Interesting Science Videos
What is Ancylostoma duodenale?
Ancylostoma duodenale is the most dangerous parasitic roundworm, causing serious infection in humans. It is commonly known as Old World hookworm. It is common in the tropical, subtropical, and temperate region of Asia, Africa, Europe, the Pacific Islands, and the Southern States of America. Ancylostoma duodenale (Greek ankylos—hooked; stoma—mouth) was originally described by Dubini in 1843 in Italy. The life cycle of the worm was worked out by Looss in 1898 in Egypt.
Image Source: CDC DPDx. and Wikipedia.
Systematic Position of Ancylostoma duodenale
Kingdom: Animalia
Phylum: Nematoda
Class: Secernentea
Order: Strongiloidae
Family: Ancylostomatidae
Genus: Ancylostoma
Species: Ancylostoma duodenale
Habits and Habitat of Ancylostoma duodenale
- The adult worms are endoparasitic and live in the small intestines of infected persons, mostly in the jejunum, less often in the duodenum, and infrequently in the ileum.
- The infective juveniles enter the human host percutaneously from the soil contaminated by the feces in which they abound.
- It can also be transmitted, orally, and probably transplacentally.
- They flourish under primitive conditions where people go barefoot, modern sanitary conditions do not exist and human feces are deposited on the ground.
Morphology of Ancylostoma duodenale
Adult worms
- They are small and cylindroidal in shape.
- They are pale pink or greyish white but may appear reddish-brown due to ingested blood.
- The body is curved with the dorsal aspect concave and the ventral aspect convex.
- The anterior end is somewhat narrow and bent dorsally in the same direction of general body curvature. This cervical curvature gave it the name hookworm.
- The mouth is not at the tip but directed dorsally. The prominent buccal capsule, reinforced with a hard chitin-like substance carries 6 teeth; 4 hook-like teeth ventrally, and 2 knob-like (triangular plates) or sharp lancets with a median cleft dorsally.
Male Worm
- The male worm is smaller than the female worm 8-11 mm in length and 0.4 mm thick.
- The posterior end of the male is expanded an umbrella-like known as copulatory bursa which surrounds the cloaca.
- The copulatory bursa consists of 3 lobes; 1 dorsal and 2 lateral. Each lobe is supported by 13 fleshy chitinous rays, 5 each in lateral lobes and 3 in dorsal lobe: one dorsal and two extradorsal rays. The dorsal ray is partially divided at the tip and each division is tripartite.
- The pattern of the rays helps in distinguishing between different species.
- There are 2 long retractile bristle-like copulatory spicules, the tips of which project from the bursa.
Female worm
- The female worm is larger, 10 to 13 mm long and 0.6 mm thick.
- Its hind end tapers bluntly in a short post-anal tail.
- The vulva opens ventrally at the junction of the middle and posterior thirds of the body.
- The vagina leads to two intricately coiled ovarian tubes which occupy the hind and middle parts of the worm.
- During copulation, the male attaches its copulatory bursa to the vulva.
- The copulating pair, therefore, presents a Y-shaped appearance.
- Sexes are easily differentiated by their size, the shape of the posterior end, and the position of the genital opening.
Eggs
- Oval or elliptical, measuring 60 μm by 40 μm.
- Colorless, not bile stained.
- Surrounded by a thin transparent hyaline shell membrane.
- Floats in a saturated salt solution.
- When released by the worm in the intestine, the egg contains an unsegmented ovum.
- Freshly-excreted eggs contain a developing embryo in the early stages of cleavage (2-8 cells).
- There is a clear space between the segmented ovum and eggshell.
Life cycle of Ancylostoma duodenale
- The life cycle of Ancylostoma duodenale is completed in a single host, hence it is called monogenetic.
- Definitive host: Humans are the only natural host.
- No intermediate host is required like other helminths.
