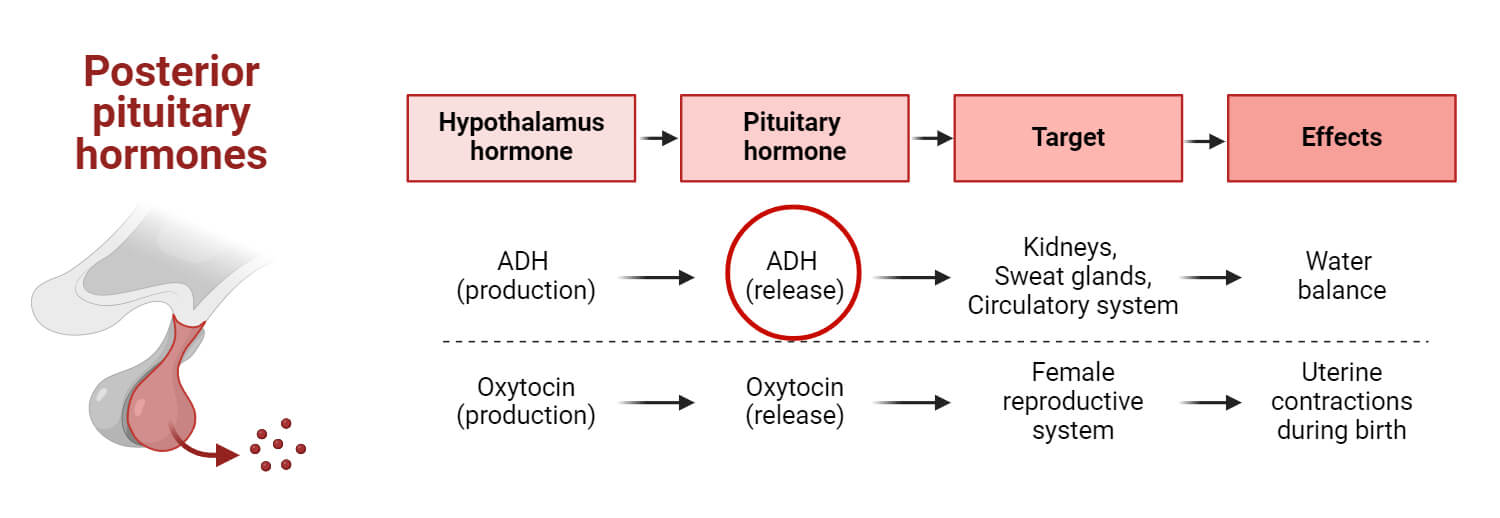
Antidiuretic hormone (ADH) or vasopressin or arginine vasopressin is a peptide hormone synthesized by supraoptic and paraventricular nuclei in the hypothalamus and is stored in the pituitary gland.
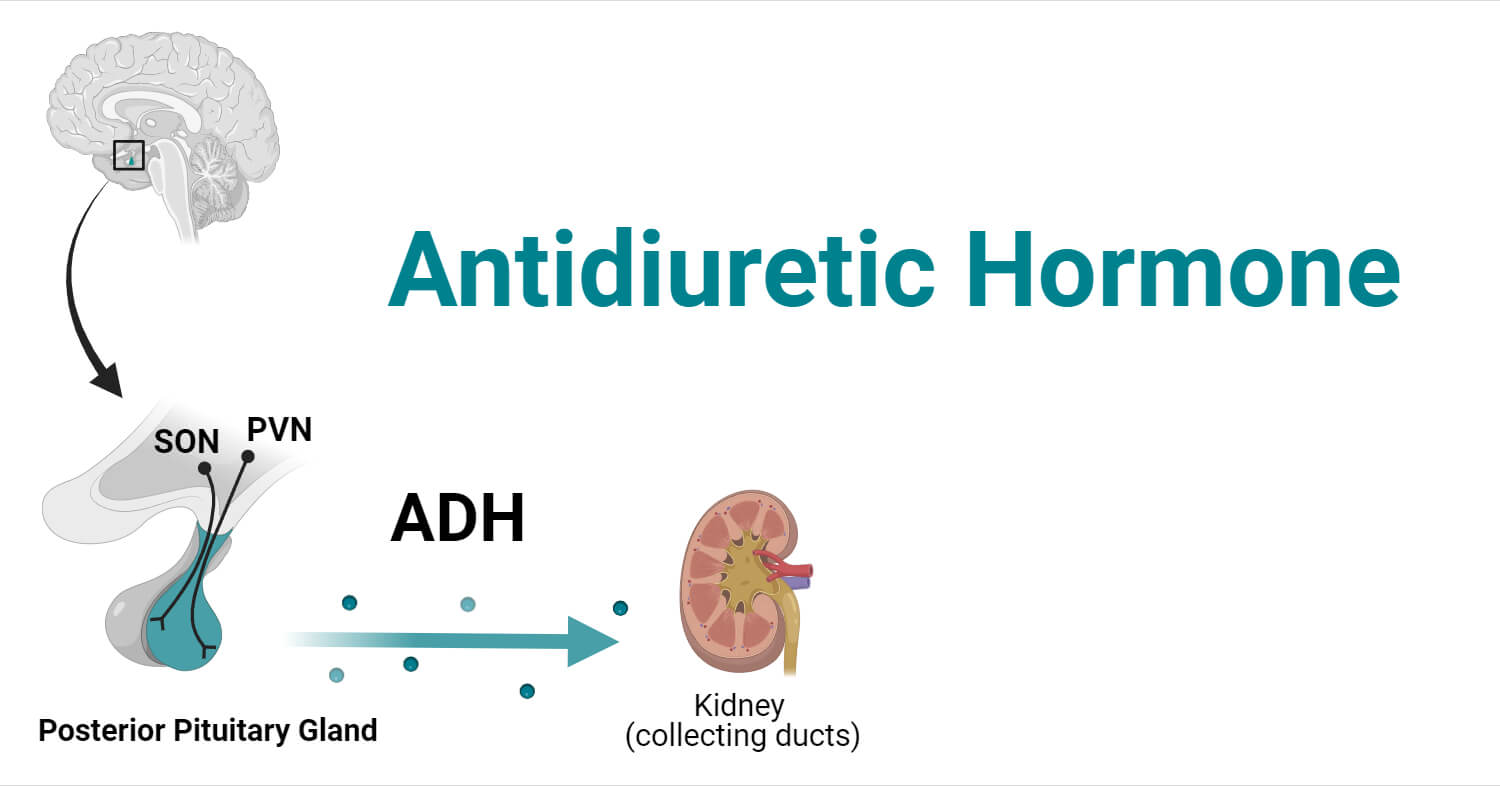
Even synthesized in the hypothalamus, the hormone is transported to the neurohypophysis (posterior pituitary gland) through nerve cells which are then released into the bloodstream through neurohypophysial capillaries by the process of exocytosis involving calcium.
ADH is called vasopressin due to its vasopressor response to pharmacological doses. Most of the animals along with humans are present with arginine vasopressin whereas pig has lysine instead of arginine.
Interesting Science Videos
Physiological functions of Antidiuretic Hormone (ADH)
Vasopressin is responsible for:
- Regulation of the body’s osmotic balance.
- Maintaining blood pressure by acting on the kidney and blood vessels.
- Maintaining blood volume.
- Homeostasis (sodium homeostasis).
- Maintaining appropriate cellular functions.
- Maintaining the water content of the tissue by regulating the concentration of urine excretion from the kidneys.
- Also, controls bleeding abnormalities and septic shocks.
Role of ADH in homeostasis
Homeostasis refers to a self-regulating process with the help of which organisms can attain internal stability by adjusting to changes in external environmental conditions.
- Fluid and electrolyte balance
ADH regulates the body’s fluid concentration by controlling the reabsorption of water from the kidneys.
- Osmoregulation
ADH helps in osmoregulation keeping the concentration of body fluids in a narrow range.
- Renal tubule permeability
ADH is responsible for increasing permeability.
- Prevention of Dehydration
ADH is responsible for maintaining appropriate levels in the body by reabsorbing water and hence preventing excessive water loss from the body.
- Regulation of Blood Pressure
ADH directly regulates the blood pressure by maintaining the blood volume in the body.
- Integration with other hormones
ADH works in conjunction with other hormones such as aldosterone for electrolytic balance in the body. This collaborative regulation of hormones contributes to the overall homeostasis.
