Interesting Science Videos
What is Listeriosis?
Listeriosis or listeria infection is the major cause of foodborne illness by a causative agent Listeria monocytogenes.
- After the consumption of contaminated food caused by the bacteria, mild fever or illness may appear but a systemic (invasive) listeriosis affects highly susceptible individuals such as immune-compromised patients, pregnant women, and old aged people.
- It causes sepsis and meningoencephalitis in animals as well as humans, especially pregnant women who suffer spontaneous abortion.
- Among the listeria species, L. monocytogenes is a human pathogen and L. ivanovii is pathogenic to animals.
- Other L. innocua, L. weishimeri, L. seeligeri, L. grayi are considered non-pathogenic.
- L. monocytogenes is a threat in the food production facilities as well causing a large number of food products at risk.
- Therefore, risk and quality control managers should focus constantly during the production process from raw materials to packaging and storage.
Source of contamination
- Listeria monocytogenes are gram-positive, non-sporing frequent veterinary pathogens widely spread in the environment (mostly in soil, water, sewage, and decaying plant matter) where they live as saprophytes.
- These bacteria can tolerate high salt concentration (10%), can survive in broad pH (4.1-9.6), and are psychrophiles (1-45°C).
- Food products that are at high risk of contamination are ready-to-eat foods such as hotdogs, smoked fish, raw seafood, sausages, pre-prepared or pre-packaged fruits, and vegetables, deli meats, unpasteurized milk, and milk products.
- These food products are the potential source of contamination and are responsible for numerous outbreaks.
Antigenic structure and virulence factors
- Listeria contains 13 known distinct serotypes of somatic (O) antigens and 5 serovars of flagellar (H) antigens.
- However, serotypes 1/2a, 1/2b, and 4b affect 98% of the human and animal outbreaks.
- L. monocytogenes is capable of surviving harsh environmental conditions like thermal variation, acidic pH, and the presence of antimicrobial agents.
- This leads to the formation of virulence genes called sigma factor B (sigB gene).
- Listeria can survive gastric pH and reach up to the intestinal cells via phagocytic vacuoles.
- The bacterial surface protein internalin (Inl) attaches to the host cells where it enters and promotes intracellular replication.
- The expression of virulence genes is controlled by regulatory genes.
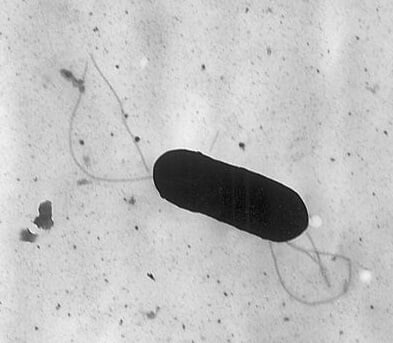
Figure: Electron micrograph of a flagellated Listeria monocytogenes bacterium, Magnified 41,250X. Image Source: Elizabeth White.
Epidemiology of Listeriosis
- The mortality rate of L. monocytogenes is high once it causes infection and newborn infants are at high risk.
- The first outbreak of listeriosis was reported in Canada by the consumption of cabbage that was contaminated by Listeria infected sheep manure.
- Pregnant women and immunocompromised patients were highly affected causing a large death rate in the United States and European countries.
- Every year in the United States, approximately 2500 serious illnesses and 500 deaths are reported by listeriosis.
- The most recent outbreak has occurred in South Africa in early 2017 which was due to the consumption of RTE meat products.
- The fatality rate of this outbreak was 27% with 1,060 confirmed cases and 216 deaths.
- Most of the outbreaks are associated with the production process therefore, risk assessment of the routes of contamination must be determined carefully.
Clinical signs and symptoms of Listeriosis
- Fetomaternal and neonatal listeriosis cause abortion or birth of the baby with granulomatosis infantiseptica which has a high mortality rate.
- Pyrogranulomatous microabscesses are also spread throughout the body.
