Interesting Science Videos
Pathogenesis of Francisella tularensis
- Francisella tularensis is carried by many species of wild rodents, rabbits, beavers.
- Humans become infected by handling the carcasses or skin of infected animals, by inhaling infective aerosols or ingesting contaminated water, through insect vectors and by being bitten by carnivores that have themselves eaten infected animals.
- Humans are infected by fewer than 50 organisms by either aerosol or cutaneous routes.
- F. tularensis subsp. tularensis is the most virulent for humans, with an infectious dose of less than 10 colony forming units.
- The pathogens invade the host either through microtrauma in the skin or through the mucosa.
- An ulcerous lesion develops at the portal of entry that also affects the local lymph nodes (ulceroglandular, glandular, or oculoglandular form).
- Through lymphogenous and hematogenous dissemination, the pathogens then spread to parenchymatous organs, in particular reticuloendothelial system (RES) such as the spleen and liver.
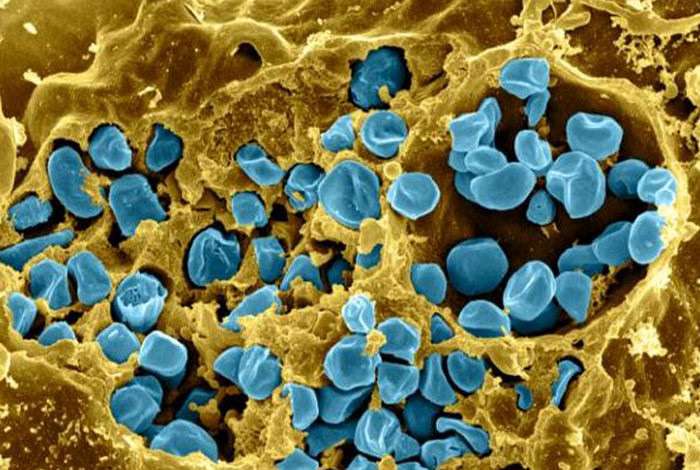
- F. tularensis is an intracellular pathogen that can survive in the cells of the reticuloendothelial system, where it resides after a bacteremic phase because the organism inhibits phagosome–lysosome fusion through secretion of proteins that facilitate bacterial escape from the phagosome and subsequent replication in the macrophage cytosol.
- The polysaccharide rich capsule of F. tularensis is a necessary component for expression of full virulence, allowing the organism to avoid immediate destruction by polymorphonuclear neutrophils and is antiphagocytic in nature.
- The capsule protects the bacteria from complement-mediated killing during the bacteremia phase of disease.
- The bacterium also produces endotoxin which is less active as compared to endotoxin produced by other Gram negative bacteria.
- A strong, innate immune response with production of interferon-γ and tumor necrosis factor (TNF) is important for controlling bacterial replication in macrophages in the early phase of infection.
- Specific T-cell immunity is required for activation of macrophages for intracellular killing in the late stages of disease. However, humoral immunity is less important for elimination of facultative intracellular pathogen.
Clinical manifestations of Francisella tularensis
- The disease associated with F. tularensis, is known as Tularemia.
- The clinical manifestation depends on the mode of transmission, the virulence of the infecting organism, the immune status of the host, and the length of time from infection to diagnosis and treatment.
- Disease caused by F. tularensis is subdivided into several forms based on the clinical presentation given as:
1. Ulceroglandular tularemia
- Ulceroglandular tularemia is the most common manifestation.
- The skin lesion, which starts as a painful papule at the site of the tick bite or direct inoculation of the organism into the skin.
- The papule then ulcerates and has a necrotic center and raised border.
- Localized lymphadenopathy and bacteremia are also typically present.
2. Glandular tularemia
- It involves primarily swollen lymph nodes with no other localized symptoms
3. Oculoglandular tularemia
- Oculoglandular tularemia is a specialized form of the disease and results from direct contamination of the eye.
- .The organism can be introduced into the eyes, for example, by contaminated fingers or through exposure to water or aerosols.
- Affected patients have a painful conjunctivitis and regional lymphadenopathy (swollen cervical lymph nodes).
4. Pneumonic tularemia
- Pneumonic tularemia results from inhalation of infectious aerosols and is associated with high morbidity and mortality.
- Patients present with atypical pneumonia and typically has systemic signs of sepsis.
5. Oropharyngeal tularemia
- It occurs following ingestion of contaminated undercooked meat.
- It is characterized by membranous pharyngitis with cervical lymphadenopathy
6. Typhoidal tularemia
- The clinical manifestations include acute illness with septicemia.
- The mortality rate is 30% to 60%.
- There is no ulcer or lymphadenopathy.
7. Gastrointestinal disease
- It occurs upon ingestion of F. tularensis and is not very common clinical form.
