Casts are generally regarded as the precipitation of protein along with other cells such as WBC (white blood cells), RBC (red blood cells), kidney cells, or substances such as fat bodies also sometimes microorganisms. They are formed in the lumen of the nephron of the kidney and are excreted in the urine. It can also be observed in the renal biopsy specimen. There are various casts formed in renal tubules which are considered indicators of injury in the kidney.
Hyaline Casts are the most common type of urinary casts and are also present during normal conditions. Hyaline Casts are the fundamental structure of all urinary casts and the only casts to be detected, even in the absence of any renal disease.
Interesting Science Videos
Structure and Composition of Hyaline Casts
Morphology:
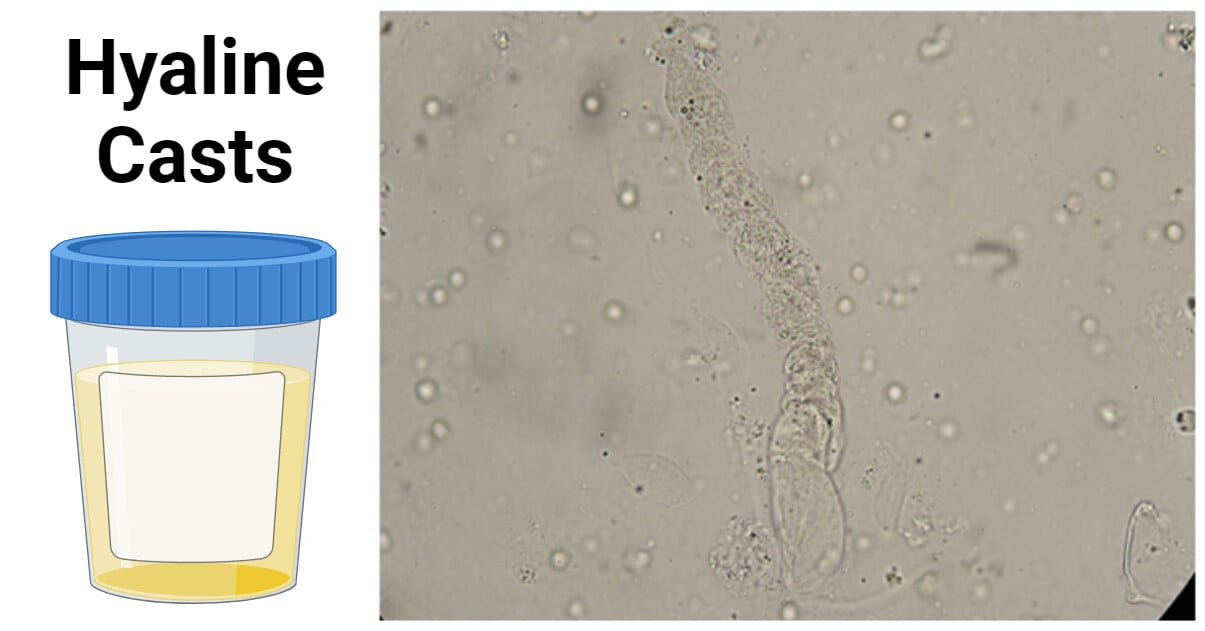
- Microscopic, homogenous tubular or cylindrical shape, with defined outer line, parallel sides, and round ends
Appearance:
- Transparent, empty appearance, smooth texture, with clear margins and blunt ends
Composition:
- These are granular structures made up of hyaline proteins called “Tamm-Horsfall” secreted by renal tubular cells. Tamm-Horsfall is the uromodulin protein, basically a precipitation of the mucoprotein.
- Consists of an acellular protein matrix (Tamm-Horsfall)
- Low refractive index
- These are the microscopic structures. However, it can go unnoticed under bright field microscopy. So, it is usually recommended to observe them under dim light. These casts can be best identified by a Phase-contrast microscope.
Types of Hyaline Casts
Hyaline casts can be broadly divided into two categories based on their composition:
Cellular casts: Consists of cellular components. These include renal tubular epithelial casts, red blood cell casts, white blood cell casts, etc.
Non-cellular casts: Consists of acellular components. These include hyaline casts, granular casts, fatty casts, and waxy casts.
