Staphylococcal food poisoning (SFP) is one of the most probably occurring food-borne diseases which cause intoxication from the consumption of food containing preformed staphylococcal enterotoxins (SEs). Staphylococcal enterotoxins are mainly produced by Staphylococcus aureus which is enterotoxigenic strains of coagulase and Thermo nuclease (TNase) positive staphylococci. While occasionally SFP causing coagulase-negative staphylococcus species are Staphylococcus intermedius, Staphylococcus hyicus, Staphylococcus lutrae, Staphylococcus agnetis, and Staphylococcus schleiferi subsp. coagulans. Similarly, one of the exceptional cases of TNase negative coagulase-positive staphylococci is Staphylococcus delphini. The typical characteristics of S. aureus (i.e., ferments mannitol and are acetoin positive) are what it differs from other staphylococcal species.
Interesting Science Videos
Source of contamination of Staphylococcal food poisoning
- S. aureus is a gram-positive, non-sporing pathogenic food-borne bacterium that can be isolated from a wide range of environments (soil, water, and air).
- The main source of enterotoxin contamination is associated with food handlers carrying enterotoxin in their nose or hand and through meat grinder’s knives to the food products and food contact surfaces.
- They are also transmitted via physical contact and through respiratory secretions while coughing and sneezing.
- In raw food, the competency of S. aureus is low with indigenous microbiota, therefore; improper handling of cooked or processed foods and storage at inappropriate temperature also serves as the main reservoir of contamination.
- S. aureus are also found in poultry and dairy animals like cattle, sheep, and goats if affected by subclinical mastitis.
- Foods that are frequently contaminated by SEs include meat and meat products, poultry and egg products, milk and dairy products, raw salads, cream-filled pastries, sandwich fillings, ice creams, and salted food products.
Toxin production during Staphylococcal food poisoning
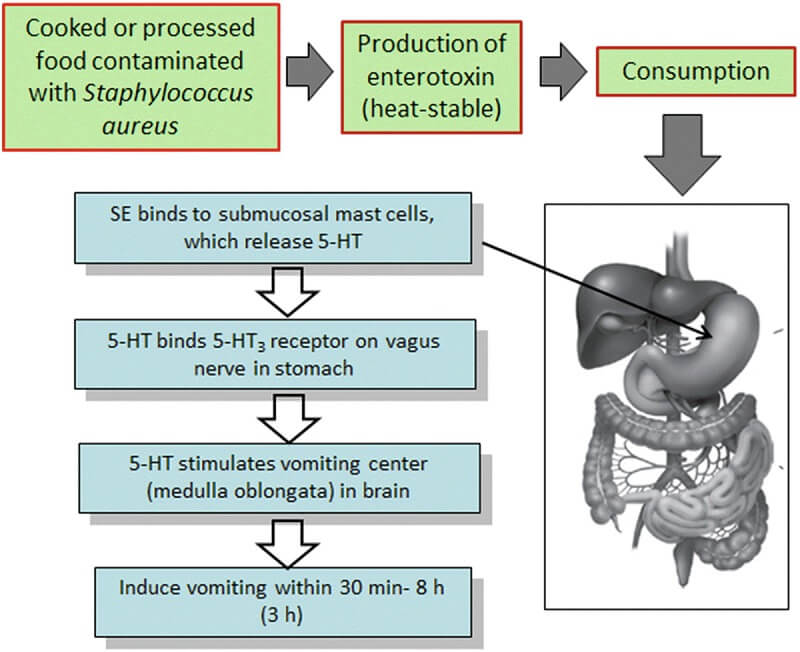
Image Source: Arun K. Bhunia 2018.
- The growth temperature of S. aureus ranges between 7 – 48°C, with an optimum of 37°C but its survival depends on a number of environmental factors such as pH, temperature, water activity (aw), salinity, oxygen availability, and composition of the food.
- This organism cannot resist high temperatures above 60°C; however, under environmental stress conditions, it starts to multiply and produce a large number of extracellular proteins and toxins.
- To date, 17 serologically distinct enterotoxins have been identified namely SEA to SER with no SEF.
