Interesting Science Videos
What is Candida tropicalis?
Candida tropicalis is a yeast form of fungi known to be pathogenic in neutropenic hosts and disseminating through the bloodstream to peripheral organs.
- It is closely related to Candida albicans in pathogenicity and clinical features.
- It is a common systemic fungus, affecting persons with immune-compromised and immune-suppressed systems.
- The common treatment therapies for invasive infection of Candida tropicalis are amphotericin B, echinocandins, broad-spectrum triazole antifungals.
- It is also known to cause infections when the normal microbiota in the human host has been compromised by intake on antimicrobial agents such as antibiotics or when the sugar levels are high in the system.
Habitat of Candida tropicalis
- Candida tropicalis is one of the fungal species that has been obtained from seawater, sea sediments, mudflats, marine fish intestine, mangrove plants, and marine algae, shrimps.
- Therefore, they are widely distributed in the tropical and subtropical marine environments.
- It is also dominantly found in the human gut, fruit surfaces, a variety of foods and soil.
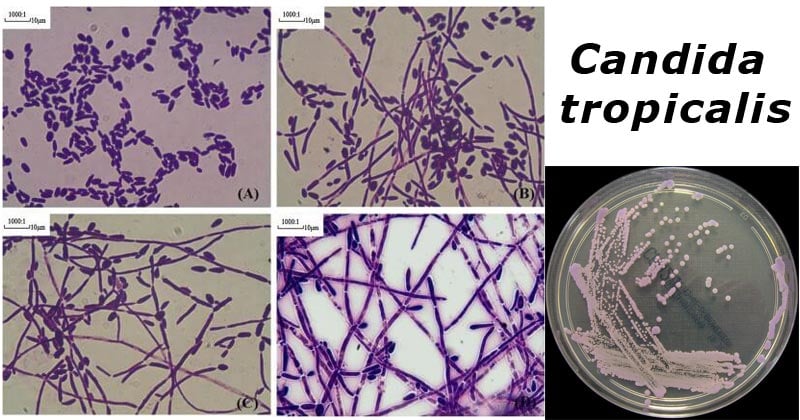
Figure: Four classes of morphologic change in hyphae formation of C. tropicalis. 5 × 106 C. tropicalis cells (20 μl) were inoculated in RPMI 1640 medium supplemented with 10% Fetal Bovine Serum at 37 °C for 12 h. Cells were Gram-stained and observed by light microscopy at 100× magnification. A–D represented Class I–IV, respectively. Image Source: https://doi.org/10.1016/j.micres.2016.06.003.
Figure: Candida tropicalis growing on ChromID Candida 2 Agar. Image Source: Flickr.
Morphological features of Candida tropicalis
- Candida tropicalis is a vegetative cell that is round or oval-shaped with a diameter of 2-10um.
- These species of candida fungi are known to produce colored pigments on the cultural media, of red, pink, or orange color.
- They are dimorphic forming single-celled blastoconidia.
- They reproduce by budding unipolar or bipolar.
- The blastoconidia buds are formed on stalks, which are needle-shaped.
- The buds are pigmented and septate which form pseudohyphae.
Cultural Characteristics of Candida tropicalis
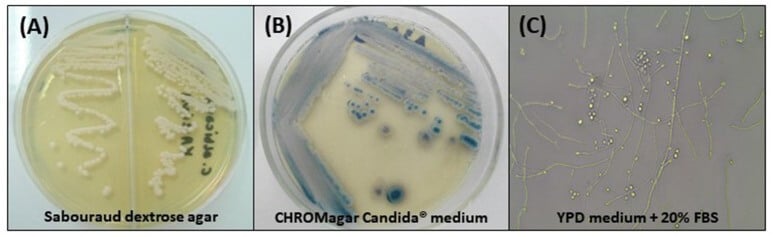
Figure: Cultural Characteristics of Candida tropicalis. (A) Cream-colored, dull, smooth colonies, after 48 h of incubation at 30°C on Sabouraud dextrose agar; (B) Colonies with typical dark blue color on CHROMagar Candida® medium after 96 h of incubation at 35°C; (C) Micromorphological aspects after incubation in YPD medium containing 20% fetal bovine serum (FBS) for 7 days at 30°C, 400x: blastoconidia in single or branched chains, true hyphae, and abundant pseudohyphae. Image Source: https://doi.org/10.3389/fmicb.2017.01927.
- Candida tropicalis grows at an optimal temperature of 25–35 °C (77–95 °F).
- Their growth thrives in sugar and fat media.
