Interesting Science Videos
Pathogenesis of Rickettsia rickettsii
- Human gets infected when infected adult tick inoculates Rickettsia rickettsii into the skin while taking a blood meal.
- It usually takes 6 hours of attachment and feeding before rickettsiae are transmitted to the host. Infection can also be transmitted occasionally by scratching and rubbing infectious tick feces into the abraded skin.
- After inoculation, rickettsiae spread throughout the body via the bloodstream.
- The outer membrane protein A (OmpA) expressed on the surface of R. rickettsii is responsible for the ability of the bacteria to adhere to endothelial cells and induce phagocytosis.
- After the bacteria penetrate into the cell, they are released from the phagosome by degradation of the phagosome membrane by production of a phospholipase C.
- R. rickettsii multiply and are propelled through the cytoplasm by polymerization of the host cell actin at one pole.
- The organisms then spread to other endothelial cells through long cellular projections of the cell membrane.
- The primary clinical manifestation results due to multiplication of rickettsiae in endothelial cells of small blood vessels with subsequent damage to the cells and leakage of the blood vessels and produce vasculitis characterized by lymphocytes that surround the blood vessels.
- The effects of damage to foci of contiguous endothelial cells are visible in the skin, where dilation of the blood vessels first produces a pink rash.
- The cells become swollen and necrotic; there is thrombosis of the vessel, leading to rupture and necrosis.
- Vascular lesions are prominent in the skin, but vasculitis occurs in many organs and appears to be the basis of hemostatic disturbances.
- Hypovolemia and hypoproteinemia caused by the loss of plasma into tissues can lead to reduced perfusion of various organs and organ failure.
- Later, leakage of red blood cells results in hemorrhagic spots (or petechiae), from which the name of the disease is derived.
- Within the blood vessels of the brain, lung, heart, liver, and other visceral organs, these pinpoint hemorrhages lead to encephalitis, pneumonitis, cardiac arrhythmia, nausea, vomiting, and abdominal pain.
- The host immune response to infection is based on cytokine-mediated intracellular killing and clearance of intracellular rickettsiae from the endothelium is achieved through the strong effects of the immune system with important contributions by cell mediated immunity, particularly CD8 lypmphocytes and their cytokines, such as interferon-γ and tumor necrosis factor.
- Antibody response to rickettsial outer membrane proteins may also be important.
Clinical manifestations of Rickettsia rickettsii
Rocky Mountain spotted fever
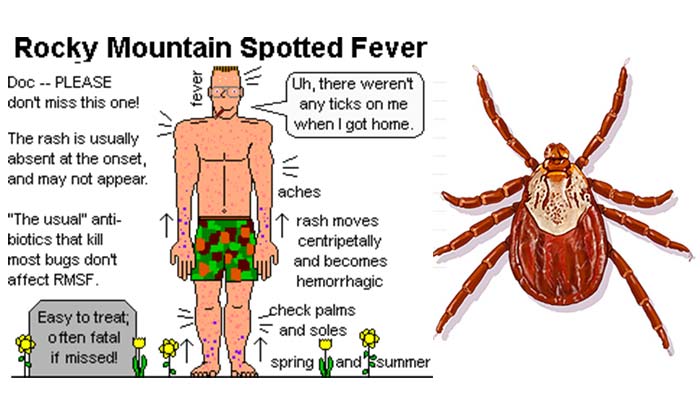
- Rocky Mountain spotted fever is a potentially lethal, but usually curable tickborne disease, and is the most common rickettsial infection caused by Rickettsia rickettsii.
- The disease usually occurs with highest frequency during the warmer months when tick activity is greatest.
- The incubation period is 7 days.
- The onset of disease is heralded by a high fever and headache that may be associated with malaise, myalgias, nausea, vomiting, abdominal pain, and diarrhea.
- A macular rash may develop after three or more days and typically appears initially on wrist, ankles, and palms and soles and then spreads to the trunk.
- The rash can evolve to the “spotted” or petechial form, which is a harbinger of more severe disease and hemorrhagic.
- Complications of Rocky Mountain spotted fever include neurologic manifestations (encephalitis), pulmonary and renal failure, and cardiac abnormalities.
- The patient may die within 5 days of onset of symptoms with the overall mortality rate being nearly 4% despite effective antibiotic therapy.
- Risk factors for fatal infection include older age, glucose-6-phosphate dehydrogenase deficiency and delayed tetracycline treatment.
