Interesting Science Videos
Pathogenesis of Mycoplasma pneumoniae
- M. pneumoniae is an extracellular pathogen transmitted by respiratory droplets expectorated during coughing which then adheres to the respiratory epithelium by means of a specialized attachment structure that forms at one end of the cell.
- M. pneumoniae possesses a membrane-associated protein, P1, which functions as a cytoadhesin.
- The adhesions interact specifically with sialated glycoprotein receptors at the base of cilia on the epithelial cell surface (and on the surface of erythrocytes).
- The organisms grow closely attached to the host cell luminal surface and inhibit ciliary action.
- Ciliostasis then occurs, after which cilia and ciliated epithelial cells, are destroyed.
- The loss of these cells interferes with the normal clearance of the upper airways and permits the lower respiratory tract to become contaminated with microbes and mechanically irritated.
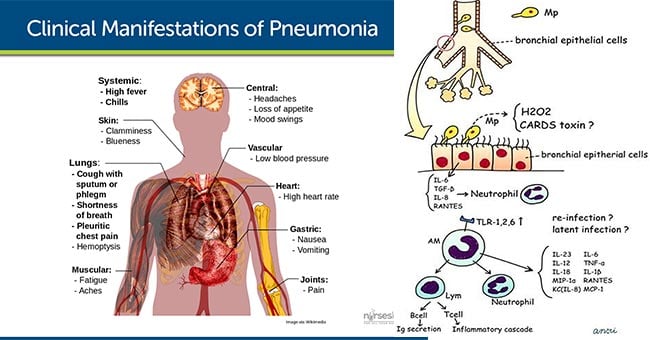
- M. pneumoniae also produces an exotoxin called as community-acquired respiratory distress syndrome (CARDS) toxin which exhibit similarities to pertussis toxin.
- This toxin functions as an ADP-ribosylating and vacuolating toxin and appears to play a role in damaging the respiratory epithelium and disrupting ciliary activity.
- The CARDS toxin and other mycoplasmal components may also elicit cellular toxicity by induction of cytokines and other inflammatory mediators.
- M. pneumoniae functions as a superantigen, stimulating inflammatory cells to migrate to the site of infection and release cytokines, initially tumor necrosis factor-α and interleukin-1 (IL-1) and later, IL-6.
- This process contributes to both the clearance of the bacteria and the observed disease.
- In infected individuals, organisms are shed in saliva for several days before onset of clinical illness.
- Reinfection is common, and symptoms are more severe in older children and young adults who have previously encountered the organism.
- An IgM antibody produce during infection in response to glycolipid antigen present in cell membrane binds to red blood cells and, at reduced temperatures, causes them to agglutinate. The antibody is called a cold hemagglutinin, which is detectable in about 50% of severe Mycoplasma infections.
- The reason M. pneumoniae infection stimulates the production of cold hemagglutinins is likely linked to a combination of molecular mimicry and shared antigens between Mycoplasma and mammalian proteins and autoimmunity.
- The clinical manifestations of M. pneumoniae infections are generally limited to the respiratory tract, but other organs are occasionally involved.
- Extrapulmonary complications of M. pneumonia infections include encephalitis and other pathologies of the central nervous system.
- Some patients develop a rash known as erythema multiforme, renal and cardiac disorders, or arthritis.
- These manifestations that sometimes occur in M. pneumoniae infections may result from direct spread of the organisms and the CARDS toxin from the respiratory tract to other parts of the body, or systemic host inflammatory and immune reactions that occur in response to the infectious process.
Clinical Manifestations of Mycoplasma pneumoniae
A. Upper respiratory tract infections
- It is usually mild and non-specific symptoms including runny nose, pharyngitis, coryza (symptoms of a head cold, stuffy or runny nose, cough, aches), and cough; most without fever.
B. Lower respiratory tract infections
- It is also called as atypical pneumonia which is best known form of M. pneumoniae infection.
- Atypical pneumonia clinically resembles pneumonia caused by a number of viruses and bacterial species.
- The incubation period averages 3 weeks.
- Onset is usually gradual, beginning with nonspecific symptoms such as mild illness with nonproductive cough, fever, malaise, pharyngitis, myalgias.
- After 2 to 4 days, a dry or scanty productive cough develops.
- Approximately 33% of patients develop pneumonia.
- Patients often remain ambulatory throughout the illness hence called as “walking pneumonia”.
- It is characterized by wheeze or rates, dry cough and peribronchial pneumonia with thickened bronchial markings and streaks of interstitial infiltration on chest X-ray.
C. Extra pulmonary manifestations
- They are rare, occur either as a result of active Mycoplasma infection (e.g. septic arthritis) or due to post infectious autoimmune phenomena (e.g. Guillain-Barre syndrome).
- Various manifestations include:
- Meningoencephalitis, encephalitis, Guillain- Barre syndrome and aseptic meningitis.
- Skin rashes including erythema multiforme major (Stevens-Johnson syndrome).
- Myocarditis, pericarditis
- Reactive arthritis
- Hemolytic anemia and hypercoagulopathy.
