Blastomyces dermatitidis is a thermally dimorphic fungus that causes blastomycosis, a chronically invasive fungal infection of the lungs, that disseminates into the skin and bones and it affects both humans and animals.
- The disease is predominantly endemic in North America (the United States and Canada) hence it has been coined as North America Blastomycosis.
- It has however been found in other continents including Africa, South America, and Asia.
- Blastomyces dermatitidis as a dimorphic fungus grows as a mold, producing hyaline branched hyphae at room temperature in the laboratory and in the environment as large singly budding yeast at 37°C in the laboratory and in human tissues.
- There are four strains of Blastomyces dermatitidis that have been sequenced, namely: B. dermatitidis SLH14081, B. dermatitidis ER-3, B. dermatitidis ATCC 18188, and B. dermatitidis ATCC 26199, with the SLH-14081 strain being the most virulent pathogen isolated from samples of immunocompetent persons.
- Moreover, recent research has indicated that Blastomyces dermatitidis can cause infection in immunocompromised individuals, therefore, it has been classified as an emerging opportunistic pathogen.
Interesting Science Videos
Habitat of Blastomyces dermatitidis
- Blastomyces dermatitidis naturally live in soil and organic materials such as animal feces, plant fragments, insects remain, and dust.
- It thrives in moist, dark places that contain organic debris and a pH of 6.0.
- They are prevalent in North America, including the USA and Canada especially in Mississippi, Ohio, and Missouri valleys, where the blastomycosis infections have the highest occurrences.
- However not common in Africa, strains of Blastomyces dermatitidis have been isolated whose virulence is lower than that found in North America.
Morphology and Cultural characteristics of Blastomyces dermatitidis
- Blastomyces dermatitidis are dimorphic fungi growing both as molds that produce asexual spores known as conidia or large chlamydospores, and also as yeast at 37°C.
- Mold forms are produced when the fungi are grown in mycological cultures while the yeast forms are produced when the fungi grow in host tissues and some specialized culture media.
- Blastomyces dermatitidis grows on Sabouraud’s agar at room temperature forming white or brownish colonies.
- These colonies are made up of branched hyphae that bear spherical, ovoid, or piriform conidia (3–5 μm in diameter).
- The conidia are held by the slender terminal or lateral conidiophores.
- In SDA media, larger chlamydospores (7–18 μm) may also be produced.
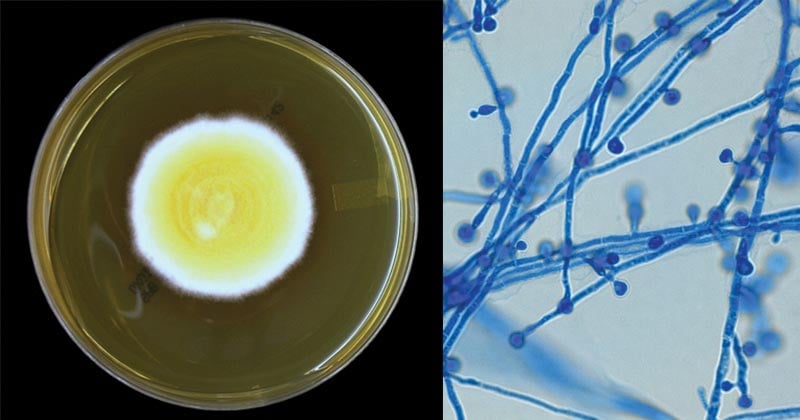
Figure: Blastomyces dermatitidis on Sabouraud Dextrose Agar (SDA) after 7 days of incubation at 30°C and Blastomyces dermatitidis conidia. Image Source: Yuri (Fun With Microbiology)
- In host tissues or culture at 37°C, Blastomyces dermatitidis grows as a thick-walled, multinucleated, spherical yeast (8–15 μm) producing single buds.
- The bud and the parent yeast are attached with a broad base, and the bud often enlarges to the same size as the parent yeast before they become detached.
- The yeast colonies are wrinkled, waxy, and soft.