- In a pregnant mother, symptoms are usually asymptomatic and if present may appear as the mild flu with headache, fever, chills, and muscle pain that lasts for one to two weeks.
- Neonatal listeriosis causes meningitis, gastroenteritis, and pneumonia in some cases.
- In adults, symptoms of listeriosis may appear as severe changes in consciousness, movement disorders, and paralysis of the brain.
- Common symptoms are headache, vomiting, malaise, visual disorders, rhombencephalitis.
- Other atypical clinical signs are endocarditis, myocarditis, arthritis, pneumonia, hepatitis, sinusitis, conjunctivitis, and mastitis in cattle.
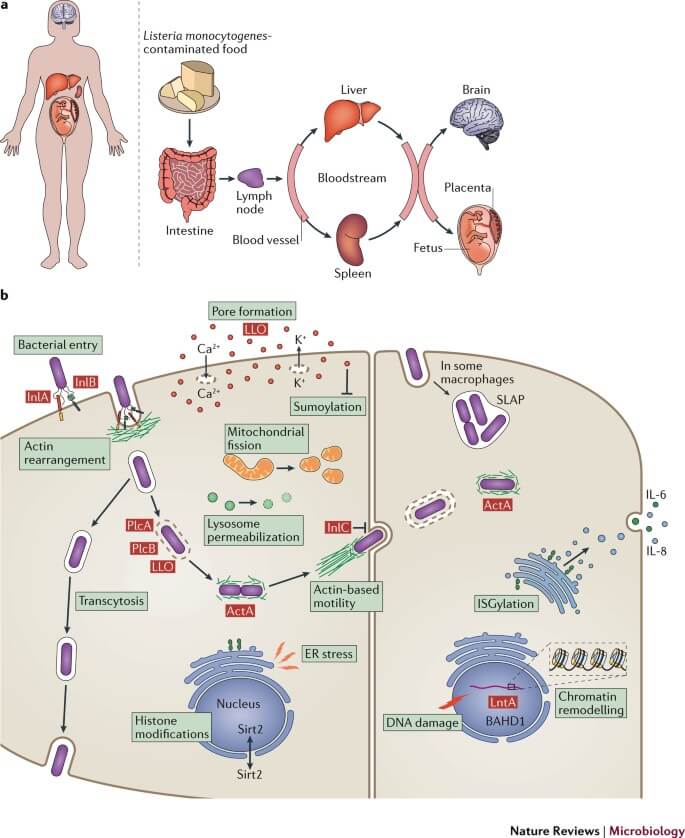
Figure: Overview of Listeria monocytogenes infection. Image Source: Nature Reviews Microbiology.
Mechanism of Pathogenesis
- From the information available from the epidemiological and clinical data, it is confirmed that the contaminated food is the major source when ingested and reaches the gastrointestinal tract and starts the primary entry of pathogens.
- In the case of gastroenteritis, the incubation period is about 20 hours after the consumption of heavily contaminated food.
- In systemic illness, the incubation period is much longer around 20 to 30 days.
- The dose required for the infection has not yet been determined but typically 105 to 106cfu/ml bacteria is detected in food that caused listeriosis.
- The pathogenicity and virulence of L. monocytogenes depend on the strain of the organism and host risk factors.
- The attachment of L. monocytogenes in the intestinal cell wall is mediated by the surface protein, InlA where it colonizes and translocates rapidly through the mucosal barrier to blood circulation and the lymphatic system.
- After the attachment of the bacteria to the intestinal tract, the glutamate decarboxylase(GAD) system protects the bacterium from stomach acid.
- Similarly, bile salt hydrolase (BSH) and the bile exclusion system (BilE) protect against bile salts then the bacterium enters through the mucosal layer and ruptures the intestinal epithelial barrier.
- Helper T-cells (CD4+) or cytotoxic T-cells (CD8+) transports bacteria to systemic sites such as the liver, spleen, lymph nodes, and the placenta of pregnant women.
