As much as immunity curtails to the 430 B.C, significantly improved immunity phenomenal were made in the 18th century starting with Edward Jenner in 1798 after he noticed that milkmaids that had contracted the mild disease of cowpox, were immune to smallpox (a fatally deadly disease).
He practically inoculated cowpox pustules into an 8-year-old boy and intentionally infected him with smallpox. As he had predicted, the child did not develop smallpox. His work was subsequently followed by Pastuer’s work who developed vaccines for chicken cholera, anthrax, and rabies.
Interesting Science Videos
Mechanism of Immunity
- To understand the immunity phenomenon, an understanding of the mechanism of immunity was needed, and therefore, the experimental work of Emil von Behring and Shibasaburo Kitasato in 1890 gave the first insight into the mechanism of immunity. They demonstrated that serum contained elements known as antibodies. They functioned to protect against infections thus laying the foundation for the identification of humoral immunity.
- Emil von Behring received the Nobel Prize in Medicine in 1901 in recognition of his work.
- Elie Metchnikoff also demonstrated that cells contribute to the immune state of an animal in 1884, earlier before von Bekring’s demonstration of the serum elements. Metchnikoff observed that certain white blood cells, which he termed phagocytes, were able to ingest (phagocytose) microorganisms and other foreign material.
- He notes that the phagocytic cells were very active in animals that had been immunized, and hypothesized that cells were the major effectors of immunity than the serum components. The active phagocytic cells identified by Metchnikoff were most likely blood monocytes and neutrophils.
Components of the Immune System
The immune system is composed of innate immunity and adaptive immunity. The innate immunity is non-specific, meaning that it elicits responses to any foreign agent, while the adaptive immune responses are specific, eliciting immune reactions against particular antigens.
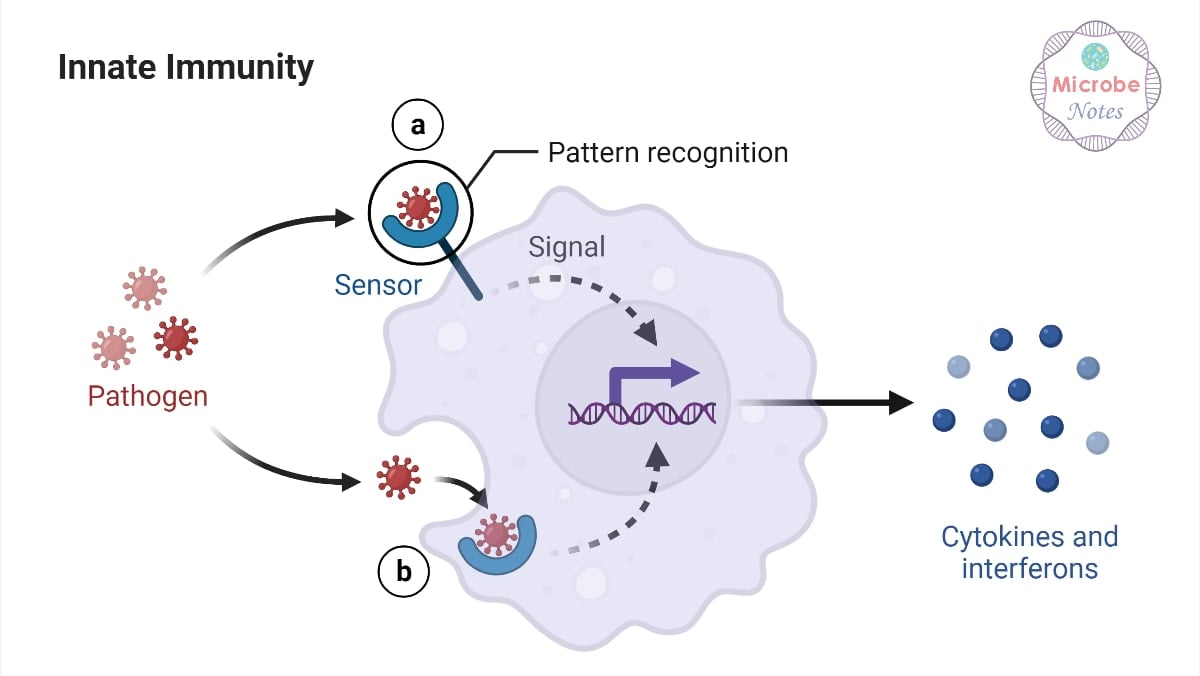
Innate immune responses
Innate immunity is considered the first line of defense against foreign agents in the host body. The components of innate immune responses are categorized into 5:
- Removing foreign agents from body tissues by non-specific white blood cells known as macrophages.
- Attracting cells of the immune system to the site of infection by releasing anti-inflammatory mediators known as cytokines and chemokines.