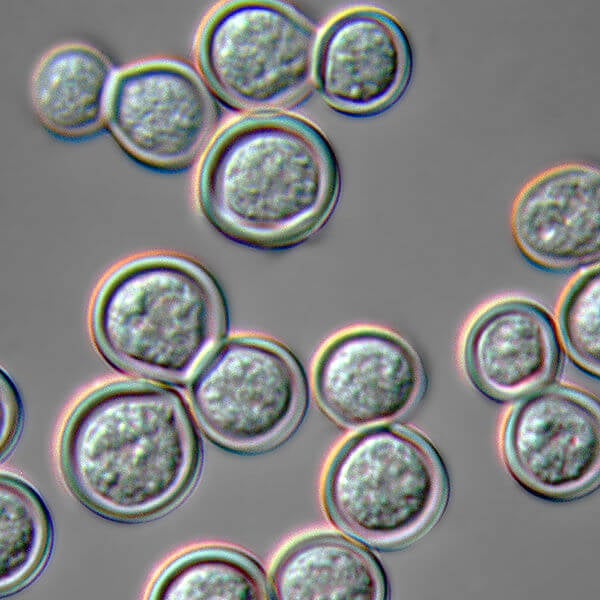
Figure: Blastomyces dermatitidis yeast form cultured on blood agar at 37 C and photographed in Nomarski Differential Interference Contrast microscopy. Image Source: Wikipedia (James Scott).
Pathogenesis of Blastomyces dermatitidis
Virulence Factors of Blastomyces dermatitidis
- The fungi are known to produce a weak Blastomyces dermatitidis antigen known as blastomycin which can be detected with complement fixation, with indications of high CF titers in patients with blastomycosis infections.
- The fungal infection also triggers the production of antibodies in antisera which can be detected to a specific B. dermatitidis antigen known as antigen A.
- These antigens have been linked to the virulence of the fungi in causing the fungal infection however there is little evidence to support the levels of virulence elicited by these antigens.
- The Fungi produces small blastospores which are light and thick-walled allowing them to be easily carried by air and therefore easily inhaled.
- The thick-walled fungal spores allow easy adherence and colonization of the host tissues
Transmission of Blastomyces dermatitidis
- Transmission os by inhalation of the Blastomyces dermatitidis spores from contaminated soil and debris, into the lungs.
- Spore exposure is airborne from excavation, construction, digging, or wood clearing.
- The fungal spores rarely infect open wounds.
- There is no human-to-human transmission or animal-to-human transmission that has been evidenced.
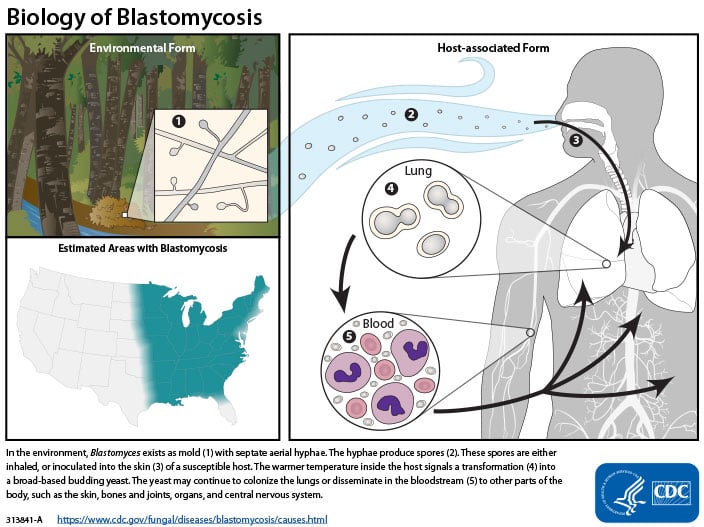
Figure: The life cycle of Blastomyces. Image Source: CDC.
Clinical Features of Blastomycosis
- The initial infection begins when blastospores are inhaled into the lungs which spread rapidly to the skin and other parts of the body.
- The most common clinical manifestation is pulmonary infiltration associated with acute lower respiratory infections including fever,
malaise, night sweats, cough, and myalgias. - Patients can also present with chronic pneumonia.
- Histological evidence shows distinct pyogranulomatous reaction with neutrophils and noncaseating granulomas.
- Dissemination is evidenced on the skin by the formation of skin lesions which can evolve to ulcerated verrucous granulomas with bordering and centralized scarring.