Factor Affecting ADH release:
Major two factors include:
Osmolarity
- Hyper-osmolarity/ increase in osmotic pressure: increase in ADH secretion
- Hypo-osmolarity/ decrease in osmotic pressure: decrease in ADH secretion
Volume
- Hypervolemia/ increase in blood volume: Inhibition of ADH secretion
- Hypovolemia/ depletion of blood volume: Increase in the secretion.
Note:
Hypoosmotic condition (along with hypovolemia)- increase in ADH secretion
Hyperosmotic condition (along with hypervolemia): reduced secretion of ADH
Other factors promoting ADH secretion include:
- Angiotensin II
- Pain
- Nausea
- Exercise
- Hypoglycemia
- Nicotine
- Steroids
- Opiates
Other factors inhibiting ADH secretion include:
- Ethanol: its inhibitory effect increases diuresis
- Alpha-adrenergic agonists
- Atrial natriuretic peptide released in response to increased blood pressure
ADH regulates majorly by:
- Altering the amount of reabsorption of water by the kidney
- In the presence of ADH, aqua proteins in the distal convoluted tubule and collecting duct are expressed increasing reabsorption.
- Increased concentration of ADH causes blood vessels to constrict increasing blood pressure.
Receptors
- Osmoreceptors
Located outside the blood-brain barrier in the organum vasuculom of the lamina terminalis (OVLT) and subfornical organ and sensitive to changes in osmotic pressure. It can directly detect blood osmolarity due to the lack of blood-brain barrier.
- Baroreceptors
Located in the left atrium, carotid arch, and aortic arc and is sensitive to changes in blood volume, or blood pressure. With the increase in blood volume, the tissues of the carotid sinus and left atrium are stretched, which stimulates the nerve in baroreceptors. The signals are transmitted to ADH-producing cells, inhibiting their secretion.
On a decrease in blood pressure, the signals are transmitted to the vagus nerve stimulating the release of ADH. With the secretion of ADH, reabsorption of water in the kidney increases, and it causes vasoconstriction.
Mechanism of Action
- The water content in the body influences the volume of the blood and the blood pressure. Also, particles such as sodium, potassium, carbon dioxide, and chlorine are responsible for maintaining a stable environment inside the body.
- The imbalances in the water level or the concentration of these particles are detected by osmotic receptors and baroreceptors which send signals to the kidney for the maintenance of water levels and regulation of thirst.
- The osmoreceptors in the hypothalamus are sensitive to changes in the osmolarity of the plasma in the cells. It is directly associated with the production of vasopressin.
- Increase in osmolarity/ low blood volume
Causes of Hyperosmolarity/ Hypovolemia
- Insufficient drinking of water.
- Losing more water compared to consumed due to heavy sweating or diarrhea.
- Consumption of highly salty foods rich in sodium and chloride ions.
Mechanism and Regulation
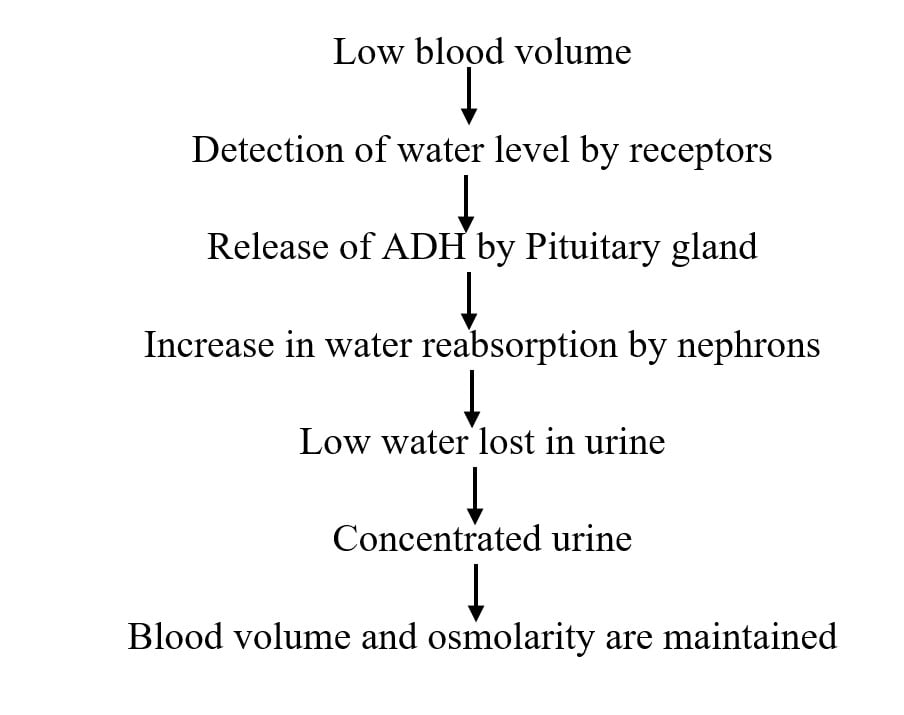
- Dehydration or low blood volume stimulates the osmoreceptors which trigger the release of vasopressin from neurohypophysis.
