- Before a microbe or parasite can invade the host and cause infection, it must first attach to and penetrate the surface epithelial layers of the body.
- Organisms gain entrance into the body by active or passive means. For example, actively, they might burrow through the skin, while passively be ingested in food, inhaled into the respiratory tract or penetrate through an open wound.
- Whatever the point of entry, they have to pass across the external physical barriers that insulate the body’s interior from the pathogens of the exterior world.
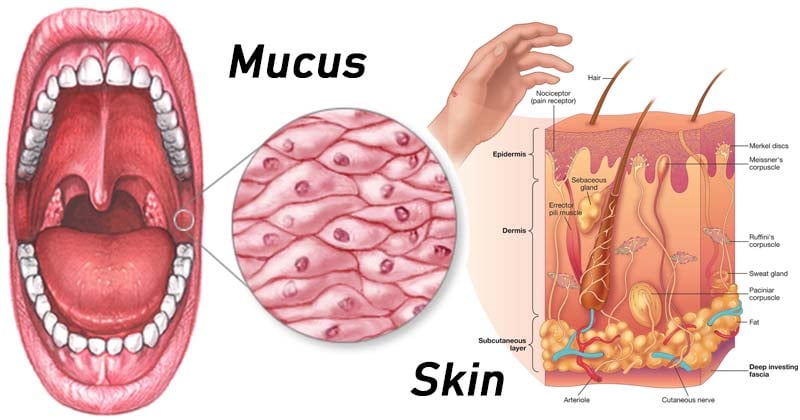
- These barriers called anatomical barriers include the skin and the tissue surfaces connected to the body’s openings called mucous epithelial layers (mucous membranes) that line the respiratory, gastrointestinal, and urogenital tracts along with the ducts of secretory glands.
- Skin and other mucous membrane provide a kind of living “plastic wrap” that encases and protects the inner domains of the body from infection.
- In addition, they contribute to physical and mechanical processes that help the body shed pathogens and also generate active chemical and biochemical defenses by synthesizing and deploying molecules that have or induce antimicrobial activity.
Interesting Science Videos
The Skin
The skin is the largest organ in the body and a critical anatomic barrier against pathogens for the following reasons:
- The epidermal layer of the skin is composed largely of specialized epithelial cells called keratinocytes composed of waterproofing protein called keratin. Keratin is not easily degraded by many microorganisms which makes skin penetration difficult.
- The relatively dry skin with high salt concentration in drying sweat is inhibitory or lethal to many microbes.
- Epithelial cells also produce defensins and cathelicidins to kill microbes.
- Skin secretes sebum, which prevents growth of many microorganisms. Sebum consists of lactic acid and fatty acids that maintain the pH of the skin between 3 and 5 which is inhibitory to many bacteria.
- Additionally, the outer surface of the skin consists of dead cells that are continuously shed causing the organisms to dislodge and also preventing viruses that require living cells for their metabolism.
- Keratinocytes also secrete a number of cytokines that may function to induce a local inflammatory reaction.
- Scattered among the epithelial-cell matrix of the epidermis are Langerhans cells which are skin-resident dendritic cells that internalize antigen by phagocytosis. These Langerhans cells undergo maturation and migrate from the epidermis to regional lymph nodes, where they function as potent activators of naive T cells.
Besides these roles in non-specific defence mechanism, the skin also has following functions:
- The epidermis also contains intraepidermal lymphocytes, which are predominantly T cells which are believed to play a role in combating infections that enter through the skin.
- The underlying dermal layer of the skin also contains scattered lymphocytes, dendritic cells, monocytes, macrophages, and may even include hematopoietic stem cells.
- Most skin lymphocytes appear to be either previously activated cells or memory cells, many of which traffic to and from local, draining lymph nodes that coordinate the responses to pathogens that have breached the skin barrier.
The Mucous Membrane
- In place of skin, the respiratory, gastrointestinal, and urogenital tracts and the ducts of the salivary, lacrimal, and mammary glands are lined by strong barrier layers of mucous epithelial cells.
- A number of non-specific defence mechanisms act to prevent entry of microorganisms through mucous membranes.
- Mucus is a viscous fluid secreted by epithelial cells of mucous membranes that entraps invading microorganism. Moreover, the epithelial cells themselves are stitched together by tight junctions that prevent pathogens from squeezing between them to enter the body.
- Saliva, tears and mucous secretions tend to wash away potential invading microorganisms thereby preventing their attachment.
- These secretions also contain antibacterial and antiviral substances that kill pathogens.
Mucus contains lysozyme to degrade bacterial peptidoglycan, antibody IgA that prevents microbes from attaching to mucosal cells and traps them in the mucous, lactoferrin to bind iron and keep it from from being used by microbes and lactoperoxidase to generate toxic superoxide radicals that kill microbes.
- Like the skin, the mucous membrane constantly sloughing cells to remove microbes that have attached to the mucous membranes.
- In lower respiratory tract, mucous membrane is covered with cilia which are hair like protrusions of epithelial cells. They move mucus and trapped particles out of the body.
- The mucosa-associated lymphoid tissue (MALT) which lies beneath the mucosal membrane contains Langerhans’ cells which act as potent activators of naïve T cells.
- Besides these roles in non-specific defence mechanism, intraepithelial T-lymphocytes and B-1 lymphocytes are associated with the epidermis and the mucosal epithelium. These cells recognize microbes common to the epidermis and mucous membranes and start immediate adaptive immune responses against these commonly encountered microbes.
References
- Brooks, G. F., Jawetz, E., Melnick, J. L., & Adelberg, E. A. (2010). Jawetz, Melnick, & Adelberg’s medical microbiology. New York: McGraw Hill Medical.
- Lydyard, P.M., Whelan,A.,& Fanger,M.W. (2005).Immunology (2 ed.).London: BIOS Scientific Publishers.
- Owen, J. A., Punt, J., & Stranford, S. A. (2013). Kuby Immunology (7 ed.). New York: W.H. Freeman and Company.
- Parija S.C.(2012). Textbook of Microbiology & Immunology.(2 ed.). India: Elsevier India.
- https://bio.libretexts.org/TextMaps/Microbiology/Book%3A_Microbiology_(Kaiser)/Unit_5%3A_Innate_Immunity/11.3%3A_Immediate_Innate_Immunity/11.3C%3A_Anatomical_Barriers_to_Infection%2C_Mechanical_Removal_of_Microbes%2C_and_Bacterial_Antagonism_by_Normal_Body_Microbiota.

Wow this is amazing notes its really helpful please