Medical Importance of Hyaline Casts
Hyaline casts are found in both healthy individuals and in those with some pathological conditions.
Normal range: 0-2 casts per LPF (low power field of the microscope)
However higher amount of these casts may indicate damage in the kidney, usually due to a decline in renal perfusion (i.e. decrease in blood flow to the kidney) leading to sluggish urinary flow.
Higher levels of Hyaline casts are often observed in concentrated urine and are usually due to dehydration, strenuous exercise, diuretic medications, vomiting, fever, etc.
Medical Importance of Other Casts
Epithelial casts: indicate severe damage and death of the tubule cells called tubular necrosis; viral disease such as cytomegalovirus (CMV) nephritis; kidney transplant rejection.
Red blood cell casts: indicate damage of glomerulus known as proliferative glomerulonephritis; bleeding from the kidney (leaking of RBC). These casts are red or yellow-orange and are usually observed when there is damage in the basement of the glomerulus.
White blood cell casts: indicate kidney infection such as poly-nephritis
Bacterial casts: infection; often found mixed with WBC casts
Fatty casts: in individuals with nephrotic syndrome which causes proteinuria and increased cholesterol; observed during complications of nephrotic syndrome
Granular casts: consist of cellular debris or protein aggregates, associated with acute tubular injury (ATI)
Waxy casts: in advanced renal disease and chronic kidney failure
Process of Formation of Hyaline Casts
A pair of bean-shaped excretory organs namely kidneys are found lying retroperitoneally in the abdomen at either side of the vertebral column. Each kidney consists of millions of nephrons, a structural and functional unit of the kidney that comprises glomerulus and Malpighian tubules.
Cast formation occurs in the posterior end of the kidney tubules, consisting of distal convoluted tubules and collecting ducts. Here, the tubule acts as a mold for the formation of casts, where the thickness of the tubule determines the width of the casts.
Distal tubules form the narrower casts whereas the collecting duct is responsible for the formation of broader casts. The matrix of the cast consists of “Tamm-Horsfall” protein, a glycoprotein secretion of the distal end of the Henle loop, and the distal convoluted tubule. It is the result of precipitation of Tamm-Horsfall protein (uromodulin) secreted by epithelial tubule cells.
These proteins are aggregated in a protein matrix which then attracts the adhesion of other particles from tubules such as cells, bile, hemoglobin, albumin, etc.
Once after the formation of urinary casts, they are removed from the tubular lumen to travel through the urinary tract before being excreted in the urine.
Influencing Factors/ Causes of Hyaline Casts
pH: Low pH or highly acidic environment favors the precipitation of protein leading to the formation of Hyaline casts.
Dehydration: Dehydration causes an increase in the levels of protein directing the formation of hyaline casts.
Strenuous exercise/ Intense physical exercise: It can cause dehydration resulting in its formation.
Fever: Fever can cause a rise in levels of protein and hence the formation of casts
Vomiting: It can cause dehydration in the body hence making the environment suitable for the formation of the casts.
Kidney injury: Kidney injury or kidney disease such as glomerulonephritis, interstitial nephritis, or diabetic neuropathy can lead to the formation of Hyaline casts.
Urinary tract infection: It can cause inflammation and damage to the kidney consecutively resulting in the formation of Hyaline casts in the urine.
Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) might result in an increase in the concentration of protein in the urine resulting in the formation of Hyaline casts.
Diagnosis of Hyaline Casts
Hyaline casts can be detected in laboratory settings by urinary sediment microscopy, a process called urinalysis.
Sample: morning urination; mid-stream urine collected in a sterile container
Centrifuge urine sample.
↓
Separate suspended particles such as casts, cells, and microorganisms sediment from the fluid.
↓
Place a drop of urine sediment on a glass slide.
↓
Examine under the microscope.
- Under field microscopy, hyaline casts appear as clear, tiny tubule-shaped particles.
- Use of dim lighting or use of phase contrast microscopy can be used for better visualization.
Clinical Significance of Hyaline Casts
Hyaline casts can be of high significance in providing diagnostic information for physicians. They may be present in low numbers (0-2/LPF) in the concentrated urine which is usually considered normal. However, the number of Hyaline casts increases with renal disease. The presence of casts usually indicates renal disease rather than lower urinary tract infection and may even be present without significant proteinuria.
