Interesting Science Videos
Introduction
- Giardia duodenalis is also known as Giardia lamblia and Giardia intestinalis.
- It is a flagellated unicellular eukaryotic microorganism that colonizes and reproduces in the small intestine.
- It commonly causes a gastrointestinal condition known as Giardiasis.
Classification of Giardia duodenalis
- There are five species of Giardia, out of that, G. intestinalis infects humans and other mammals.
- G. duodenalis can further be differentiated into seven genotypes from A to G, out of which genotypes A and B usually infect humans.
History and Distribution of Giardia duodenalis
- It is one of the earliest protozoan parasites to have been recorded.
- It was first observed by Dutch scientist Antonie van Leeuwenhoek (1681) in his own diarrheal stools.
- It is named Giardia after Professor Giard of Paris and lamblia after Professor Lambie of Prague, who gave a detailed description of the parasite.
- It was initially thought to be commensal, it has been recognized as a pathogen since the mid-1900s.
- It is the most common protozoan pathogen causing both endemic and epidemic intestinal disease and diarrhea and worldwide in distribution.
- Its prevalence is high in people with low socio-economic status and poor living conditions as well as people in over-crowded areas with poor environmental sanitation, improper garbage disposal, unsafe water supply, and unhygienic personal habits.
Habitat of Giardia duodenalis
- Giardia duodenalis lives in the duodenum and upper jejunum.
- It is the only protozoan parasite found in the lumen of the human small intestine.
Morphology of Giardia duodenalis
Giardia duodenalis exists in two forms- Trophozoite (or vegetative form) and Cyst (or cystic form).
1. Trophozoite
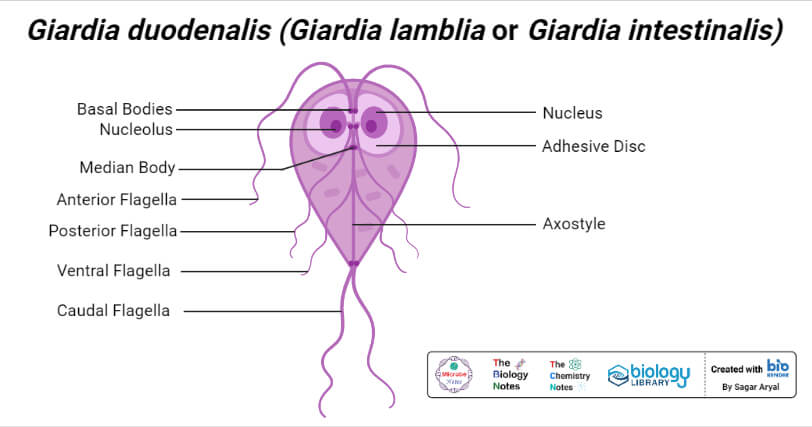
- The trophozoite is in the shape of a tennis racket (heart-shaped or pyriform-shaped).
- It is rounded anteriorly and pointed posteriorly.
- It has falling leaf-like motility and measures 12-15 µm length and 4µm thick.
- It is dorsoventrally convex and ventrally, it has a concave sucking disk, which helps in its attachment to the intestinal mucosa. Hence, it appears as sickle-shaped in lateral view.
- It is bilaterally symmetrical on each side from the midline and it possesses:
- One pair of nuclei
- Four pairs of flagella (two lateral, one ventral, and one caudal pair of flagella)
- Blepharoplast, from which the flagella arise (four pairs).
- One pair of axostyles, running along the midline.
- Two sausage-shaped parabasal or median bodies, lying transversely posterior to the sucking disk.
- It lives in the duodenum.
2. Cyst
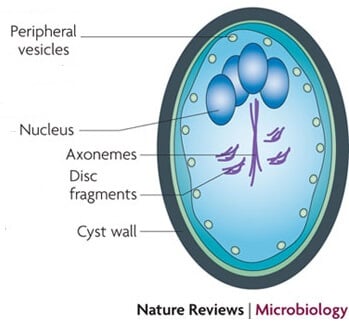
Figure: Giardia duodenalis cyst. Image Source: Nature Reviews Microbiology.
- A cyst is oval in shape and measures 11–14 μm in length and 7–10 μm in width.
- It is surrounded by a hyaline cyst wall: which likely protects them from the environment.
- It contains two or four nuclei depending upon the stage of maturity.
- The axostyle lies diagonally, forming a dividing line within the cyst wall.
- It also contains remnants of axonemes, basal bodies, and parabasal bodies.
- It is the infective form as well as the diagnostic form of the parasite.
Life cycle and Mode of Transmission of Giardia duodenalis
Host- Giardia passes its life cycle in one host.
Infective Form- Mature cyst.