- Activating sequence of immune reactions that function to clearing bacteria, infected host cells, and debris known as the complement cascade.
- The innate immunity also acts as a physical barrier against the entry of foreign agents (e.g. skin is a component of the innate immune system).
- Lastly, the innate immune response acts to activate the adaptive immune system by presenting foreign, processed antigens to adaptive immunity.
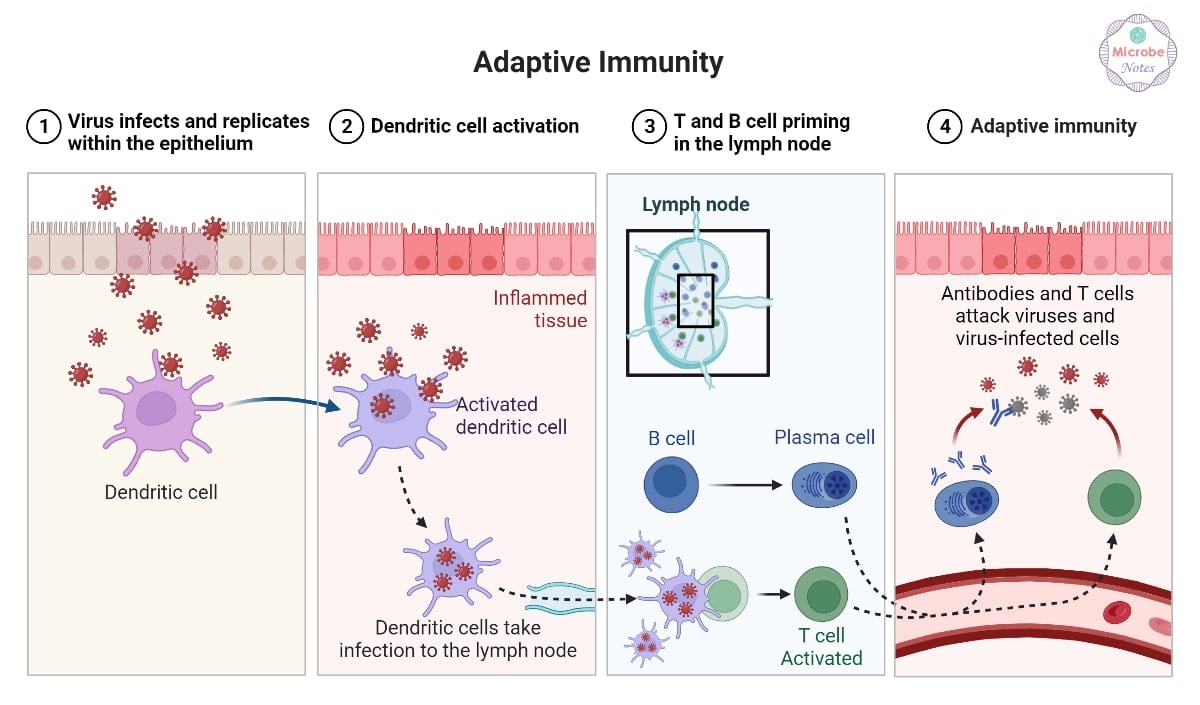
Adaptive immune Responses
- This is the most specialized immune reaction elicited by the host body.
- It aims at clearing previously encountered foreign agents with the help of two major immune cells, B-cells and T-cells.
- B cells are responsible for the secretion of antibodies specific to foreign antigens.
- T cells are responsible both for activating B cells (T helper cells) and for killing pathogens/pathogen-infected host cells (T-killer cells).
- This branch of the immune system is adaptive, because of several mechanisms it has to mature immune cells making them highly specific to antigens encountered on pathogens and subsequently presented by the innate immune system.
Immunization through Vaccination
- Immunization is the process of eliciting a long-lived state of protective immunity against a disease-causing pathogen. This means that the body is exposed to a live pathogen and after recovery, one becomes immune to the disease (common route of immunization).
- Vaccination is an intentional exposure to a form of a pathogen that does not cause disease, in the form of a vaccine.
- Immunoprophylaxis is the prevention of disease by the production of active or passive immunity. A decline in disease occurrences and breakouts for infections such as diphtheria, measles, mumps, pertussis (whooping cough), rubella (German measles), poliomyelitis, and tetanus, is because of the vaccination era.
- Vaccination as an immunoprophylactic mechanism of reducing disease occurrences and spread is a cost-effective weapon for disease prevention. It ensures a state of immune protection either by natural means (from mother to fetus) or by injection of antiserum against a pathogen. Both means provide immune protection.
- Diseases like diphtheria, pertussis, tetanus, measles, mumps, rubella, and poliomyelitis, also known as vaccine-preventable diseases have been successfully brought down to negligible levels in most developed nations and in some cases in the developing nations as well.