- Infective form: Third stage filariform larva
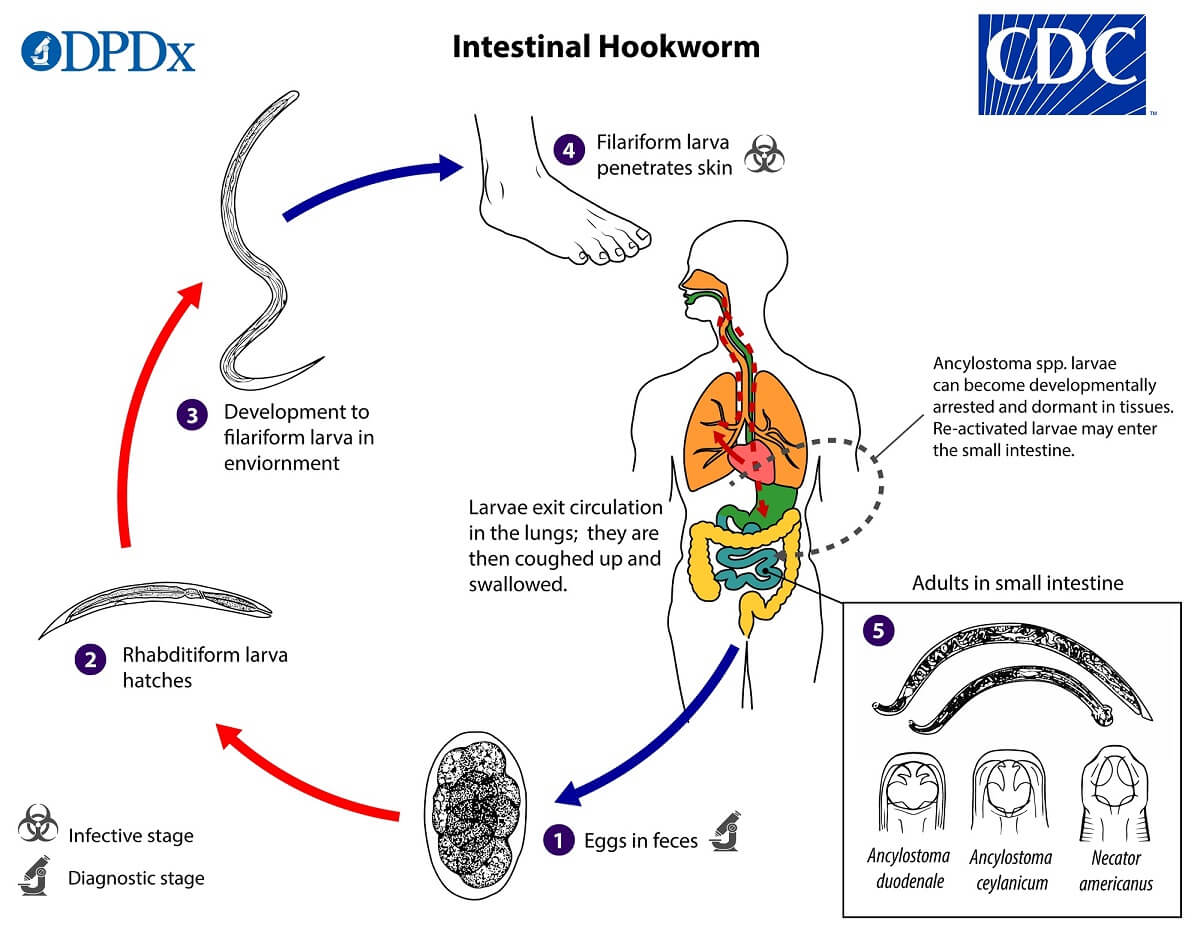
Figure: The life cycle of Ancylostoma duodenale. Image Source: CDC DPDx.
a. Copulation and fertilization
- Copulation occurs in the host’s intestine.
- During the process of copulation, the copulatory brusa of males is applied to the vulva of females, and sperms are transferred.
- Fertilization occurs in seminal receptacles.
b. Egg laying
- The female worm lays eggs in the intestine of the host with approximately 28,000eggs daily.
- The eggs containing segmented ova with 4 blastomeres are passed out in the feces of the infected person.
- Eggs freshly passed in feces are not infective for humans.
c. Development in soil
- A. duodenale hookworm eggs hatch in a warm, moist and shady environment in about 48 hours, giving rise to first-stage juvenile or rhabditiform larvae which are about 250µmin in length and feeds on organic material and bacteria.
- After about seven days, the larvae cease feeding and moults twice to become infective third-stage juvenile or filariform larvae.
