The major target for these radiations is considered to be microbial DNA, where damage occurs as a result of ionization and free radical production (gamma-rays and electrons) or excitation (UV light).
Ultraviolet (non-ionizing) radiation
- Ultraviolet radiation includes light rays from 150-3900 Å, of which 2600 Å has the highest bactericidal effect.
- Non-ionizing waves have a very little penetration power, so microorganisms only on the surface are killed.
- Upon exposure, these waves are absorbed by many materials, particularly nucleic acids.
- The waves, as a result, cause the formation of pyrimidine dimers which bring error in DNA replication and cause the death of microbes by mutation.
- UV radiation owing to its poor penetrability of conventional packaging materials is unsuitable for sterilization of pharmaceutical dosage forms.
- It is, however, applied in the sterilization of air, for the surface sterilization of aseptic work areas, and the treatment of manufacturing-grade water.
Ionizing Radiation
- X-ray and gamma rays are the commonly used ionizing radiation for sterilization.
- These are high energy radiation which causes ionization of various substances along with water.
- The ionization results in the formation of a large number of toxic O2 metabolites like hydroxyl radical, superoxide ion, and H2O2 through ionization of water.
- These metabolites are highly oxidizing agents and kill microorganisms by oxidizing various cellular components.
- With ionizing radiation, microbial resistance decreases with the presence of moisture or dissolved oxygen (as a result of increased free radical production) and also with elevated temperatures.
- Radiation sterilization is generally exposed to items in the dried state which include surgical instruments, sutures, prostheses, unit-dose ointments, plastic syringes, and dry pharmaceutical products.
Sound (sonic) waves Vibration
- Sonic waves can be used as bactericidal agents which employ ultrasound (usually from 20–40 kHz) to vibrate a fluid.
- The ultrasound can be used with just water, but the use of a solvent appropriate for the object to be cleaned and the type of soiling present enhances the effect.
- The explanation for the antibacterial activity of airborne sound waves on a physical is based on the possible transformation of acoustic energy into heat.
- The impact of airborne sound differs with the medium as the absorption of acoustic energy is greatly affected by the nature of the medium through which it is transmitted.
- As the sound waves propagate through a detergent solution, these ultrasonic waves produce alternating tensile and compressive forces that oscillate, and these oscillating forces cause millions of microscopically-sized cavities to form in the detergent solution.
- Once they reach a maximum size, these cavities violently collapse, causing submicroscopic voids to form which induce the formation of high-energy hydraulic shock waves.
- These shock waves, which may reach temperatures as high as 10,000°F and hydrodynamic pressures as low as 10,000 PSI, physically loosen and remove microorganisms and other adhering debris from even the most inaccessible surfaces of a contaminated instrument.
- The antibacterial activity of airborne sound waves is directly related to the sound intensity, the period of irradiation, and the distance of the sample from the sound source.
- These sonic waves are found to be effective against bacteria spores depending on the chemical composition of these spores.
- The lipoidal substances within the microbes readily absorb ultrasonic frequencies, and any changes in the lipid level of the test organism directly affect the amount of acoustic energy taken up by the spore as well as the removal of those spores.
- This method is routinely used by healthcare facilities to clean surgical and dental instruments before the terminal sterilization.
Pressure (Pascalization)
- Pascalization or High-Pressure Processing (HPP) is a method employed for preservation and sterilization of food, in which products are processed under very high pressure (hundreds of megapascal), leading to the death of specific microorganisms and inactivation of enzymes in the food.
- HHP treatments may be applied at room temperature, and with the exception of some vegetables, shape, color, and nutrients of most foods are not affected.
- Hydrostatic pressures are nonthermal, and covalent bonds are not broken, so that flavor is unaffected.
- At 400-600 MPa, proteins are easily denatured, and cell morphology is altered, and ribosomes are destroyed.
- Changes occur in the lipid-protein complex of cell membranes, and increased membrane fluidity is also observed, which causes leakage of nucleic acids.
- Pascalization is not particularly effective against spores, but combined treatment with heat is found to be effective in the inactivation of spores.
- Pascalization is especially useful on acidic foods, such as yogurts and fruits, because spores which are pressure-tolerant don’t have the ability to live in environments with low pH.
- The treatment works equally well for both solid and liquid products.
Sunlight (Solar Disinfection)
- Solar disinfection is a process used for the removal of microorganisms with the help of sunlight.
- This process is commonly used to purify or disinfect drinking water.
- Solar disinfection is based on the inactivation of pathogenic organisms as a result of the UV-A (wavelength 320–400 nm) part of the sunlight, which reacts with oxygen dissolved in the water and releases highly reactive forms of oxygen (oxygen free radicals and hydrogen peroxides).
- These metabolites damage pathogens, while it also interferes with metabolism and destroys bacterial cell structures, and simultaneously the full band of solar energy (from infrared to UV) heats the surface.
- The principle of solar disinfection is similar to that of radiation sterilization; however, the efficacy of solar disinfection is significantly low as it requires a long period of exposure.
- However, this process is economical and an environment-friendly option.
References
- Frazier WC and Westhoff DC. Food Microbiology. Tata McGraw Hill Publishing Company Limited. 1995.
- Banwart GJ (1989). Basic Food Microbiology. Chapman & Hall, New York, NY.
- Jay JM (2000). Modern Food Microbiology. CBS Publications and Distribution. Delhi.