- There are two major ADH receptors: V1 and V2 receptors. V1 receptors are present in blood vessels for vasopressor action whereas V2 receptors (G-protein linked cell surface receptor) are in the basolateral membrane of collecting tubules in the kidney.
- With the release of ADH, activation of the V2 (AVPR2) receptor occurs in collecting tubule activating adenyl cyclase, and hence the formation of cAMP.
- This cAMP activates PKA initiating a phosphorylation cascade.
- Here, the vesicular trafficking mediates the insertion and removal of aqua porin II in the apical membrane. This aquaporin-2 (AQP 2), vasopressin-responsive water channel, during high osmolarity or decreased blood volume, allows the rapid passive moment of water guided by the osmolar gradient inside the cell from the kidney.
- This maintains the water level and blood volume in the body, in turn balancing the osmolarity. Here the volume of urine is reduced making the urine concentrated, rich in sodium chloride and other particles.
- With the release of ADH, the permeability of the collecting duct to urea also increases. As more water is being reabsorbed, urea becomes highly concentrated, generating a high gradient for the passive movement of urea out of the filtrate.
- Reabsorption of urea with water ensures that the water potential at the interstitial space is kept lower than the filtrate, so water continues to be reabsorbed.
- High concentrations of ADH also cause vasoconstriction of peripheral blood vessels, ensuring that blood pressure does not drop too low. Restoring the blood osmolarity is only fully achieved by drinking more water.
- The hypothalamus also activates the thirst center in response to low blood water potential, increasing the urge to drink water. Following the restoration of the blood water potential, osmoreceptors send fewer impulses to the hypothalamus, and secretion of ADH is reduced. This is an example of negative feedback.
- According to recent studies, the mutations aquaporin 2 gene and vasopressin receptor gene are responsible for causing Diabetes insipidus.
- The decrease in the blood volume or blood pressure is detected by the large blood vessels and the receptors present in the heart stimulate the release of ADH.
- ADH also has a second action on vascular smooth muscle.
- ADH binds to V receptors acting on vascular smooth muscle activating G protein.
- Activated G protein activates phospholipase C (PLC), resulting in the production of inositol triphosphate (IP-3) as well as diacylglycerol (DAG) from the cell membrane.
- The IP3 produced stimulates the release of intracellular calcium from the endoplasm reticulum. DAG and calcium activate protein kinase C (PKC), which, like PKA, results in a signaling phosphorylation cascade.
- The net effect of this signaling cascade is a contraction of vascular smooth muscle leading to increases in total peripheral resistance and thus increases in blood pressure.
- The increase in the concentration of salts in the bloodstream also controls the secretion of ADH, which is identified by special nerve cells in the hypothalamus.
- If the levels of ADH are higher, the water is retained by the kidneys in the body. When excess ADH is released when not required, the blood gets diluted due to excess water retention.
- The salt concentration in the blood thus decreases. High levels of ADH may be caused due to the side effects of drugs, lung diseases, etc. Increased ADH is associated with leukemia, lymphoma, bladder cancer, brain cancer, etc.
