Interesting Science Videos
Laboratory diagnosis of Streptococcus pneumoniae
Specimen: Sputum, blood, endotracheal aspirate, bronchoalveolar lavage, cerebrospinal fluid (CSF), pleural fluid, joint fluid, abscess fluid, bones, and other biopsy material.
Microscopy
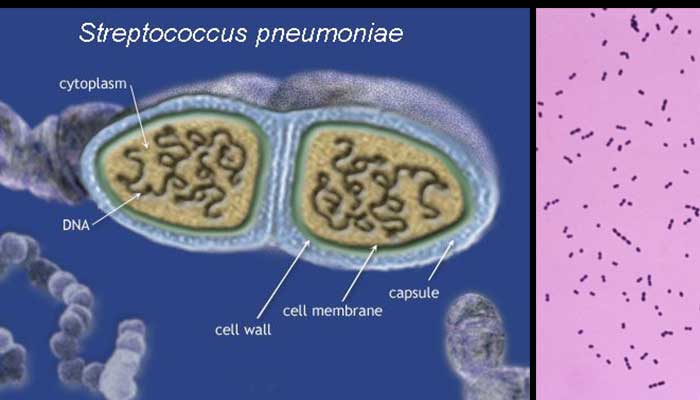
- Gram staining of sputum shows lancet shaped Gram-positive cocci in pairs.
- Fresh emulsified sputum mixed with antiserum causes capsule swelling (the quellung reaction) for identification of pneumococci.
- In acute pneumococcal otitis media, Gram stain of an aspirated fluid smear from middle ear is useful to demonstrate the bacteria.
Culture
- Sputum or blood is plated on blood agar and incubated at 37° C in the presence of 5–10% carbon dioxide.
- Gray colonies with alpha-hemolysis are observed after overnight incubation.
- Diagnosis of pneumococcal meningitis is confirmed by CSF culture.
Identification of bacteria
- Optochin sensitivity test
- S. pneumoniae is identified by its sensitivity to optochin (ethylhydrocupreine dihydrochloride).
- The isolate is streaked onto a blood agar plate and a disk saturated with optochin is placed in the middle of the inoculum.
- A zone of inhibited bacterial growth is seen around the disk after overnight incubation.
- Bile solubility test
- It detects an autolytic enzyme, amidase, present in pneumococci, which breaks the bond between alanine and muramic acid of the peptidoglycan of the pneumococcal cell wall.
- Isolates of S. pneumoniae are lysed rapidly when the autolysins are activated after exposure to bile.
- Thus the organism can be identified by placing a drop of bile on an isolated colony.
- Inulin fermentation test
- It ferments inulin and hence differentiate it from other streptococci.
Animal inoculation
- S. pneumoniae can be isolated from clinical specimens containing few pneumococci by intraperitoneal inoculation in mice.
- Pneumococci are demonstrated in the peritoneal exudate and heart blood of the mice, which die 1–3 days after inoculation.
Antigen detection
- Pneumococcal C polysaccharide is excreted in urine and can be detected using a commercially prepared immunoassay.
- The CIEP is a useful test to detect pneumococcal capsular polysaccharide antigen in the CSF for diagnosis of meningitis, and in the blood or urine for diagnosis of bacteremia and pneumonia.
- Latex agglutination test using the latex particles coated with anti-CRP antibody is employed to detect C reactive protein.
- The CRP is used as a prognostic marker in acute cases of acute pneumococcal pneumonia, acute rheumatic fever, and other infectious diseases.
Antibody detection
- The indirect hemagglutination, indirect fluorescent antibody test, and ELISA are used to demonstrate specific pneumococcal antibodies in invasive pneumococcal diseases.
Nucleic Acid–Based Tests
- Nucleic acid probes and PCR assays are used for identification of S. pneumoniae isolates in culture.
Treatment of Streptococcus pneumoniae
- Most pneumococci are susceptible to penicillin.
- Other antibiotics, such as macrolides or selected fluoroquinolones with activity against pneumococci, are available for patients who are allergic to penicillin.
- Penicillin-resistant pneumococci are being increasingly documented.
- The mechanism of this resistance is an alteration of one or more of the bacterium’s penicillin-binding proteins (PBPs) rather than production of beta-lactamase.
- Most resistant strains remain sensitive to third generation cephalosporins (such as cefotaxime or ceftriaxone), and all are still sensitive to vancomycin.
- For serious pneumococcal infections, treatment with a combination of antibiotics is recommended. Vancomycin combined with ceftriazone is used commonly for empiric treatment, followed by monotherapy with an effective cephalosporin, fluoroquinolone or vancomycin.
- Ceftriaxone can be used for meningitis caused by ceftriaxone-susceptible pneumococci.
- Amoxicillin is the drug of choice for treatment of otitis media, sinusitis, and pneumonia caused by penicillin-resistant pneumococci with intermediate resistance.
- Ceftriaxone is the drug of choice for non-CNS invasive pneumococcal diseases caused by penicillin- and ceftriaxone resistant pneumococci.
- Vancomycin is used if the pneumococcus is resistant to ceftriaxone.
Prevention and control of Streptococcus pneumoniae
- Pneumococcal vaccines: 23 valent pneumococcal polysaccharide vaccine (PPSV23) and polyvalent pneumococcal conjugate vaccine (PCV13) play an important role in prevention of pneumococcal diseases.
- Personal hygiene is another important factor.

will that be enough for 10 marks in TU exam
Micriobiology has always been my passion. Aiming to advance inmicriobiology research.