- Adams RM and Moss MO (2008). The Royal Society of Chemistry. Cambridge.
- Boyle, C. Sichel, P. Fernández-Ibáñez, G.B. Arias-Quiroz, M. Iriarte Puña, A. Mercado, E. Ubomba-Jaswa, K. G. McGuigan. Bactericidal Effect of Solar Water Disinfection under Real Sunlight Conditions. Applied and Environmental Microbiology May 2008, 74 (10) 2997-3001; DOI: 10.1128/AEM.02415-07
- Pisano, M. A., Boucher, M. G., & Alcamo, I. E. (1966). Sterilizing effects of high-intensity airborne sonic and ultrasonic waves. Applied microbiology, 14(5), 732–736.
- Alkadhim, Saif Aldeen (2018) Hot Air Oven for Sterilization: Definition & Working Principle. SSRN Electronic Journal. doi- 10.2139/ssrn.3340325.
Sources
- 3% – https://www.infectioncontroltoday.com/environmental-hygiene/benefits-ultrasonic-cleaning
- 3% – https://basicmedicalkey.com/sterilization-procedures-and-sterility-assurance/
- 2% – https://www.researchgate.net/publication/315804456_STERILISATION_AND_DISINFECTION
- 2% – http://www.pharmacy180.com/article/filtration-sterilization—sterilization-methods-639/
- 1% – https://www.amazon.ca/Flexzion-Commercial-Ultrasonic-2L-Instruments/dp/B0144E3WPM
- 1% – https://wikimili.com/en/Solar_water_disinfection
- 1% – https://pharmawiki.in/pdf-ppt-hot-air-oven-working-principle-sterilization-diagram-sop-uses-temperature/
- 1% – https://lso-inc.com/svs-site/overview-of-sterilization-methods/
- 1% – https://en.wikipedia.org/wiki/Dry_heat_sterilization
- 1% – https://blog.tuttnauer.com/blog/liquids-sterilization-by-filtration
- 1% – https://aem.asm.org/content/14/5/732
- 1% – http://www.pharmacy180.com/article/radiation-sterilization—sterilization-methods-638/
- 1% – http://www.biologydiscussion.com/micro-biology/clinical-microbiology/sterilisation-and-disinfection-meaning-and-methods/31089
- <1% – https://www.tradelineinc.com/reports/2008-12/air-filtration-and-use-hepa-filters-biological-safety-cabinets
- <1% – https://www.thesprucepets.com/before-you-buy-an-aquarium-filter-1378506
- <1% – https://www.studyread.com/what-is-sterilization-methods/
- <1% – https://www.slideshare.net/zgoutham/high-pressure-processing-of-food
- <1% – https://www.sciencedirect.com/topics/medicine-and-dentistry/endotoxin
- <1% – https://www.sciencedirect.com/topics/food-science/pasteurization
- <1% – https://www.sciencedirect.com/topics/engineering/steam-sterilization
- <1% – https://www.researchgate.net/publication/261143936_Features_Functions_and_selection_of_Pharmaceutical_Packing_Materials
- <1% – https://www.pharmaguideline.com/2011/10/steam-sterilisation-heating-in.html
- <1% – https://www.microrao.com/micronotes/sterilization.pdf
- <1% – https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-guides/microbiological-pharmaceutical-quality-control-labs-793
- <1% – https://www.coursehero.com/file/22230721/chapter-12-micro/
- <1% – https://www.caister.com/spores
- <1% – https://www.britannica.com/science/boiling-point
- <1% – https://upendrats.blogspot.com/2010/03/sterilization-cotrol-of-microorganisms.html
- <1% – https://quizlet.com/20195856/micro-chapter-11-flash-cards/
- <1% – https://quizlet.com/128286840/exam-2-chpt-3-4-flash-cards/
- <1% – https://microbeonline.com/moist-heat-sterilization-definition-principle-advantages-disadvantages/
- <1% – https://en.wikipedia.org/wiki/Ultrasonic_cleaning
- <1% – https://en.wikipedia.org/wiki/Moist_heat
- <1% – https://en.wikipedia.org/wiki/Induction_hardening
- <1% – https://en.wikipedia.org/wiki/Boiling_point
- <1% – https://apps.who.int/phint/pdf/b/7.5.9.5.8-Methods-of-sterilization.pdf
- <1% – https://answers.yahoo.com/question/index?qid=20110102165414AAV8jr0
- <1% – https://answers.yahoo.com/question/index?qid=20100722133323AA1mK65
- <1% – https://answers.yahoo.com/question/index?qid=20061031081405AAFmSW0
- <1% – http://www.romwell.com/cookbook/Preserve/changes.shtml
- <1% – http://www.microrao.com/micronotes/sterilization.pdf
- <1% – http://www.lamission.edu/lifesciences/lecturenote/mic20/Chap07Control.pdf
- <1% – http://www.donaldsonaerospace-defense.com/library/files/documents/pdfs/042665.pdf
- <1% – http://www.authorstream.com/Presentation/jayaraj2775-1367598-sterilization/

Great
Amazing blog. This will be really helpful for the people working in Medical labs and Students who need sterilization of surgical instruments.
I am interested in the use of dry steam as a sterlisation method for Meat to keep it looking fresh in the shop window of my butcher’s shop I would appreciate it if you could advise what you think would be the best method of sterilization please,
Robert
So simple to understand thenks alot