- Sabourand dextrose agar or yeast potato dextrose agar produces cream-colored or off white to grey, dull, smooth, soft, and creamy or wrinkled or rough. This media suppresses conidia growth but promotes the formation of mycelium.
- Cornmeal agar produces thrived conidia (blastoconidia).
- They can also grow in Potato Dextrose Agar, Potato-glucose, potato-carrot, tomato juice, and lima bean media.
Pathogenesis of Candida tropicalis
Candida tropicalis is one of the most common Candida species that colonize the human host causing pathogenic infections on human skin, in the gastrointestinal tract, and also in the female genitourinary tract.
Transmission of Candida tropicalis
- The most common mode of transmission is the nosocomial transmission between health-care workers and patients.
- The fungi, which is predominantly found in immune-compromised patients with HIV/AIDS, cancer, leukemia, organ transplantation, causes a fungal infection known as candidiasis in various organ systems of the body.
Virulence Factors of Candida tropicalis
- Blastoconidial spores are resistant to several environmental factors that allow it to grow and thrive in natural and human host environments. Therefore, they can survive on the hands for over 24 hours before it is transmitted to a different host.
- Colonization abilities of Candida tropicalis have been linked to the formation of a biofilm on the surface of the epithelial and endothelial cell lining.
- Adherence is due to the secretion of enzymatic enzymes such as protease which allows the fungi to penetrate the epithelial lining to cause infection.
- Protease enzymes help in the hydrolyzation of the peptide bonds and support the attachment and colonization into the deep tissues hence causing organ infections.
- Phospholipids hydrolyze the phospholipids which help in penetrating the hyphal tips into the epithelial cell membrane into the cytoplasm.
- Other factors that contribute to the fungi colonization on the epithelial and endothelial cell lining includes:
- immunocompromised system of the host
- long term administration of antimicrobial agents such as antibiotics
- Use of catheters for a prolonged period of time.
- Overuse of antifungals
Clinical Features of Candida tropicalis infection
Infections caused by Candida tropicalis vary on the site of localization of the fungi. The various clinical manifestations include:
- Superficial and mucosal candidiasis
- It is associated with oral thrush (oropharyngeal candidiasis), angular cheilitis, and vulvovaginal candidiasis.
- Oral thrush is also known as oropharyngeal candidiasis is the colonization of the tongue and the mouth cavity.
- Colonization is by the secreted enzymes of Candida tropicalis which allow it to evade the immune mechanisms of the host, and colonize the epithelial lining.
- It can also cause superficial infections of the skin and nails (onychomycosis).
- Candiduria is also common in diabetic patients, catheterized patients, and leukemic patients.
- Interdigital candidiasis, diapers rash are common superficial infections caused by C. tropicalis.
- Systemic Candidiasis
- Disseminated candidiasis
- Gastrointestinal candidiasis – this is when C. tropicalis colonizes the gastrointestinal tract in patients likely to develop invasive candidiasis
- Candidemia – This is the spread and effect of C. tropicalis on the internal organs of the human host. It is common amongst cancer patients with leukemia or neutropenia. This infection can be acquired nosocomially.
- Chronic Disseminated Candidiasis
- This is severe dissemination of candidiasis in leukemic patients and secondary neutropenia patients.
- They affect the liver, spleen, and kidney.
Laboratory Diagnosis of Candida tropicalis
Specimen: Skin scarping, oral and genital swabs, Tissue biopsies, blood, cerebrospinal fluid (CSF), or urine.
Microscopic Examination
- 10% KOH wet mount from skin scrapings or tissue biopsies for identification of pseudohyphae
- Differential stains including Haematoxylin and eosin, periodic acid–Schiff and Gomori–Grocott methenamine silver stains are the preferred for differential diagnosis of fungal infection in tissue sections taken from biopsy or autopsy specimens.
Cultural Identification
- Using Saboraud Dextrose Agar, and/or Yeast extract agar to produce smooth, shiny colonies with the formation of small blastoconidial spores held by a hyphal stalk structure (mycelium).
- Cornmeal agar to produce smooth blastoconidia spores.