- The organism gets trapped by a phagosome after the entry into the host cell but it escapes with the help of an enzyme listeriolysin O (LLO) and phospholipase.
- These enzymes form monomer units in the membrane with the formation of pores resulting in the lysis of cells and inducing apoptosis leading to disruption of the membrane, releasing intracellular enzymes, and degrading DNA.
- During infection, 90% of the organism infects the liver and 10% infects the spleen. Neutrophils, Kupffer cells, and macrophages control the infection in the liver as soon as the organism enters the infected hepatocytes.
- Polymorphonuclear neutrophils pile up at the site of infection and form discrete microabscesses.
- ActA Actin polymerization protein (ActA) aids the bacterial movement within the cytoplasm and spreads cell to cell causing systemic listeriosis.
- The bacterial colonization in the uterus results in abortion and premature childbirth which gets accessed by hematogenous penetration of the placental barrier.
- This causes placental infection characterized by numerous microabscesses focal necrotizing villitis which subsequently causes the death of the fetus.
Laboratory Diagnosis of Listeria monocytogenes
Serology testing
- Widal test, a classical agglutination reaction gives a result based on O and H antigens.
- Listeriolysin O (LLO) antibodies are also used for the diagnosis of human listeriosis which is serially diluted after being incorporated into nitrocellulose fibers.
- The absorbed anti-LLO is determined by an enzyme-labeled anti-human IgG.
- This test has 90% sensitivity and specificity but this technique is not commercially available.

Organism cultivation
- For the identification, L. monocytogenes is cultured on venous blood, urine, placenta, amniotic fluid, and biopsy tissues.
- Gram staining is also performed on sterile specimens such as cerebrospinal fluid and tissue smears.
- Mostly Listeria is mistaken for pneumococci and corynebacterium during diagnosis.
Molecular detection
- PCR-based methods are widely used for the detection of organisms being rapid and sensitive.
- Clinical samples such as cerebrospinal fluid and for screening of food, 16S ribosomal RNA gene sequence of Listeria are used in amplification.
Treatment Listeriosis
- If the symptom of the infection is minor, medication is not required but if the case is serious, antibiotic therapy must be taken at an earlier stage.
- Ampicillin, amoxicillin, penicillin G, and gentamicin are the choices of antibiotics.
- If an individual suffers from meningitis or septicemia, intravenous antibiotics must be given with proper care and treatment for at least 6 weeks.
- Fluid therapy must be taken in case of gastroenteritis to balance electrolytes in the body.
Prevention and Control Listeriosis
- Proper heat treatment or pasteurization of processed foods before consumption.
- Thorough cooking of refrigerated meat and kinds of seafood before consumption.
- Cleanliness in a farm, animal feed, silage, and in the processing plant to prevent the infection.
- Implementation of sanitation in the processing plant and routine surveillance of the production facilities.
- Pregnant women and susceptible people should avoid salads, meats, and soft cheeses from deli counters.
References
- Bortolussi, R., & Mailman, T. L. (2010). Listeriosis. Infectious Diseases of the Fetus and Newborn, 470–488.
- Vazquez-Boland, J. A., Kuhn, M., Berche, P., Chakraborty, T., Dominguez-Bernal, G., Goebel, W., … Kreft, J. (2001). Listeria Pathogenesis and Molecular Virulence Determinants. Clinical Microbiology Reviews, 14(3), 584–640.
- Buchanan, R. L., Gorris, L. G. M., Hayman, M. M., Jackson, T. C., & Whiting, R. C. (2017). A review of Listeria monocytogenes : An update on outbreaks, virulence, dose-response, ecology, and risk assessments. Food Control, 75, 1–13.
- https://www.researchgate.net/publication/226125437_Listeria_monocytogenes_and_the_Genus_Listeria- 16%
- https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/sheep-manure- 2%
- https://onlinelibrary.wiley.com/doi/full/10.1111/apm.12847- 1%
- https://microbenotes.com/biochemical-test-of-listeria-monocytogenes- <1%