- The agents used for inducing passive immunity include antibodies from humans or animals, whereas active immunization is achieved by inoculation with part of the microbial pathogens/elements to induce immunity but do not cause disease or with antigenic components from the pathogens.
- Without the development of memory B or T cells specific to the organism, however, this state of immunity is only temporary. Thus, vaccination is an event, whereas immunization (the development of a protective memory response) is a potential outcome of that event.
Considering these factors, immunization can therefore be achieved in two ways:
- Passive immunization
- Active Immunization
Passive Immunization
- This type of immunization is done by transferring preformed antibodies to a recipient. These preformed antibodies are naturally formed when a mother’s IgG crosses the placenta into the developing fetus.
- Maternal antibodies to diphtheria, tetanus, streptococci, rubeola, rubella, mumps, and poliovirus all afford passively acquired protection to the developing fetus.
- Additionally, the maternal antibodies that are present in breast milk can also provide passive immunity to the infant in the form of maternally produced IgA.
- Passive immunization can also be achieved by injecting a recipient with preformed antibodies, known as the antiserum. These are acquired from an immune individual.
- Earlier on before antibiotics and vaccines became available, passive immunization was the only effective therapy for some of the most fatal diseases, like diphtheria, which meant that the humoral defense mechanisms were very much needed.
- However, presently, several other conditions still warrant the use of passive immunization such as;
- Congenital or acquired immune deficiencies of the defected B-cells
- Toxin or venom exposure with an immediate threat to life
- Exposure to pathogens that can cause death faster than an effective immune response can develop
- Passive immunity is used in unvaccinated individuals exposed to the organisms that cause botulism, tetanus, diphtheria, hepatitis, measles, and rabies or to protect travelers and health-care workers who might be exposed to potential pathogens of which the lack the protective immunity.
- Antiserum provides protection against poisonous snake and insect bites.
- Nonetheless, we should note that passive immunization does not activate the host immune responses, and hence it does not generate memory response, therefore, its protection is short-live/transient.
Negative effects of Passive immunization
- Additionally, however effective passive immunization may be, it ought to be used with caution to prevent certain risks associated with the injection of the preformed antibodies.
- Depending on where or who the donor of the preformed antibodies are acquired from, some individuals will produce a strong response to the isotypic determinants of the new/foreign antibodies, for example, if these antibodies are acquired from the horse, which is one of the most common animal sources, the recipient elicits a strong response to the isotypic determinants of the foreign antibody or part of the antibody that is unique to the horse species. Such instances arising from the anti-isotype response can cause serious complications such as the production of IgE antibody specific for horse-specific determinants leading to high levels of the IgE-horse antibodies, which can induce pervasive mast-cell degranulation leading to systemic anaphylaxis.
- Others may produce IgG or IgM antibodies that are specific for the foreign antibody, forming complement activating immune complexes, thus leading to deposition of these complexes in the tissues causing type III hypersensitivity reactions.
- Even when human antiserum, or gamma globulin, is used, the recipient can generate an anti-allotype response to the human immunoglobulin (recognition of within species antigenic differences), although its intensity is usually much less than that of an anti-isotype response.
Active Immunization
- As noted above, passive immunization provides a transient form of protection, active immunization on the other hand functions to trigger and activate the immune responses of adaptive immunity, in a way to elicit protective immunity and immunologic memory.
- Successful active immunization means that subsequent exposure to the pathogen or pathogenic agent produces a secondary immune response that can eliminate the pathogen successfully or prevent a cause of disease by the pathogen and its products.
- Active immunization as mentioned here is achieved by natural infection with microbes or by the artificial acquisition by the administration of a vaccine. When the vaccine is introduced into the host body, the immune system is activated producing antigen-reactive T and B cells, resulting in the formation of protective memory cells, which is the primary role of vaccination.
- Active immunization has played a key role in offering protection in infants and children against many infectious diseases since most of them are offered at the beginning of birth.
- Global recommendations for child immunization programs start at birth to age 6, as per the recommendations of the CDC and The American Academy of Pediatrics (updated 2012).
- The program includes the following vaccines for children from birth to age 6:
- Hepatitis B vaccine (HepB)
- Diphtheria- tetanus-( acellular) pertussis (DTaP) combined vaccine
- Haemophilus influenzae type b (Hib) vaccine to prevent bacterial meningitis and pneumonia
- Inactivated (Salk) polio vaccine (IPV)
- Measles- mumps- rubella (MMR) combined vaccine
- Varicella-zoster vaccine for chickenpox
- Meningococcal vaccine (MCV4) against Neisseria meningitidis
- Pneumococcal conjugate vaccine (PCV) or pneumococcal polysaccharide vaccine (PPSV) against Streptococcus pneumonia
- Influenza virus vaccine (seasonal flu)
- Hepatitis A vaccine (HepA)
- Rotavirus (RV)
- As per the new recommendations by CDC and The American Academy of Pediatrics, dated February 2012 young adults including males ages 11 to 12, individuals recommended receiving the vaccination against sexually-transmitted human papillomavirus (HPV), the primary cause of cervical cancer in women.