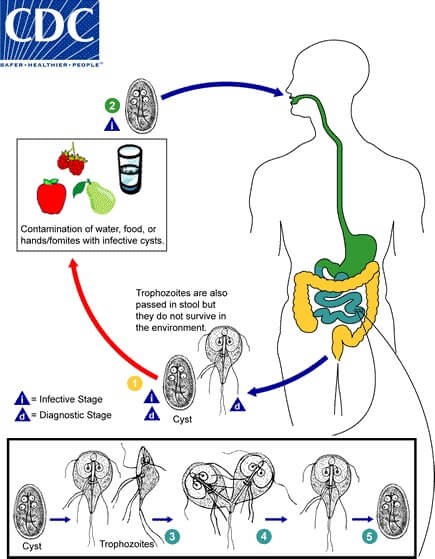
Figure: Life cycle of Giardia duodenalis. Image Source: CDC.
- Cyst are the transmission stage and are excreted in the feces of infected individuals into an environment where they can survive for weeks.
- Man acquires infection by ingestion of cysts in contaminated water and food.
- Ingestion of as far as 10 cysts are sufficient to cause infection in a man.
- Children are commonly affected.
- Direct person-to-person transmission may also occur in children, male homosexuals, and mentally ill persons.
- Enhanced susceptibility to giardiasis is associated with blood group A, achlorhydria, use of Cannabis, chronic pancreatitis, malnutrition, and immune defects such as 19A deficiency and hypogammaglobulinemia.
- Within half an hour of ingestion, excystation takes place in the small intestine where two trophozoites are release from each cyst.
- The trophozoites attach to epithelial cells of the upper intestine, primarily the jejunum but also the duodenum, where they grow and multiply by binary fission.
- Attachment is required to prevent swept away by peristalsis and is mediated by the ventral disc of trophozoites as well as adhesins on the parasitic surface.
- In the active stage of the diseases, sometimes the trophozoites are excreted in diarrhea stool.
- During unfavorable conditions, encystment occurs usually in the colon.
- The appearance of Encystation-specific vesicles (ESV) in the cytoplasm helps in the processing and transportation of the cyst wall protein antigens to the exterior of the plasma.
- Encystment begins with the retraction of the flagella followed by condensation of the cytoplasm and finally the formation of the cyst wall. On maturation, nuclei divide to become four. Then, mature cysts are passed in the stool and remain viable in soil and water for several weeks, and are infective to man.
- The promoting factor for encystation are the conjugated bile salts, alkaline pH, and cholesterol starvation.
- There may be 200,000 cysts passed per gram of feces.
- The infective dose is 10–100 cyst.
Pathogenicity of Giardia duodenalis
- As few as 10–25 cysts can initiate the infection.
- G. duodenalis is typically seen within the crypts of duodenal and jejunal mucosa.
- It is an intestinal parasite and non-invasive but remains tightly adhered to the intestinal epithelium by means of the sucking disc.
- This cause disruption of the intestinal epithelial brush border that leads to increase permeability and malabsorption
- Variant specific surface proteins (VSSP) of giardia play an important role in the virulence and infectivity of the parasite.
- The malaabsorption is of various types: Malabsorption of fat (steatorrhea)— leads to foul-smelling profuse frothy diarrhea, Disaccharidase deficiencies (lactate, xylose)—leading to lactose intolerance, Malabsorption of vitamin B12 and folic acid, and Protein-losing enteropathy.
Clinical manifestation of Giardia duodenalis
- The incubation period is variable, usually 2 weeks.
- In the majority of cases, infection remains asymptomatic.
- Symptomatic infection is more common in children than adults because of their lower immunity.
1. Acute giardiasis
- The incubation period varies from 1 week to 3 weeks (average 12–20 days).
- Symptoms may develop suddenly or gradually.
- The common symptoms include diarrhea, abdominal pain, bloating, belching, flatus. Occasionally nausea, vomiting, fever, rashes, or constipation in some.
- Diarrhea is often foul-smelling with fat and mucus but no blood.
- The acute stage lasts for 1 week but usually resolves spontaneously. Very rarely, in some children may last for months.
2. Chronic giardiasis
- It may present with or without a previous acute symptomatic episode.
- Symptoms are intermittent and recurring.
- The common symptoms include chronic foul-smelling diarrhea with malabsorption of fat (steatorrhoea), malabsorption of vitamin A and B12, disaccharides, especially lactose and, protein, with malabsorption of fats and lactose being the most common and profound weight loss leading to growth retardation.
- Uncommon symptoms such as—fever, presence of blood and/or mucus in the stools, and other signs and symptoms of colitis.
- It lasts for several weeks.
