Interesting Science Videos
Virulence factors or antigenic structures of Neisseria gonorrhoeae
A. Pili
- Pili are the hair like appendages that extend up to several micrometers from the gonococcal surface.
- It mediates the exchange of genetic material between strains and attachment to human mucosal cell surface, invasion of host cells, and survival through the inhibition of phagocytosis.
- Two types: types T1-T2 virulent and T3-T5 avirulent
- Genetic-phase variation of pilus structure between types T1 through T5 allows the organism to vary its antigenic structure, preventing recognition by host immune cells.
B. Porin proteins (por proteins)
- Por protein extends through the gonococcal cell membrane.
- It forms pores in the surface through which some nutrients enter the cell.
- Por proteins may impact intracellular killing of gonococci within neutrophils by preventing phagosome– lysosome fusion.
- In addition, variable resistance of gonococci to killing by normal human serum depends on whether Por protein selectively binds to complement components C3b and C4b.
C. Opacity proteins (opa proteins)
- These proteins function in adhesion of gonococci within colonies and in attachment of gonococci to host cell receptors such as heparin-related compounds and CD66 or carcinoembryonic antigen–related cell adhesion molecules.
D. Reduction modifiable protein (rmp protein)
- It is antigenically conserved in all gonococci.
- It associateswith Por in the formation of pores in the cell surface.
- It blocks the bactericidal effect of host IgG.
E. Lipooligosaccharide
- Gonococcal lipopolysaccharide (LPS) does not have long O-antigen side chains and is called a lipooligosaccharide(LOS).
- Toxicity in gonococcal infections is largely attributable to the endotoxic effects of LOS.
- Capsule, lipooligosaccharide (endotoxin), and outer cell membrane proteins I-III are important in antigenic variation and for eliciting an inflammatory response.
F. Other proteins
- Lip (H8) is a surface exposed protein that is heat modifiable like Opa.
- The Fbp (ferric-binding protein), similar in molecular weight to Por, is expressed when the available iron supply is limited, such as in human infection.
- Gonococci elaborate an IgA1 protease that splits and inactivates IgA1, a major mucosal immunoglobulin of humans.
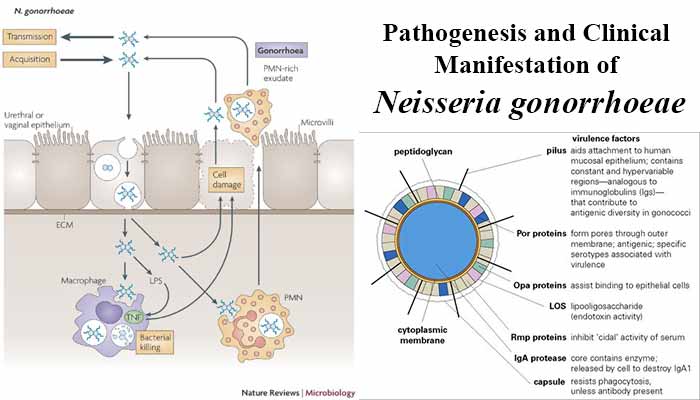
Pathogenesis of Neisseria gonorrhoeae
- Gonorrhoeal infection is generally limited to superficial mucosal surfaces lined with columnar epithelium.
- Pili and Opa proteins facilitate adhesion of the gonococcus to epithelial cells of the urethra, rectum, cervix, pharynx, and conjunctiva, thereby making colonization possible.
- Pili, PorB, and Opa proteins mediate gonococci to attach to mucosal cells, penetrate into the cells and multiply, and then pass through the cells into the subepithelial space where infection is established.
- The gonococcal LOS stimulates release of the proinflammatory cytokine tumor necrosis factor-α (TNF-α), which causes most of the symptoms associated with gonococcal disease.
- Antibodies to LOS can activate complement, releasing complement component C5a, which has a chemotactic effect on neutrophils; however, IgG and secretory IgA1 antibodies directed against Rmp protein can block this bactericidal antibody response.
- The gonococcus requires iron for growth and survival in vivo.
- The pathogen acquires this necessary nutrient by expression of specific transport systems that remove and internalize the iron from human iron binding proteins including transferrin, lactoferrin and hemoglobin.
Clinical manifestations of Neisseria gonorrhoeae
Gonococci most often colonize the mucous membrane of the genito -urinary tract or rectum. There, the organisms may cause a localized infection with the production of pus or may lead to tissue invasion, chronic inflammation, and fibrosis. A higher proportion of females than males are generally asymptomatic, and these individuals act as the reservoir for maintaining and transmitting gonococcal infections.
A. Genitourinary tract infections
- Acute infections in males
- In males, yellow, purulent urethral discharge and painful urination
- In females, infection occurs in the endocervix and extends to the urethra and vagina. A greenish-yellow cervical discharge is most common, often accompanied by intermenstrual bleeding.
- Genital infections include acute purulent urethritis, prostatitis, and epididymitis in males and acute cervicitis in females.
- The disease may progress to the uterus, causing salpingitis (inflammation of the fallopian tubes), pelvic inflammatory disease (PID), and fibrosis.
- Pelvic inflammatory disease (PID) may cause sterility, ectopic pregnancy or perihepatitis also referred to as Fitz-Hugh–Curtis syndrome.
B. Rectal Infections
- Prevalent in men who have sex with men, rectal infections are characterized by constipation, painful defecation, and purulent discharge.
C. Pharyngitis
- Pharyngitis is contracted by oral-genital contact.
- Infected individuals may show a purulent pharyngeal exudates.
D. Ophthalmia neonatrum
- This infection of the conjunctival sac is acquired by newborns during passage through the birth canals of infected mothers.
- If untreated, acute conjunctivitis may lead to blindness.
E. Disseminated infection
- Most strains of gonococci have a limited ability to multiply in the bloodstream.
- Therefore, bacteremia with gonococci is rare.
- However, some strains of gonorrhoeae do invade the bloodstream and may result in a disseminated infection in which the organism can cause fever; a painful, purulent arthritis; and small, single, scattered pustules on the skin, whose base becomes erythematous due to dilation or congestion of capillaries.
- Necrosis may develop.
- Disseminated infections are seen in both men and women but are more common in women, particularly during pregnancy and menses.

I am really appreciate you description concerned above thank and please may wish you to give me more about several species pathogenesis
In Iraq GC in (1960 ) sensitive to p[penicillin than (1980 ) to ciprofloxacin ,In (1990) to cefotraxion < now seen resistance to cefotraxion