- Since 2006 this vaccine has been recommended for females, starting at age 11 to 12.
- Children’s vaccination requires boosters which are repeated inoculations, at appropriately timed intervals so as to achieve protective immunity.
- In the first months of life, the reason for this may be the persistence of circulating maternal antibodies in the young infant. For example, passively acquired maternal antibodies bind to epitopes on the DTaP vaccine and block adequate activation of the immune system; therefore, this vaccine must be given several times after the maternal antibody has been cleared from an infant’s circulation in order to achieve adequate immunity.
- The passively acquired maternal antibody also interferes with the effectiveness of the measles vaccine; for this reason, the MMR vaccine is not given before 12 to 15 months of age. In developing countries, however, the measles vaccine is administered at 9 months, even though maternal antibodies are still present because 30% to 50% of young children in these countries contract the disease before 15 months of age.
- Multiple immunizations with the polio vaccine are required to ensure that an adequate immune response is generated to each of the three strains of poliovirus that make up the vaccine.
References
- Kuby Immunology 7th Edition
- Microbiology by Prescott
- Microbiology and Immunology 2nd Edition by Shubash Chandra Parija
- 3% – http://www.jiwaji.edu/pdf/ecourse/microbiology/Active%20and%20Passive%20immunization.pdf
- 1% – https://www.nutra-supp.com/wp-content/uploads/2019/06/CUREIT_6.pdf
- 1% – https://www.britannica.com/biography/Louis-Pasteur
- 1% – https://www.austincc.edu/apreview/EmphasisItems/Inflammatoryresponse.html
- 1% – https://www.78stepshealth.us/heavy-chain/passive-immunization-involves-transfer-of-preformed-antibodies.html
- 1% – https://med.seu.edu.cn/_upload/article/files/4c/37/03879d2643f0a3ee510a3f684c84/760e6b40-a7bb-477a-9dba-66d0abfc2b04.pdf
- <1% – https://www.who.int/topics/immunization/en/?bcsi-ac-56c8c0c21347732b=28195A2600000002Mo1VyJjW6uZDMIq0Z03pt94RbsqBAgAAAgAAAE4KCgCEAwAADgAAAHX/AAA=
- <1% – https://www.thoughtco.com/the-main-animal-characteristics-4086505
- <1% – https://www.technologynetworks.com/immunology/articles/active-vs-passive-immunity-differences-and-definition-335112
- <1% – https://www.seracare.com/Human-Gamma-Globulin-Powder-1860-0047/
- <1% – https://www.sciencedirect.com/topics/medicine-and-dentistry/history-of-public-health
- <1% – https://www.sciencedirect.com/topics/medicine-and-dentistry/measles-vaccine
- <1% – https://www.sciencedirect.com/science/article/pii/S0378608000800380
- <1% – https://www.sciencedirect.com/science/article/pii/S0264410X07006974
- <1% – https://www.sciencedirect.com/science/article/pii/B9780123852458000182
- <1% – https://www.researchgate.net/publication/11216740_The_Intangible_Value_of_Vaccination
- <1% – https://www.publichealth.org/public-awareness/understanding-vaccines/vaccines-work/
- <1% – https://www.newhealthadvisor.org/Primary-Immune-Response.html
- <1% – https://www.microbiologytext.com/6th_ed/book/displayarticle/758
- <1% – https://www.medicinenet.com/t-helper_cell/definition.htm
- <1% – https://www.frontiersin.org/articles/10.3389/fimmu.2012.00313/full
- <1% – https://vaccinate.initiatives.qld.gov.au/why-immunise/facts/
- <1% – https://quizlet.com/85980587/types-of-acquired-immunity-and-vaccines-flash-cards/
- <1% – https://quizlet.com/81764615/immunity-active-and-passive-flash-cards/
- <1% – https://quizlet.com/21107170/chapter-21-the-immune-system-questions-flash-cards/
- <1% – https://quizlet.com/122861731/immunobiology-chapters-1-6-flash-cards/
- <1% – https://naturalnewsblogs.com/vaccination-blessing-of-science-or-deception-and-harm/
- <1% – https://en.wikipedia.org/wiki/Maternal_immune_tolerance
- <1% – https://en.wikipedia.org/wiki/List_of_Nobel_laureates_in_Physiology_or_Medicine
- <1% – https://en.wikipedia.org/wiki/Chemokine
- <1% – https://downloads.aap.org/AAP/PDF/periodicity_schedule.pdf
- <1% – http://www.bbc.co.uk/history/british/empire_seapower/smallpox_01.shtml
