Interesting Science Videos
Pathogenesis of Mycobacterium leprae
- M. leprae is an acid-fast, gram-positive obligate intracellular bacillus that shows tropism for cells of the reticuloendothelial system and peripheral nervous system (notably Schwann cells).
- Organisms may be acquired by the susceptible host usually through respiratory system or by way of skin to skin contact (between exudates of a leprosy patient’s skin lesions and the abraded skin of another individual).
- It has low pathogenecity, only a small proportion of infected people develop signs of the disease with incubation period varying from 6 months to 40 years or longer.
- After entering the body, bacilli migrate towards the neural tissue and enter the Schwann cells.
- Toll-like receptors (TLRs) also play important role in the pathogenesis of leprosy.
- TLRs, such as TLR-1 and TLR-2, are found on the surface of Schwann cells, especially in patients with tuberculoid leprosy.
- M. leprae activates this receptor on Schwann cells, which is suggested to be responsible for the activation of apoptosis genes and which enhances the onset of nerve damage seen in the mild disease.
- Bacteria can also be found in, macrophages, muscle cells and endothelial cells of blood vessels.
- After entering the Schwann cells /macrophage; fate of the bacterium depends on the resistance of the infected individual towards the infecting organism.
- Bacilli start multiplying slowly (about 12-14 days for one bacterium to divide into two) within the cells, get liberated from the destroyed cells and enter other unaffected cells.
- Till this stage person remains free from signs and symptoms of leprosy.
- As the bacilli multiply, bacterial load increases in the body and infection is recognized by the immunological system.
- Lymphocytes and histiocytes (macrophages) invade the infected tissue.
- At this stage clinical manifestation may appear as involvement of nerves with impairment of sensation and/ or skin patch.
- If it is not diagnosed and treated in the early stages, further progress of the diseases is determined by the strength of the patient’s immune response.
- Specific and effective cell mediated immunity (CMI) provides protection to a person against leprosy.
- When specific CMI is effective in eliminating/controlling the infection in the body, lesions heal spontaneously or it produces pauci-bacillary (PB) type of leprosy.
- If CMI is deficient; the disease spreads uncontrolled and produces multi bacillary (MB) leprosy with multiple system involvement.
- Blood stream may be invaded, with resulting foci in the liver, spleen, adrenals, testicles and bone marrow and excretion in the milk.
- Lepromatous leprosy (multibacillary leprosy) is more infectious than other types and have poor prognosis.
- In all forms of leprosy, M. leprae invade both sensory and motor nerves and destroy nerve fibers.
- Sometimes, the immune response is abruptly altered, either following treatment or due to improvement of immunological status, which results in the inflammation of skin and/ or nerves and even others tissue, called as leprosy reaction.
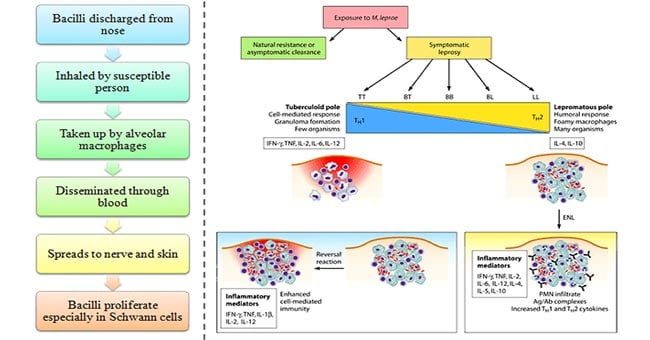
- Though leprosy runs as a chronic disease, several allergic type of acute exacerbations occur throughout its course, called leprae reactions which are of two types:
- Lepra reaction Type 1
- It is also called as reversal reaction and occurs in borderline cases (BT, BB, BL) who develop cell mediated immunity and consequently shifts towards tuberculoid part of spectrum.
- Clinically there is erythema and swelling of the skin lesions which may undergo ulceration.
- There is a predominant THl response with increased levels of IFN-γ and IL-2.
- Lepra Reaction Type-2
- It is developed mostly in lepromatous patients (LL or BL),undergoing chemotherapy.
- The most common feature is crops of painful erythematous papules, which become nodular termed as Erythema Nodosum Leprosum (ENL).
- Relapse is common and recurrent cases are more severe.
- There is a predominant TH2 response with increased levels of IL-6 and IL-8.