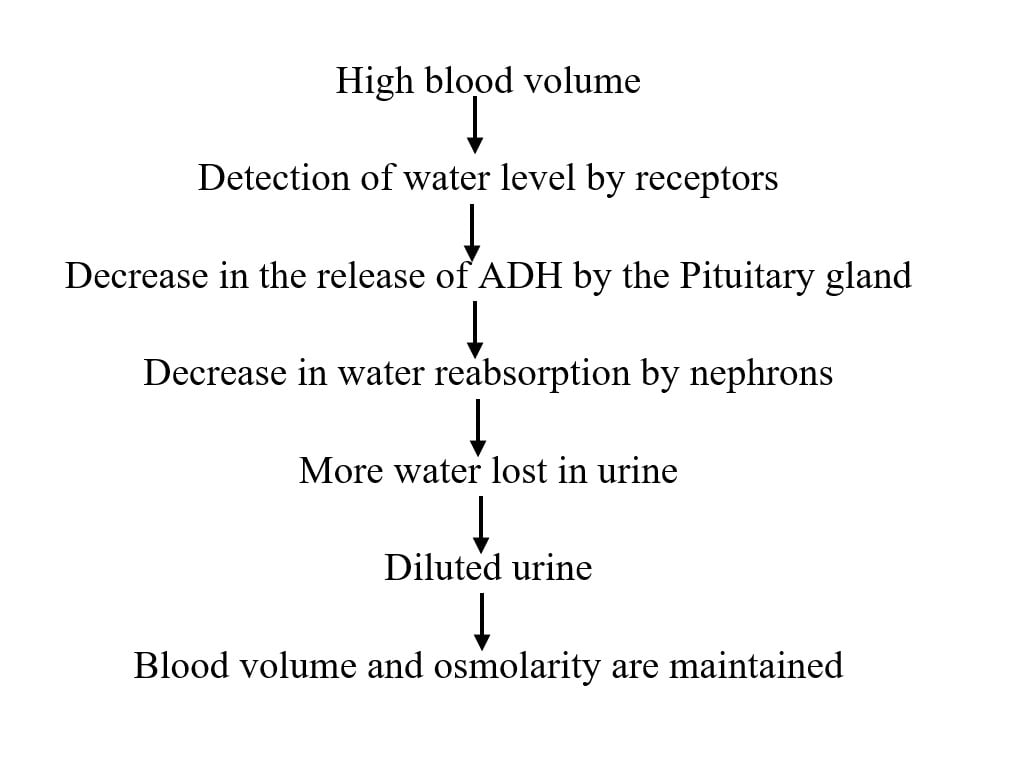
- Decrease in osmolarity/ high blood volume
Causes of Hypo-osmolarity/Hypervolemia
- Drinking too much water
- Not having sufficient salt and electrolytes in the diet to replace those lost in metabolism and excretions.
- Fluid replacement therapy causes fluid overload due to excessive infusion of too much fluid. (usually to patients in hospitals)
Mechanism:
- Overhydration, increased blood volume, or decreased osmolarity due to various above-mentioned reasons, osmoreceptors are inhibited and decrease the secretion of osmoreceptors. The receptors are inhibited to prevent the release of ADH.
Interaction of ADH and aldosterone hormone and angiotensin II
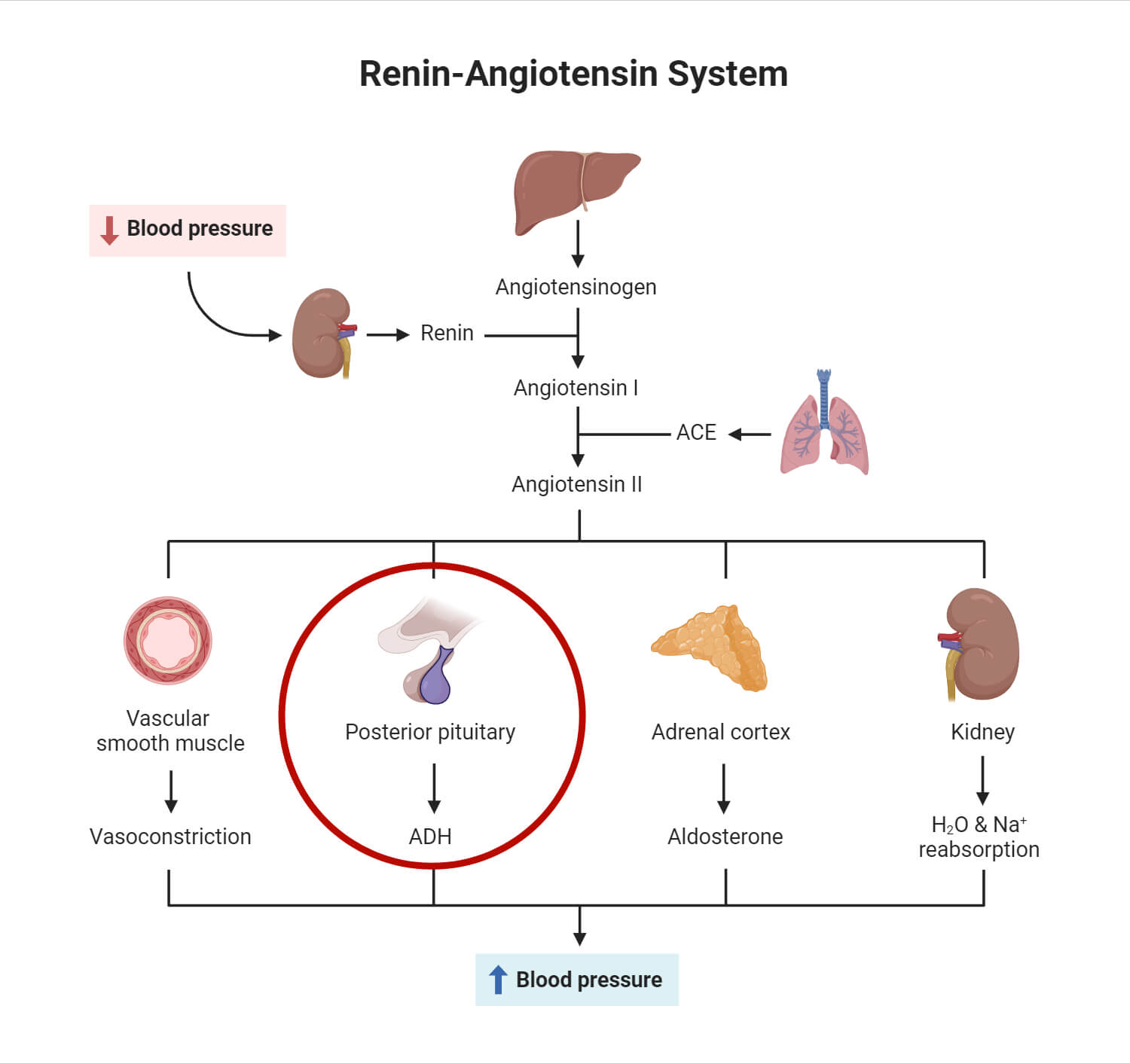
Aldosterone is responsible for retaining Na+ and water in the bloodstream. Both ADH and aldosterone regulate water retention in the DCT and collecting duct. On a decrease in blood pressure, the kidney releases a hormone called renin which causes the release of Angiotensin II, causing vasoconstriction and corelease of ADH and aldosterone. ADH and aldosterone are released simultaneously to increase blood pressure or blood volume. Here, ADH is released majorly during dehydration or high osmolarity. Similarly, the release of aldosterone occurs in low Na+ and K+ states. All three of them work to maintain the proper blood volume and blood pressure in the body.
Impact of ADH imbalance on health/ Clinical conditions Related to ADH
Test for ADH
Sample: blood sample withdrawn from venipuncture method
Normal ADH level: 1-5 picograms per milliliter (pg/ml); may differ slightly with laboratories.
ADH Deficiency
Causes:
- Compulsive water drinking
- Low blood serum osmolarity: Refers to decreased concentration of particles in blood.
- Central Diabetes insipidus: Metabolism disorder, Diabetes insipidus sometimes causes ADH deficiency
Symptoms:
- Polyuria/Excessive urination: An excessive amount of water is excreted in the form of urine.
- Polydipsia/Thirst sensation: An increase in ADH levels triggers thirst as a response to a decrease in water level in the body, dehydration, or elevated blood osmolarity.
- Low blood pressure: An increase in the volume of urine causes dehydration ultimately lowering the blood pressure.
- Damage in the pituitary gland: Significant lowering of ADH levels can also lead to damage to the hypothalamus or pituitary gland.
