Interesting Science Videos
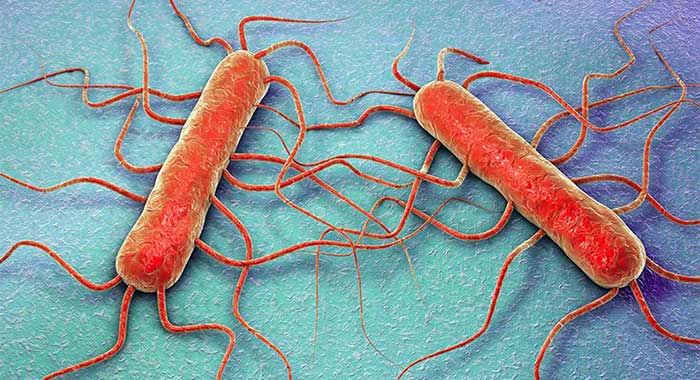
Laboratory diagnosis of Listeriosis caused by Listeria monocytogenes
Specimens: Cerebrospinal fluid (CSF), Blood
Microscopy
- Gram-stain preparations of cerebrospinal fluid (CSF) typically show no organisms because the bacteria are generally present in concentrations below the limit of detection (e.g., 10ˆ4 bacteria per milliliter CSF or less).
- If the Gram stain shows organisms, they are intracellular and extracellular gram-positive coccobacilli.
Culture of Listeria monocytogenes
- Listeria grows on most conventional laboratory media, with small, round colonies observed on agar media after incubation for 1 to 2 days.
- It may be necessary to use selective media and cold enrichment (storage of the specimen in the refrigerator for a prolonged period) to detect listeriae in specimens contaminated with rapidly growing bacteria.
- Listeria grows well on media such as 5% sheep blood agar on which it exhibits the characteristic small zone of hemolysis around and under colonies.
- β-Hemolysis on sheep blood agar media can serve to distinguish Listeria from morphologically similar bacteria; however, hemolysis is generally weak and may not be observed initially.
- Hemolysis is enhanced when the organisms are grown next to β-hemolytic Staphylococcus aureus.
- This enhanced hemolysis is referred to as a positive CAMP (Christie, Atkins, Munch-Petersen) test.
- The characteristic motility of the organism in a liquid medium or semisolid agar is also helpful for the preliminary identification of Listeria.
- All gram-positive rods isolated from blood and CSF should be identified to distinguish between Corynebacterium (presumably a contaminant) and Listeria.
Biochemical Test of Listeria monocytogenes
Catalase: positive
Oxidase: negative
Indole: negative
Methyl Red: positive
Voges Proskauer: positive
Citrate: negative
Urease: negative
Carbohydrate fermentation of Listeria monocytogenes
D- Mannitol: negative
L- Rhamnose: positive
D- Xylose: negative
CAMP test: positive
Motility: tumbling
Arylesterase activity: negative
Serology and molecular methods
- Serologic and molecular typing methods are used for epidemiologic investigations.
- Serologic classification is done only in reference laboratories and is primarily used for epidemiologic studies.
- There are 13 known serovars based on O (somatic) and H (flagellar) antigens.
- Serotypes 1/2a, 1/2b, and 4b make up more than 95% of the isolates from humans and are responsible for most infections in neonates and adults.
- Serotype 4b causes most of the food borne outbreaks.
- Pulsed-field gel electrophoresis (PFGE) is the most commonly used molecular method for epidemiologic investigations of suspected outbreaks.
Treatment of Listeriosis
- Most antibiotics are only bacteriostatic with L. monocytogenes, hence the combination of gentamicin with either penicillin or ampicillin is the treatment of choice for serious infections.
- Listeriae are naturally resistant to cephalosporins, and resistance to macrolides, fluoroquinolones, and tetracyclines has been observed, which can limit the utility of these drugs.
- Trimethoprim-sulfamethoxazole is bactericidal to L. monocytogenes and has been used successfully.
Prevention and control of Listeriosis
- Listeriae are ubiquitous and most infections are sporadic. Hence, prevention and control are difficult.
- People at high risk of infection should avoid eating raw or partially cooked foods of animal origin, soft cheeses, and unwashed raw vegetables.
- A vaccine is not available, and prophylactic antibiotic therapy for high-risk patients has not been evaluated.