- The skin lesions’ borders are filled with microabscesses with sharp sloping edges.
- The disease dissemination in bones and the genitalia (prostate, epididymis, and testis) and the central nervous system may also occur.
- The disease blastomycosis occurs in three clinical forms:
- cutaneous disease
- pulmonary disease
- disseminated disease
Laboratory Diagnosis of Blastomycosis
Specimen: Sputum, pus, and tissue biopsies.
Microscopic Examination
- KOH wet mount for observation of yeast cells, which are 3-5 µm diameter or blastospores produced after culturing.
Culture Identification
- Sabouraud Dextrose Agar (SDA) forms white or brownish colonies, which produces ovoid spherical shaped spores.
- Tissue culture should produce yeast-like cells which are thick-walled, multinucleated, and spherical shaped.
Histological Examination
- Use of hematoxylin- Eosin Stain to observe for polymorphonuclear leukocytes and pyogranulomatous reaction due to neutrophilic interactions of the granuloma from the host tissues.
- Gomori’s methenamine silver stain (GMS) and periodic acid-Schiff (PAS) can readily visualize the fungus;
- GMS stains the yeast cell wall deep black and interior of the yeast cells are rose-colored, with a green background.
- PAS stains the yeast cells red with a pink background or light green, determined by the type of counterstain that is used.
- The histological stains show small yeast cells (2-10 µm in diameter) or large cells (25-40 µm in diameter) with short septate hyphae with hyaline.
Immunological Diagnosis
- Complement fixation test for detecting the blastomycin antigen; high complement fixation titers indicate the presence of Blastomyces dermatitidis antigen.
- Immunodiffusion is used for the detection of Blastomyces dermatitidis antigen A.
- Skin Test for detection of blastomycin.
- ELISA for detection of antibodies against Blastomyces dermatitidis antigen A.
Treatment of Blastomycosis
- Amphotericin B (Fungizone), itraconazole (Sporanox), or ketoconazole (Nizoral) are the drugs of choice for treatment.
- Amphotericin B should be preferred particularly in immunocompromised patients.
- Mild pulmonary blastomycosis clears spontaneously and does not require antifungal therapy.
- Surgery may be necessary for the drainage of large pulmonary abscesses along with antifungal therapies.
Prevention and Control of Blastomyces dermatitidis
- There are no Infection control issues as this disease is not spread from person to person.
- There is no vaccine available.
- There is no prophylaxis recommended.
References
- Medical Microbiology by Jawerts, 23rd Edition
- Microbiology by Prescott, 5th Edition
- Infectious Disease Advisor; Blastomycosis
- https://www.health.state.mn.us/diseases/blastomycosis/basics.html#transmission
- Drfungus: knowledge base/blastomycoses species
- https://microbewiki.kenyon.edu/index.php/Blastomyces_dermatitidis
Internet Sources
- 1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3418356/
- <1% – https://www.writework.com/essay/blastomyces-dermatitidis-and-blastomycosis
- <1% – https://www.sigmaaldrich.com/content/dam/sigma-aldrich/docs/Sigma/General_Information/2/395.pdf
- <1% – https://www.researchgate.net/publication/287438008_Blastomycosis_The_morphology_of_Blastomyces_dermatitidis_in_tissue_sections_from_African_and_American_cases_suggests_that_different_varieties_of_the_fungus_prevail_in_the_old_and_new_worlds
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3910939/
- <1% – https://www.cdc.gov/fungal/diseases/blastomycosis/symptoms.html
- <1% – https://www.brainscape.com/flashcards/mycology-6152049/packs/9479405
- <1% – https://www.alliedstemcells.com/disease-conditions/
- <1% – https://web.duke.edu/pathology/MicroCases/Microbiology_Infectious_Disease_Case_Studies.doc
- <1% – https://quizlet.com/300782626/exam-master-infectious-disease-flash-cards/
- <1% – https://quizlet.com/105249367/microbiology-chapter-15-study-questions-flash-cards/
- <1% – https://en.m.wikipedia.org/wiki/White_nose_syndrome
- <1% – https://academic.oup.com/mmy/article/47/7/745/1041939
- <1% – http://www.antimicrobe.org/f02.asp

Such a nice information. Thanks a lot. All points are well put up. Language is easy to understand.