Interesting Science Videos
Pathogenesis of Treponema pallidum
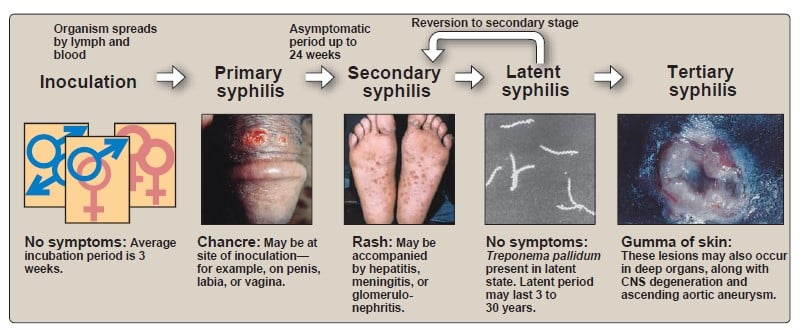
- The two major routes of transmission of Treponema pallidum are sexual and transplacental.
- Sexual exposure to a person who has an active syphilitic chancre carries a high probability of acquiring syphilis.
- The organisms enter a susceptible host by penetration of intact mucous membranes or the minute abrasions in the skin surface that occur during sexual intercourse.
- The organism multiply locally at the site of entry, and some spread to nearby lymph nodes and then reach the bloodstream and may lodge in any organ.
- Within 2–10 weeks after infection, a papule develops at the site of infection and breaks down to form an ulcer with a clean, hard base (“hard chancre”), also called as primary lesion.
- The chancre is painless and most frequently occur on the external genitalia, but it may occur on the cervix, peri-anal area, in the mouth or anal canal.
- Chancres usually occur singly, but in immunocompromised individuals, such as those infected with the Human Immunodeficiency Virus (HIV), multiple or persistent chancres may develop.
- Dissemination of the organism occurs during this primary stage; once the organism has reached a sufficient number.
- This “primary lesion” always heals spontaneously, but 2–10 weeks later, the “secondary” lesions appear.
- These are highly variable and widespread but most commonly involve the skin where macular or pustular lesions develop, particularly on the trunk and extremities.
- During this phase the patient is ill and seeks medical attention.
- Systemic symptoms such as fever, weight loss, malaise, and loss of appetite are present in about half of the patients.
- The lesions of secondary syphilis are highly infectious and these lesions gradually resolve and a period of latent infection is entered, in which no clinical manifestations are evident, but serological evidence of infection persists.
- Relapses are common during early (≤ 1 year) latent syphilis.
- Late latent syphilis (≥ 1 year) is usually asymptomatic and noninfectious.
- Tertiary syphilis is the tissue-destructive phase that appears 10 to 25 years after the initial infection in upto 35% of untreated patients.
- It is a slowly progressive, destructive, inflammatory disease that may affect any organ.
- The three most common forms are neurosyphilis, cardiovascular syphilis and gummatous syphilis – a rare granulomatous lesion of the skeleton, skin or mucocutaneous tissues.
- Treponemes can cross the placental barrier from the bloodstream of an infected mother and cause disease in the fetus where unborn fetus may develop an asymptomatic infection or symptomatic infection with damage to the bone and teeth, deafness, neurosyphilis, or neonatal death.
Clinical manifestations of Treponema pallidum
A. Syphilis
- Primary syphilis
Primary syphilis is characterized by:
- Primary (or hard) chancre which usually begins as a single painless papule that rapidly becomes ulcerated, hard, and indurated, covered by thick exudates. The most common sites are penis (in males), cervix or labia (in females), and anal canal, rectum or mouth (in homosexual).
- Regional (usually inguinal) lymphadenopathy which appears within 1 week of onset of skin lesions.
- Lymph nodes are painless firm, non-suppurative, and often bilateral.
- The chancre generally heals within 4-6 weeks (range 2- 12 weeks), but lymphadenopathy may persist for months.
- Secondary syphilis
- Secondary syphilis results from the systemic spread of the infection when treponemes replicate in the lymph nodes, the liver, joints, muscles, skin, and mucous membranes distant from the site of the primary chancre.
- Skin and mucous membranes are commonly affected and characterized by:
- Skin rashes (palms and soles )
- Condylomata lata (mucocutaneous papules which coalesce to form large pink to grey lesions in warm moist intertriginous areas (such as perianal region, vulva, and scrotum).
- Mucous patches (superficial mucosal erosions)
- Generalized lymphadenopathy is seen.
- The patient may also have syphilitic meningitis, chorioretinitis, hepatitis, nephritis (immune complex type), or periostitis.
- Latent syphilis
- It is characterized with no clinical manifestations but serological evidence of infection persists.
- Latent syphilis is classified as early (high likelihood of relapse) or late (recurrence unlikely).
- Individuals with late latent syphilis are not generally considered infectious, but may still transmit infection to the fetus during pregnancy and their blood may remain infectious.
- Latent syphilis may have one of the following fates: Persistent lifelong infection (common), Development of late syphilis (rare), Spontaneous cure.
- Tertiary syphilis
- Tertiary syphilis is responsible for a majority of the morbidity and mortality associated with the disease.
- The hallmark of tertiary syphilis is the destruction of tissue caused by a response to the presence of treponemal antigens.
- The three most common forms are neurosyphilis, cardiovascular syphilis and gummatous syphilis.
- Gummatous syphilis
- Granulomatous lesions in the skin, bones, and liver
- Neurosyphilis
- Degenerative changes in the central nervous system
- Common manifestations include:
- Meningeal syphilis (meningitis)
- Meningovascular syphilis (vasculitis of arteries leading to embolic stroke)
- General paresis of insane
- Tabes dorsalis (demyelination of the posterior columns)
- Cardiovascular syphilis
- Characterized by aneurysm of ascending aorta and aortic regurgitation (aortitis, aortic aneurysm, aortic valve insufficiency).
B. Congenital syphilis
- A pregnant woman with syphilis can transmit T pallidum to the fetus through the placenta beginning in the 10th –15th weeks of gestation.
- Some of the infected fetuses die, and miscarriages result; others are stillborn at term.
- Congenital anomalies include premature birth, intrauterine growth retardation, and multiple organ failure.
Manifestations of congenital syphilis include:
- Earliest manifestations occur within 2 years of age and affected children are infectious and they suffer from rhinitis (or snuffles), mucocutaneous lesions, bone changes, hepatospleenomegaly and lymphadenopathy.
- Late congenital syphilis occurs after 2 years and is noninfectious.
- It is characterized by interstitial keratitis, eighth-nerve deafness, bilateral knee effusions (Clutton’s joints).
- Residual stigmata may remain for long time such as:
- Hutchinson’s teeth (notched central incisors)
- Mulberry molars
- Saddle nose, and saber shins
- In the congenital infection, the child makes IgM antitreponemal antibody.

Very interested topic, and useful
Thanks very much Dr. It’s very interesing.
Thank you 🙂
Keep up the nice work
The write up is clear and concise, straight to the point, I love it.
Thanks a lot and happy new year to you all. I have picked interest to always read your post and how can I access it.
Thank you so much 🙂