- Tumor necrosis factor-α (TNF-α) plays a central role in the immunology of ENL.
Clinical Manifestations of Leprosy caused by Mycobacterium leprae
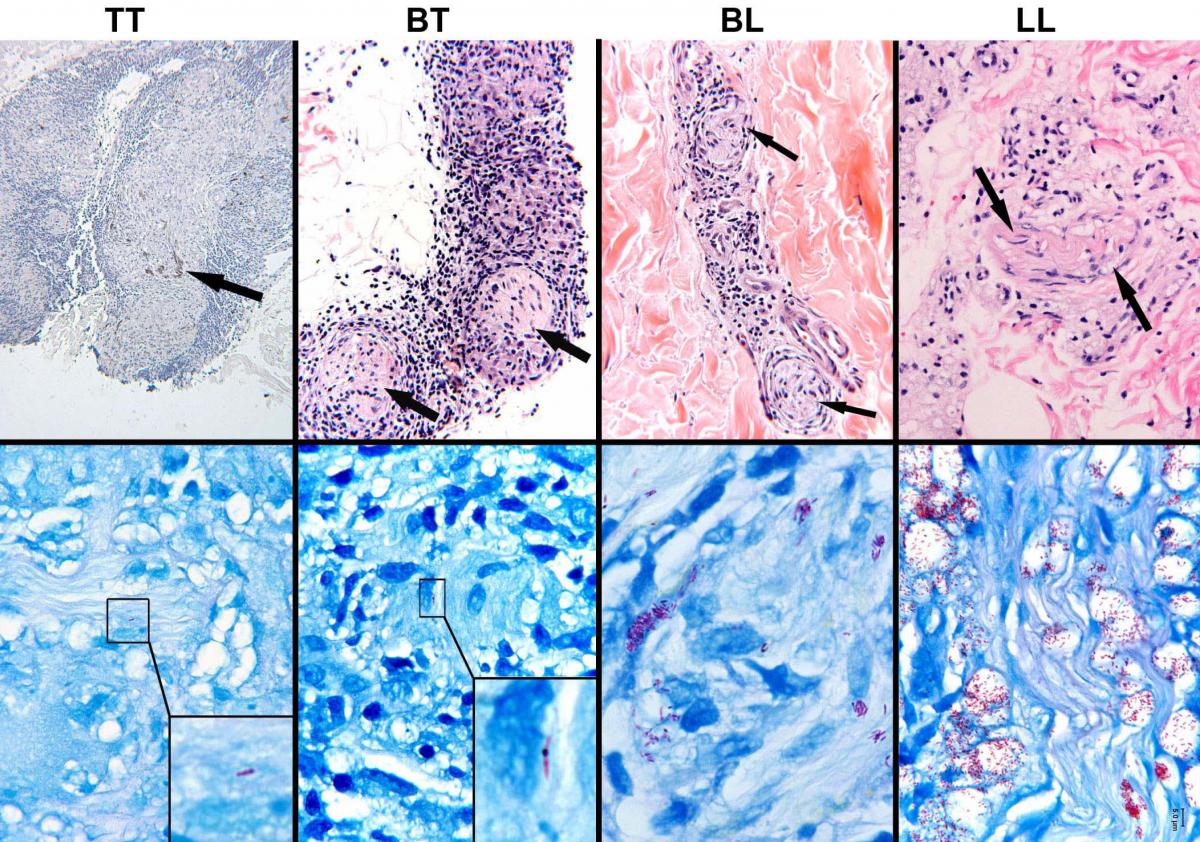
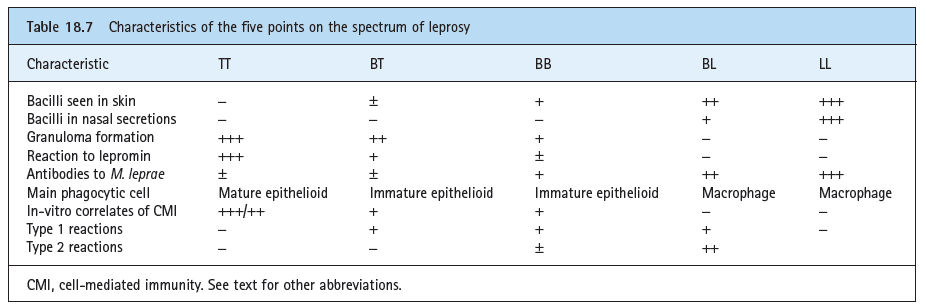
A. Tuberculoid leprosy
- The course is benign and non progressive, with a small number of macular skin lesions containing few bacilli (especially the nose, outer ears, and testicles), and in superficial nerve endings.