- Extraintestinal manifestations are rare but sometimes such as urticaria anterior uveitis, salt, and pepper retinal changes, and arthritis are seen in rare cases.
Laboratory diagnosis of Giardia duodenalis
Specimen: Stool, duodenal contents, bile stained mucus, duodenal/jejunal biopsy.
a. Stool Examination
- Giardiasis can be diagnosed by the identification of cysts of Giardia lamblia in the formed stools and the trophozoites and cysts of the parasite in diarrheal stools.
- Macroscopic examination: offensive odor, are pale-colored and fatty and float in water.
- Microscopic examination:-Direct wet mount preparations of the diarrheal stool where trophozoites are identified by falling leaf-like motility indicate the active stage of the disease. Iodine wet preparations: cyst can be observed.
- Concentration techniques like formal ether or zinc acetate are employed to increase the chance of detection of parasites in microscopy.

Figure: Giardia duodenalis cysts in wet mounts under differential interference contrast (DIC) microscopy. Image Source: CDC.
b. Entero-test (string test)
- If stool examination is negative, then direct duodenal samples like aspirates (obtained by entero-test) or biopsy (done by endoscopy) should be processed.
- The string test uses a gelatin capsule attached to a thread.
- One end of the thread is attached to the inner aspect of the patient’s cheek, and then, the capsule is swallowed.
- Capsule gets dissolved in the intestine releasing the thread which is kept there for 4–6 hours to take the duodenal fluid.
- Later, the thread is withdrawn and shaken in saline to release trophozoites which can be detected microscopically.
- The entero-test is also useful in the search for other upper intestinal parasites.
- This invasive test is not more sensitive for detecting parasites but can be used when the more widely-used diagnostic methods fail.
c. Serodiagnosis
Antigen detection in the stool (Copro-antigen)
- Enzyme-linked immunosorbent assay (ELISA), immunochromatographic strip tests, and indirect immunofluorescent (IIF) tests using monoclonal antibodies have been developed for the detection of Giardia antigens in feces.
- The presence of antigen indicates active infection.
- Commercially available ELISA kits (ProSpec T/Giardia kit) detects Giardia-specific antigen 65 (GAS 65).
- The sensitivity of the test is 95% and specificity is 100% when compared to conventional microscopy.
- The test may be used for the quantification of cysts.
- They are very useful in microscopy negative samples and also in outbreak situations or in institutional settings when screening large numbers of people.
Antibody detection
- IIF test and ELISA are used to detect antibodies against Giardia.
- The demonstration of antibodies is useful in epidemiological and pathophysiological studies.
- These tests cannot differentiate between recent and past infections and lack sensitivity and specificity.
d. Molecular Method
- DNA probes and polymerase chain reaction (PCR) have been used to demonstrate the Giardia-specific nucleic acid.
- It is a highly specific and sensitive test.
Treatment of giardiasis of Giardia duodenalis
- Nitroimidazole, metronidazole and tinidazole are drug of choice.
- Metronidazole (250 mg, thrice daily for 5-7 days dose) andtinidazole (2g single dose)
- The cure rate with metronidazole is more than 90%.
- Furazolidone and nitazoxanide are preferred in children, as they have fewer adverse effects.
- Parmomycin, an oral aminoglycoside can be given to symptomatic pregnant females.
Prophylaxis of Giardia duodenalis
- Proper disposal of wastewater and feces.
- The practice of personal hygiene like hand-washing before eating and proper disposal of diapers.
- Prevention of food and water contamination.
- Community chlorination of water is ineffective for inactivating cysts.
- Boiling or filtering of potentially contaminated water.
References and Sources
- https://www.doctoralerts.com/giardia-lamblia-g-intestinalis-g-duodenalis-morphology-life-cycle-diseases-symptoms-treatment/ – 7%
- https://clinicalgate.com/schistosomiasis-and-other-trematode-infections/ – 5%
- https://en.wikipedia.org/wiki/Giardia_lamblia – 4%
- https://www.slideshare.net/AnupBajracharya1/giardiasis-179329625 – 2%
- https://www.learninsta.com/giardia-lamblia-of-medical-parasitology/ – 1%
- https://bestpractice.bmj.com/topics/en-gb/353/treatment-algorithm – 1%
- https://www.vin.com/apputil/content/defaultadv1.aspx?id=5124212&pid=11343&print=1 – <1%
- https://onlinelibrary.wiley.com/doi/full/10.1042/BC20070173 – <1%
- https://en.wikipedia.org/wiki/Intestinal_malabsorption – <1%

I like de full detailed content, it has improve knowladge under the Giardia lamblia soo much. am I able to get it in a PDF form? if i may ask…
Sorry, we dont have PDF. You can look contents from our website 🙂