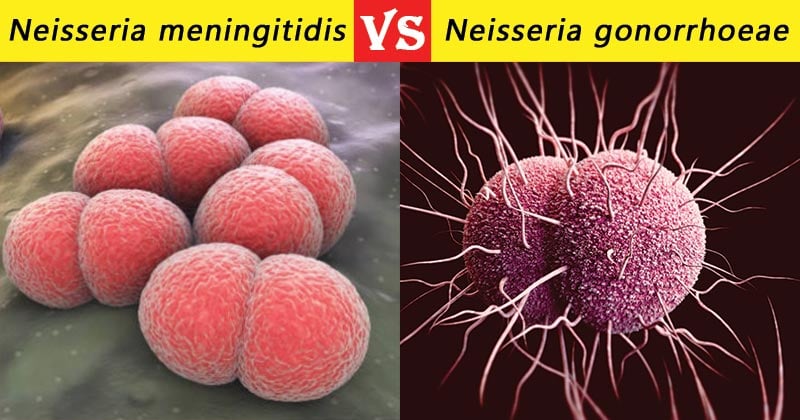
Neisseria meningitidis and Neisseria gonorrhoeae, are obligate human pathogens that cause distinctly different disease syndromes. They are both Gram negative diplococci, non-sporing, oxidase positive and difficult to differentiate on morphological and cultural characteristics.
Interesting Science Videos
However, they can be differentiated on the following grounds:
S.N. |
Character |
Neisseria gonorrhoeae |
Neisseria meningitidis |
| 1. | Commonly Called | Gonococcus | Meningococcus |
| 2. | Causative agent of | Sexually transmitted disease- Gonorrhoea | Causes a range of diseases embraced by the term invasive meningococcal disease. Most commonly cerebrospinal meningitis. |
| 3. | Cell Morphology | Kidney shaped with apposing ends concave. | Semicircular diplococcus with flat apposing ends. |
| 4. | Capsule | Absent | Capsule is present which is anti-phagocytic and an important virulence factor. |
| 5. | Pili | N. gonorrhoeae most often moves using one retracting pilus. | N. meningitidis most often move using four pili. |
| 6. | Plasmids | Usually possess plasmids, coding for drug resistant genes. | Rarely have plasmids |
| 7. | Form | Predominantly exist in
intracellular form |
Exist in both intra· and
extracellular forms |
| 8. | Movement | Movement of N. gonorrhoeae occurs at lower speed. | Movement of N. meningitidis occurs faster with a larger number of retracting pili. |
| 9. | Growth on Blood Agar | N. gonorrhoeae grow less well on blood agar than N. meningitidis. | N. meningitidis grow well on blood agar than N. gonorrhoeae |
| 10. | Culture medium | Contain antimicrobials that inhibit the growth of organisms other than N. gonorrhoeae; typically vancomycin (inhibits Gram-positive bacteria), colistin (inhibits gram-negative bacteria including the commensal Neisseria spp.), trimethoprim (inhibits swarming of Proteus spp.) and nystatin or amphotericin B (antifungal agents). | Blood agar, trypticase soy agar, supplemented chocolate agar, and Mueller-Hinton agar. |
| 11. | Growth Rate | Slower than Meningococcus. | Slow |
| 12. | Fastidious | Most fastidious among Neisseria spp. | Comparatively less fastidious. |
| 13. | Colony morphology | N. gonorrhoeae form smooth, round, moist, uniform grey/ brown colonies with a greenish colour underneath on primary isolation medium.
Mostly, has a irregular margin. |
N. meningitides would form smooth, round, moist, uniform
large grey/brown colonies with a glistening surface and entire edges. |
| 14. | Sugar Fermentation | Produce acid from glucose only | Produce acid from glucose and maltose. |
| 15. | Maltose Fermentation | No | Yes |
| 16. | Nitrite Reduction | N. gonorrhoeae doesn’t reduce nitrites. | N. meningitidis can reduce nitrites in low concentrations. |
| 17. | Autolysis | May autolyse | Autolyse |
| 18. | Glutamylaminotransferase | Non-producer | Producer |
| 19. | Β-Lactamase Production | Common | Rare |
| 20. | Antigen Heterogeneity | More than meningococci. | Comparatively less. |
| 21. | Grouping | Strains characterized by auxotyping which recognizes reqiurements for specific nutrients. | Serogroup is determined by its lipopolysaccharide capsular antigen. |
| 22. | Normal Flora | Not considered as normal flora. | Many normal individuals may harbor Neisseria meningitidis in the upper respiratory tract |
| 23. | Pathogen | It is always a pathogen. | It may or may not be pathogenic. |
| 24. | Portal of Entry | Genital | Respiratory |
| 25. | Site of Infection | Primarily causing infection of the anogenital tract. | Colonizes the upper respiratory tract as a commensal and occasionally invades to
cause systemic disease. |
| 26. | Virulence Factors | Pili, IgA proteases and production of lipopolysaccharide endotoxin. | LPS capsule, IgA protease and iron utilizationfrom transferrin. |
| 27. | Related Conditions | N. gonorrhoeae can also cause conjunctivitis, pharyngitis, proctitis or urethritis, prostatitis, and orchitis. | Cause meningitis and other forms of meningococcal disease such as meningococcemia, a life-threatening sepsis. |
| 28. | Specimens | Transport swab of endocervix, urethra, rectum, pharynx, conjunctiva, blood, joint fluid, aspirates from skin lesions. | Cerebrospinal fluid (CSF) and blood, swab skin lesions and nasopharynx. |
| 29. | Presence in inflammatory exudates (pus) | In larger proportions | In less numbers |
| 30. | Prevalence and Mortality | N.gonorrhoeae infections have a high prevalence and low mortality. | N. meningitidis infections have a low prevalence and high mortality. |
| 31. | Superbug | Considered as “superbug” | Not considered as “superbug” |
| 32. | Vaccines | No | Serogroup A, B, C, Y and W-135 meningococcal infections can be prevented by vaccines. |
References
- Greenwood, D., Slack, R. C. B., Peutherer, J. F., & Duguid, J. P. (1992). Medical microbiology: A guide to microbial infections : pathogenesis, immunity, laboratory diagnosis, and control. Edinburgh: Churchill Livingstone.
- Sastry A.S. & Bhat S.K. (2016). Essentials of Medical Microbiology. New Delhi : Jaypee Brothers Medical Publishers.
- Parija S.C. (2012). Textbook of Microbiology & Immunology.(2 ed.). India: Elsevier India.
- https://microbiologyinfo.com/difference-between-neisseria-gonorrhoeae-and-neisseria-meningitides/
- https://www.jfmed.uniba.sk/fileadmin/jlf/Pracoviska/ustav-mikrobiologie-a-imunologie/NEISSERIA_AND_HAEMOPHILUS.pdf
- http://textbookofbacteriology.net/neisseria.html