Even if these casts are observed also in healthy individuals, sometimes they can indicate severe conditions such as:
- Acute glomerulonephritis
- Pyelonephritis
- Chronic renal failure
- Congestive heart failure
- Spillover proteinuria
High hyaline cast levels may also indicate kidney damage most probably due to decreased blood flow to the kidneys. Hence, patient medical history, including information on recent medication and illness can be of great importance in diagnosis.
Preventive Methods of Hyaline Casts
Staying hydrated: Staying hydrated can help prevent dehydration, as dehydration is the major cause of the formation of hyaline casts.
Medical treatment/ discontinuing medications: Taking proper health treatment, for underlying medical conditions such as hypertension or diabetes can prevent the formation of these casts.
Avoiding excessive/strenuous exercise: Excessive exercise causes dehydration which ultimately leads to the formation of Hyaline casts. So, it should be avoided.
Regular medical checkups: Regular checkups help in the identification of underlying medical conditions before the formation of the high number of casts and their excretion in the urine.
Avoiding NSAIDs: Some non-steroidal anti-inflammatory drugs can increase protein concentration, so minimizing it can lead to the prevention of the formation of casts.
Conclusion
In conclusion, Hyaline casts are present normally in the urine and are not painful to excrete but are potential parameters for the detection of various kidney-associated diseases.
References
- Benovska, M., Wiewiorka, O. & Tumova, J. MIcroscopic analysis of urine. Retrieved from https://is.muni.cz/do/rect/el/estud/lf/js15/mikroskop/web/pages/valce_en.html. Accessed on 3rd January 2023.
- Cavanaugh, C., & Perazella, M. A. (2019). Urine Sediment Examination in the Diagnosis and Management of Kidney Disease: Core Curriculum 2019. American journal of kidney diseases: the official journal of the National Kidney Foundation, 73(2), 258–272. https://doi.org/10.1053/j.ajkd.2018.07.012
- Dvanajscak, Z., Cossey, L. N., & Larsen, C. P. (2020, May). A practical approach to the pathology of renal intratubular casts. In Seminars in Diagnostic Pathology (Vol. 37, No. 3, pp. 127-134). WB Saunders. https://doi.org/10.1053/j.semdp.2020.02.001
- Formation and Significance of Casts. 23rd June 2016.Retrieved from https://www.labce.com/spg30115_formation_and_significance_of_casts.aspx. Accessed on 2nd January 2023.
- Hernandez, A. Hyaline Casts. Osmosis from Elseier. Retrieved from https://www.osmosis.org/answers/hyaline-casts. Accessed on 4th January 2023.
- Hyaline Casts in Urine. 14 December 2022. Laboratory info. Retrieved from https://laboratoryinfo.com/hyaline-casts-in-urine/. Accessed on 3rd January 2023.
- Hyaline Casts in Urine. Microbiologie Clinique. Retrieved from https://microbiologie-clinique.com/en/hyaline-casts-in-urine.html. Accessed on 3rd January 2023.
- Hyaline Casts. 30th March 2023. Lab Test Guide. Retrieved from https://www.labtestsguide.com/hyaline-casts. Accessed on 4th |January 2023.
- Karen M. Ringsrud, Casts in the Urine Sediment, Laboratory Medicine, Volume 32, Issue 4, April 2001, Pages 191–193, https://doi.org/10.1309/KJ5E-V5FE-MAHR-KXT2
- McPherson, R. A., & Pincus, M. R. (2021). Henry’s clinical diagnosis and management by laboratory methods E-book. Elsevier Health Sciences.
- Srakocic, S. (21 March 2023). Different Types of Urinary Casts. Healthline. Retrieved from https://www.healthline.com/health/urinary-incontinence/types-of-urinary-casts. Accessed on 2nd January 2023.
- Tietze, K. J. (2012). Review of Laboratory and Diagnostic Tests. Clinical Skills for Pharmacists, 86–122. doi:10.1016/b978-0-323-07738-5.10005-5
- Urinary Casts. Mount Sinai. Retrieved from https://www.mountsinai.org/health-library/tests/urinary-casts. Accessed on 4th January 2023.
