Interesting Science Videos
Pathogenesis of Coxiella burnetii
- Human infection usually follows inhalation of aerosols containing C. burnetii.
- It is estimated that only between 1 and 10 bacteria are necessary to cause infection.
- C. burnetii has also been known to enter the body via other mucous membranes, abrasions, and the gastrointestinal tract through consumption of milk from infected animals.
- C. burnetii exists in two antigenic forms called phase I and phase II.
- Phase I is the virulent form that is found in humans with Q fever and infected vertebrate animals, and it is the infectious form, whereas Phase II is the avirulent form.
- Entry into the lungs results in infection of the alveolar macrophages.
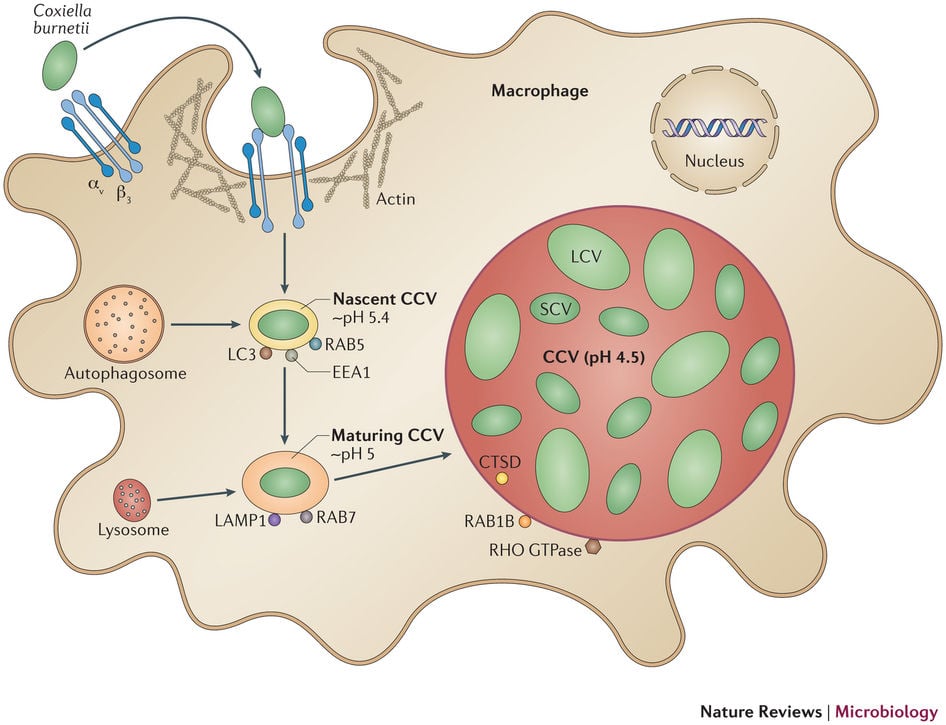
- C. burnetii escapes intracellular killing in macrophages by:
- Inhibiting the final phagosome maturation step (cathepsin fusion)
- Resistant to the acidic environment of phagolysosome by producing superoxide dismutase.
- The normal progression after phagocytosis of most organisms is fusion of the phagosome with a series of endosomes (intracellular vesicles), resulting in a drop in intracellular pH, followed by fusion with lysosomes containing hydrolytic enzymes and resultant bacterial death which occurs with C. burnetii if phase II organisms are ingested; however, phase I Coxiella is able to arrest this process before lysosomal fusion.
- In addition, the organisms require acid pH for their metabolic activities, which, in turn, protects them from the killing activities of most antibiotics.
- Coxiella is able to regulate the cell signaling pathways in its phagocytic home so that cell death is delayed.
- The ability of C. burnetii to cause either acute or chronic disease is determined in part by the organism’s ability to survive intracellularly.
- In acute cases, in the presence of interferon-γ, phagosome–lysosome fusion occurs, leading to bacterial death; however, in chronic infections interleukin-10 is overproduced by the host cell, which interferes with fusion and allows intracellular survival of C. burnetii.
- Infection with C. bumetii induces autoantibodies, particularly to cardiac and smooth muscles.
- Chronic form leads to disseminated cases affecting various organs with pathological condition.
Clinical Manifestations of Coxiella burnetii
Query fever (Q fever)
- The majority of individuals exposed to C. burnetii have an asymptomatic infection, and most symptomatic infections are mild, presenting with nonspecific flulike symptoms with an abrupt onset, high-grade fever, fatigue, headache, and myalgias.
- The patient may also suffer pneumonitis, hepatic and bone marrow granulomata, and meningoencephalitis.
- Hepatitis is usually asymptomatic or presents with fever and increase in serum transaminases.
- Most cases of pneumonia are mild, with a nonproductive cough, fever, and nonspecific findings on chest radiograph.
- Acute pneumonia and hepatitis are associated with antibodies to phase II antigens.
- Chronic infections can develop, with the organism persisting in cardiac valves and possibly other foci.
- Chronic Q fever (symptoms lasting more than 6 months) can develop months to years after the initial exposure and occurs almost exclusively in patients with predisposing conditions, such as underlying valvular heart disease or immunosuppression.
- Fever is usually absent or of low grade.
- Reactivation of latent infection may occur during pregnancy, and the organism is shed with the placenta or abortus.
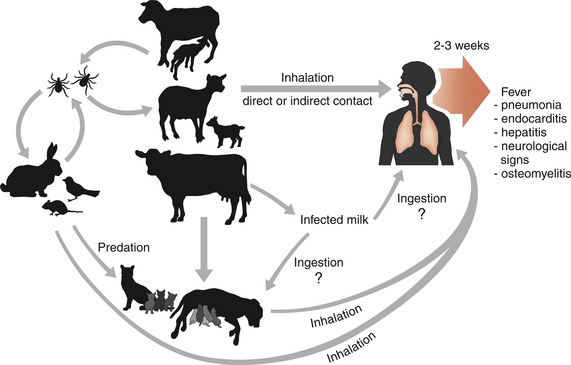

What is the pathogenesis in different animal species?