- Insufficient production of ADH may lead to a condition known as Diabetes insipidus. It is a condition where the body makes a very low amount of anti-diuretic hormone which occurs usually due to inflammation in the pituitary gland or hypothalamus, also sometimes due to tumor or trauma. Diabetes insipidus results in increased thirst and pale urine production leading to dehydration as well.
Excessive ADH secretion/ Syndrome of inappropriate antidiuretic hormone (SIADH)
It is the condition where the hypothalamus synthesizes too much ADH.
Causes:
Excessive ADH levels are associated with conditions such as
- Leukemia
- Lymphoma
- Lung cancer
- Pancreatic cancer
- Bladder cancer
- Brain cancer
- Guillain Barre Syndrome
- Epilepsy
- Cystic fibrosis
- Tuberculosis
- HIV/AIDS
- Brain trauma
- Psychosis
- Medication such as anticonvulsants, and chemotherapy drugs.
- Nephrogenic diabetes insipidus– ADH is sufficient in the body, but the kidney cannot respond to it.
Symptoms
- Hyponatremia: Excessive ADH can decrease blood sodium levels resulting in neurological symptoms and various complications
- Cramping
- Nausea and vomiting
- Loss of Appetite
- Seizures
- Coma
To sum up in a table:
| Plasma osmolarity | Water concentration | ADH level | Water reabsorption in the kidney | Urine concentration |
| High concentration | Low | Increases | Increase | High |
| Low concentration | high | Decreases | Decrease | Low |
References
- Antidiuretic Hormone. Mount Sinai. Retrieved from
https://www.mountsinai.org/health-library/tests/antidiuretic-hormone-blood-test. Accessed on 8th January 2023.
Antidiuretic Hormone. Byju’s Biology.Retrieved from https://byjus.com/biology/adh-hormone/. Accessed on 10th January 2023. - ADH. StudySmarter. Retrieved from https://www.studysmarter.co.uk/explanations/biology/responding-to-change/adh/. Accessed on 8th January 2023.
- Antidiuretic Hormone. BBC. Retrieved from https://www.bbc.co.uk/bitesize/guides/zgh2xsg/revision/3. Accessed on 8 January 2023. Accessed on 12th January 2023.
- Brandis, K. Antidiuretic Hormone. LibreTextsMedicine. Retrieved from https://med.libretexts.org/Bookshelves/Anatomy_and_Physiology/Fluid_Physiology_(Brandis)/05%3A_Control_of_Water_Metabolism/5.07%3A_Antidiuretic_Hormone. Accessed on 10th January 2023.
- Florjanczyk, U., Narayanan, J., McKenney, E. Antidiuretuc Hormone. Osmosis from ELSEVIER. Retrieved from https://www.osmosis.org/learn/Antidiuretic_hormone. Accessed on 8th January 2023.
- SIADH. Cleveland Clinic. Retrieved from https://my.clevelandclinic.org/health/diseases/23976-siadh-syndrome-of-inappropriate-antidiuretic-hormone-secretion. Accessed on 11th January 2023.
- Cuzzo, B., Padala S. A., Lappin. S.L. (2023) Physiology, Vasopressin. IN StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK526069/#:~:text=ADH%20is%20an%20important%20hormone,of%20effective%20arterial%20blood%20flow.
(2009). Vasopressin (VP) or Antidiuretic Hormone (ADH). In: Binder, M.D., Hirokawa, N., Windhorst, U. (eds) Encyclopedia of Neuroscience. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-29678-2_6236. Accessed on 12th January 2023. - Antidiuretic Hormone. July 2021. You and Your Hormones. Retrieved from https://www.yourhormones.info/hormones/anti-diuretic-hormone/. Accessed on 9th January 2023.
- Pietrangelo, A. (23 December 2022). Syndrome of Inappropriate Antidiuretic Hormone (SIADH). Healthline. Retrieved from https://www.healthline.com/health/syndrome-of-inappropriate-antidiuretic-hormone#diagnosis. Accessed on 12th January 2023.
- Khanna, A. (22 August 2023). Antidiuretic Hormone. TeachMePhysiology. Retrieved from https://teachmephysiology.com/urinary-system/regulation/antidiuretic-hormone/. Accessed on 10th January 2023.
- Syndrome of inappropriate ADH secretion (5 December 2023). MedlinePlus. Retrieved from https://medlineplus.gov/ency/article/000314.htm. Accessed on 10th January 2023.