- These are usually circular, or serpiginous, sharply demarcated and often hypopigmented (patch lighter in colour compared to surrounding skin).
- These lesions may have raised and erythematous border with a dry scaly appearance in the center with complete anesthesia.
- The skin lesions are commonly found on the face, limbs, buttocks, or elsewhere but are not found in the axilla, perineum, or scalp.
- Neuritis leads to patches of anesthesia in the skin.
- The organisms grow and cause thickening in nerve sheaths.
- These thickened nerves can be felt through the skin, a characteristic of leprosy.
- The ulnar, peroneal, and greater auricular nerves are involved, leading to tender, thickened nerves with subsequent loss of function.
- Damage of the nerve can result in wrist drop or foot drop.
- The lesions are heavily infiltrated by lymphocytes and giant and epithelioid cells, but caseation does not occur.
- The patient mounts a strong cell-mediated immune response and develops delayed hypersensitivity, which can be shown by a skin test with lepromin, a tuberculin-like extract of lepromatous tissue.
- There are few bacteria in the lesions also called as paucibacillary.
- Patients with tuberculoid leprosy (also called paucibacillary Hansen disease) have a strong cellular immune reaction with many lymphocytes and granulomas present in the tissues and relatively few bacteria.
B. Borderline tuberculoid leprosy
- Lesions in this form of leprosy are similar to those seen in the tuberculoid leprosy, but are smaller and more numerous.
- Skin lesions are few, asymmetric, and with nearly complete anesthesia.
- Peripheral nerves are thickened and involved asymmetrically.
- This form of leprosy may remain at this stage or can regress to the tuberculoid form; or it can progress to lepromatous form.
C. Mid-borderline leprosy
- Skin lesions in this type of leprosy consist of numerous unequally shaped plaques that are less well defined than in the tuberculoid types.
- These skin lesions are distributed asymmetrically.
- Anesthesia is moderate, and the disease can remain in this stage, can improve, or worsen to more disseminated form.
D. Borderline lepromatous leprosy
- Skin lesions are moderate to numerous.
- They are slightly asymmetrical with slight or no anesthesia.
- Peripheral nerves are enlarged moderately and symmetrical.
- Like the other forms of borderline leprosy, the disease may remain in this stage, improve, or lead to lepromatous form.
E. Lepromatous leprosy
- The lepromatous leprosy is characterized by the presence of large number of acid fast bacilli in large clumps (globi) inside the macrophages (lepra cells).
- The skin lesions include macules, nodules, plaques, or papules.
- The skin lesions are extensive and are bilaterally symmetrical.
- They are most severe at the cooler parts of the body.
- This form of disease is associated with disfigurative lesions.
- The skin of the face and forehead becomes thickened and corrugated, giving rise to typical leonine face.
- The lateral part of the eyebrows may be lost.
- Other disfiguring lesions include pendulous ear lobes, hoarseness of voice, involvement of cornea, perforation of the nasal septum, and nasal collapse.
- Painless inguinal and axillary adenopathy, scarring of testis leading to sterility and gynecomastia are other complications.
- Diffuse hyperanesthesia involving peripheral parts of extremities also occur due to involvement of the neural tissue.
- Patients with lepromatous leprosy are anergic to leprae because of a defect in their cell-mediated immunity.

please provide reference for pathogenesis explained above
Hi Sagar Aryal,
My name is Moisés Santos.
I am a biomedicine student in Brazil, in Rio de Janeiro through the university IBMR – Brazilian Institute of Rehabilitation Medicine.
In the second semester I will have to do a paper on leprosy and I would like to thank you first for your blog, it will be part of the bibliography of my work and it will be an inspiration for us undergraduates.
I have a question about the image below the title: Clinical Manifestations of Leprosy caused by Mycobacterium leprae.
There are different titles, such as: TT, BT, BL and LL, what would be the meaning of these letters?
Thank you in advance and congratulations again for your work.
Att.
Moisés Santos
Borderline leprosy includes borderline tuberculoid (BT), borderline borderline (BB), and borderline lepromatous (BL) leprosy