- Filariform larva is about 500–600 μm long, with a sharp-pointed tail. The filariform larva are non-feeding. They can live in the soil for 5–6 weeks, with their heads waving in the air, waiting for their hosts. They can also ascend on blades of grass or other vegetation, being carried in capillary water films on their surface. Direct sunlight, drying, or saltwater can kill the larva.
- The time taken for the development from eggs to filiform larvae is on average 8 to 10 days.
d. Mode of infection
- The transmission occurs when third-stage infective filariform larvae come into contact with skin.
- The anterior end of larvae is equipped with oral spears which enable it to penetrate the skin of a potential human host.
- The larvae generally penetrate the cutaneous tissues, most often those of the hands, feet, arms, and legs due to exposure and usually through hair follicles or abraded skin. Their penetration is generally accompanied by severe dermatitis called ‘Ground itch’ characterized by ulceration of skin about wounds.
- Rarely, an infection may take place by the oral route, the filariform larva being carried on contaminated vegetables or fruits. The larvae may penetrate the buccal mucosa to reach the venous circulation and complete their migration via the lungs.
- Transmammary and transplacental transmission has been also reported for Ancylostoma.
e. Larval migration
- Following skin penetration, the larvae enter subcutaneous venules and lymphatics to gain access to the host’s afferent circulation.
- Ultimately, they enter the pulmonary capillaries where they penetrate into the alveolar spaces, ascend the brachial tree to the trachea,
traverse the epiglottis into the pharynx, and are swallowed into the gastrointestinal tract. - During migration or on reaching the esophagus, they undergo third molting.
- They feed, grow in size, and undergo a fourth and final moulting in the small intestine and develop the buccal capsule, by which they attach themselves to the small intestine and grow into adults.
- Adult worms exhibit considerable variation in size, and female worms are usually larger than males.
- In about 3 to 4 weeks they become sexually mature to repeat the life history again.
- The normal life span of adult worms in the human intestine has been estimated differently by different workers; generally believed to be 3 to 4 years.
Read Also: Plasmodium vivax- Life Cycle in Man and in Mosquito
Pathogenicity of Ancylostoma duodenale
- Pathogenicity is fairly extensive involving the skin, lungs, and small intestine.
- Some people can develop an Ancylostoma infection without any symptoms, while others may have mild to severe symptoms. There are 3 phases: invasion, migration, and establishment in the intestine.
- During the invasion stage, the filariform larvae penetrate the skin results in a hypersensitivity reaction causing local irritation, intense itchiness, and vesicular rash lesions that are called ground itch.
- One to two weeks following skin invasion, hookworm larvae travel through the vasculature and enter the lungs, where they can uncommonly result in pneumonitis.
- The pulmonary symptoms that may develop are usually mild and transient, consisting of a dry cough, sore throat, wheezing and slight fever. The pulmonary symptoms are more pronounced and of longer duration
- The acute symptomatic disease may also result from oral ingestion of A. duodenale larvae, referred to as the Wakana syndrome, which is characterized by nausea, vomiting, pharyngeal irritation, cough, dyspnea, and hoarseness.
- There is an appearance of eosinophilia with the development of adult hookworms in the intestine. The major pathology of infection, however, results from the intestinal blood loss that results from adult parasite invasion and attachment to the mucosa and submucosa of the small intestine.
- Usually, only moderate and high-intensity infections in the gastrointestinal tract produce clinical manifestations, with the highest intensity infections occurring most often in children, although even in low-intensity infections, initial symptoms may include dyspepsia, nausea, and epigastric distress.
- A. duodenale may also result in acute enteritis with uncontrollable diarrhea and foul stools that may last indefinitely.
- Chronic infection in the intestine results in iron-deficiency anemia, accompanied by the loss of appetite, abdominal discomfort, and malnutrition due to protein deficiency. This can cause physical and cognitive impairment.
- Uncommonly, there may be constipation or diarrhea with occult blood in the stools or frank melena, especially in children; there may also be an urge to eat soil (pica).
- Overwhelming infection may cause listlessness, coma, and even death, especially in infants under one year of age.