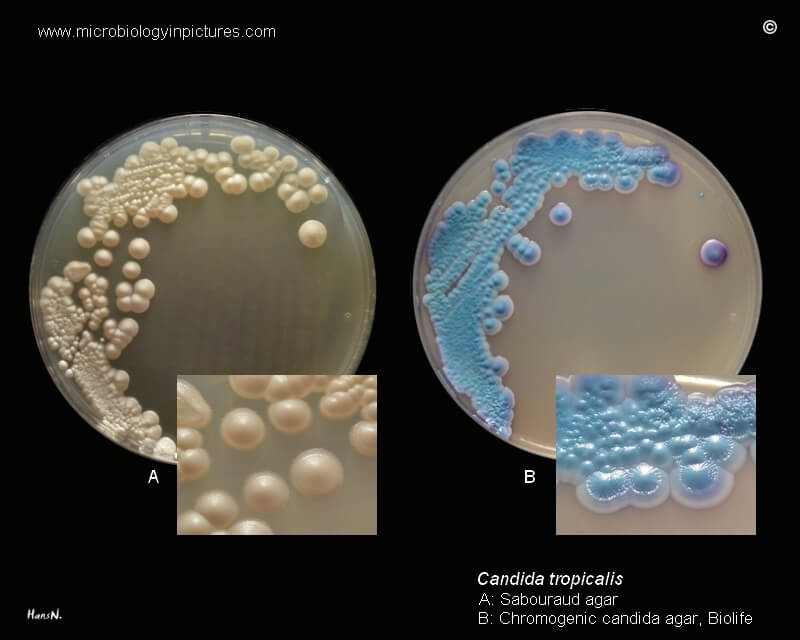
Figure: Candida tropicalis on Sabouraud agar and Chromogenic candida agar. Image Source: Microbiology In Pictures.
Biochemical Characterisation
- This test is used for the detection of the production of acetic acid.
- Fermentation on various sugars and production of inositol element in carbon sources.
- Production of urease is common among the C. tropicalis groups.
Molecular Detection
- Polymerase Chain Reaction for detection of genotyping
Treatment of Candida tropicalis infections
- Candida tropicalis infections are treated with antifungal agents.
- Most commonly, amphotericin B is used to treat Candida infections.
- Topical antifungals which are administered orally or applied topically.
- Topical antifungals such as nystatin are used for the treatment of superficial skin and nail infections.
- Oral antifungals are used for treating oral thrush and gastrointestinal candidiasis.
- Flucytosine such as caspofungin, micafungin, and anidulafungin are used to treat oropharyngeal and esophageal candidiasis and invasive candidiasis
- Systemic candidiasis is treated with amphotericin b and/or lower doses of fluconazole.
- New generation broad-spectrum fluconazole known as voriconazole is used to treat recurrent candidiasis in HIV/AIDS patients who have developed fluconazole resistance.
Candida tropicalis Antifungal resistance
- Candida tropicalis has developed resistance to fluconazole over time and therefore it is not recommended for treatment of recurrent candidiasis. Fluconazole acts against the phospholipase linkage to the host epithelial cells, which assist in adherence.
- If its mode of action is not effective, highly active agents such as itraconazole, voriconazole, posaconazole, ravuconazole, and isavuconazole.
- A new generation broad-spectrum antifungal fluconazole drug known as voriconazole was developed to tackle the resistance of Candida tropicalis.
Prevention and Control of Candida tropicalis
- Hygienic washing of hands to get rid of fungal spores on the hands to prevent the spread of the fungi.
- Washing infected surfaces using water and ethyls.
References and Sources
- 3% – https://en.wikipedia.org/wiki/Candida_tropicalis
- 1% – https://www.tandurust.com/infections/candida-tropicalis-causes-symptoms.html
- 1% – https://www.biologydiscussion.com/micro-biology/fungal-infections-classification-and-laboratory-diagnosis/30093
- 1% – https://www.bfr.bund.de/cm/349/can-the-new-type-of-coronavirus-be-transmitted-via-food-and-objects.pdf
- 1% – https://microbenotes.com/candidiasis/
- 1% – https://bodytomy.com/internal-organs-of-human-body
- <1% – https://www.uptodate.com/contents/chronic-disseminated-candidiasis-hepatosplenic-candidiasis
- <1% – https://www.sciencedirect.com/science/article/pii/S2095809917301492
- <1% – https://www.sciencedirect.com/science/article/pii/S0966842X16301366
- <1% – https://www.ncbi.nlm.nih.gov/pubmed/22203604
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4086041/
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1722213/
- <1% – https://bnfc.nice.org.uk/treatment-summary/antifungals-systemic-use.html
- <1% – https://biologyreader.com/acetic-acid-production.html
- <1% – https://academic.oup.com/jpids/article/6/suppl_1/S22/4100190
- <1% – https://academic.oup.com/cid/article/36/Supplement_1/S31/302495
- <1% – http://www.jbc.org/content/237/2/389.full.pdf