Diagnosis of Ancylostoma duodenale
Direct methods
- Demonstration of characteristic oval segmented eggs in feces by direct wet microscopy or by formalin-ether concentration methods is the best method of diagnosis. In stool samples examined 24 hours or more after collection, the eggs may have hatched and rhabditiform larvae may be present. These have to be differentiated from Strongyloides larvae.
- Egg counts give a measure of the intensity of infection. Modified Kato- Katz smear technique is a useful method for quantitative
estimation of eggs in the stool. - Stool cultures (fecal sample smear on moistened filter paper in a closed tube for a few days)(Harada-Mori technique) to demonstrate third-stage filariform larvae A. duodenale larvae have long buccal cavities and smaller genital primordium, whereas Strongyloides have short buccal cavities.
Indirect methods
- Blood examination reveals microcytic, hypochromic anemia, and eosinophilia.
- Stool examination may show occult blood and Charcot -Leyden crystals
- Chest radiography will usually be negative during the pulmonary phase of larval migration, although sputum examination may reveal erythrocytes, eosinophils, and rarely migrating larvae.
- Radiographic findings include intestinal hypermotility, proximal jejunal dilatation, and coarsening of the mucosal folds.
- Several immunoserological tests have been developed to detect host antibodies against A. duodenale antigens, but they generally do not discriminate between patent or previous infections.
- Recent research has focused on the development of DNA-based tools for diagnosis of infection, specific identification of hookworm, and analysis of genetic variability within hookworm populations because hookworm eggs are often indistinguishable from other parasitic eggs, PCR assays could serve as a molecular approach for accurate diagnosis of hookworm in the feces.
Treatments and prophylaxis of Ancylostoma duodenale
- Effective drugs: A single dose of albendazole(400mg) or mebendazole(500mg) or a 3-day dose of albendazole, mebendazole, or pyrantel pamoate((11 mg/kg × 3 days).
- For kids, pregnant women, or others who develop anemia as a result of hookworm infection, health care providers will often prescribe an iron supplement to overcome hemoglobin due to anemia.
- Prevention of soil pollution with feces and proper use of sanitary latrines.
- Use of footwear to prevents entry of larva through the skin of the foot. Gloves give similar protection to the hands of farmworkers.
- Treatment of patients and carriers, preferably all at the same time, limits the source of infection.
References and Sources
- Kotpal RL. 2017. Modern Text Book of Zoology- Invertebrates. 11th Edition. Rastogi Publications.
- Jordan EL and Verma PS. 2018. Invertebrate Zoology. 14th Edition. S Chand Publishing.
- Aziz MH, Ramphul K. Ancylostoma. [Updated 2020 May 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507898/
- https://www.verywellhealth.com/hookworm-overview-4176230
- https://web.stanford.edu/group/parasites/ParaSites2009/PinedaANDYang_Hookworm/PinedaANDYang_Hookworm.htm
- 3% – https://europepmc.org/article/MED/29939675
- 3% – http://www.parasite.org.au/para-site/text/ancylostoma-necator-text.html
- 2% – https://otrosbichos.blogspot.com/2012/09/phylum-nematoda-anquilostomiasis.html#!
- 2% – http://dictionary.sensagent.com/Hookworm/en-en/
- 1% – https://www.symptoma.com/en/ddx/diarrhea+dry-cough
- 1% – https://www.sciencedirect.com/topics/nursing-and-health-professions/hookworm-infection
- 1% – http://jumed16.weebly.com/uploads/8/8/5/1/88514776/parasitology_introduction_protozoa_helmenths_introduction___.pdf
- <1% – https://www.scribd.com/document/103703481/Medical-Parasitology
- <1% – https://www.sciencedirect.com/topics/medicine-and-dentistry/fasciolopsiasis
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3186755/
- <1% – https://www.healthhype.com/human-intestinal-worms-symptoms-pictures-treatment.html
- <1% – https://study.com/academy/lesson/transmission-prevention-of-fungal-disease-infection.html
- <1% – https://quizlet.com/79512049/laboratory-methods-flash-cards/
- <1% – https://en.wikipedia.org/wiki/Orally_transmitted_diseases
- <1% – https://en.wikipedia.org/wiki/Human_embryogenesis
- <1% – https://cmr.asm.org/content/15/4/595