- The SEC contains antigenically distinct 3 subtypes: SEC1, SEC2, and SEC3 and SEG have a SEGv variant form.
- Each enterotoxin encoding gene are carried and distributed by different mobile genetic elements such as prophages, plasmids, pathogenicity islands (SaPIs), enterotoxin gene cluster (egc), and the staphylococcal cassette chromosome (SCC).
- Enterotoxins are resistant to heat treatment, drying, freezing, and protease-resistant but are soluble in water.
- However, recent cases have been reported that SEA and SED were found to be accumulated in broth, minced food, and raw pasteurized milk.
- The classical enterotoxins (prophage encoded enterotoxins), SEA – SEE are the major reported SFP outbreak.
Symptoms and complications of Staphylococcal food poisoning
Enterotoxin infection occurs within 1-7 hours of ingestion and lasts no longer than 1 to 2 days. The severity of illness depends on the amount of toxin ingested present in the food and general health and age group of the victim.
Some of the common symptoms include:
- Nausea
- Vomiting
- Diarrhea
- Weakness
- Sweating
- Abdominal cramp
- Fatigue
- Chills
- Myalgia
- Headache
- Fever
In case of aerosol exposure, sudden fever, chills, and cough occur which may last for 10-14 days.
Epidemiology of Staphylococcal food poisoning
- The first food-related illness was reported in Michigan (USA) in 1884 when a serious incident took place because of the consumption of staphylococci contaminated cheese.
- The authors failed to trace the main cause and stated Micrococcus or some other microorganisms.
- After a decade, Denys concluded the presence of pyogenic staphylococci when illness occurred in a family after consuming the meat of a dead ill cow.
- In 1907, an outbreak of SFP symptomatology occurred from dried beef from where Owen isolated staphylococci.
- Barber in 1914, proved that staphylococci are the main cause of food poisoning by experimenting himself. He consumed unrefrigerated milk from a cow suffering from mastitis and showed similar characteristics to SFP.
- One of the huge totals of 5,550 outbreaks has been reported by EFSA in Europe in 2009 where almost 49,000 people were affected and 46 deaths were reported.
- Most of the outbreaks were caused by Staphylococcal enterotoxins while other toxins were produced by Bacillus and Clostridium species.
- The mortality rate is 0.02%, occurring in the most susceptible infants, elderly and immunosuppressed people.
Mechanism of Pathogenesis
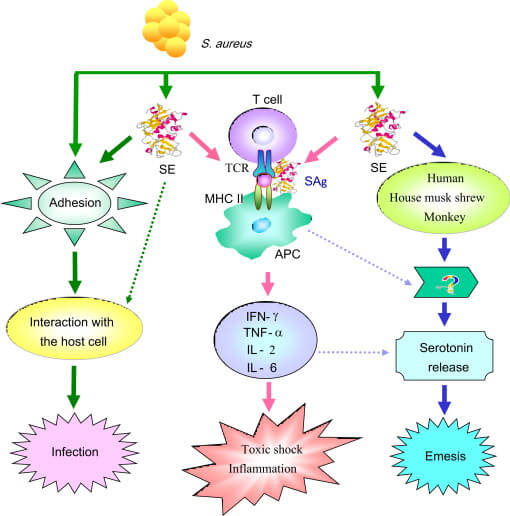
Image Source: Dong-LiangHu et al. 2014.
- About 105 to 108 cfu/g of S. aureus and toxin concentration dose of 1µg/g is enough to cause infection.
- The emetic dose of SEA toxin needed to show intoxication syndrome in humans is 200µg/kg and SEB toxin is 0.4µg/kg.
- After the consumption, toxins are absorbed in the abdomen and cause typical gastroenteritis.
- The toxin stimulates the vomiting center of the brain via the vagus nerve endings in the stomach lining and sympathetic nerves and shows a violent emetic response.
- Enterotoxins also cause damage to the epithelial lining, villus distension, crypt elongation, and lymphoid hyperplasia of the intestinal cells.
- Super antigenic property of SEs stimulates a large number of T-cells as compared to other bacterial toxins.
- The SEs enter the blood and binds to MHC class II molecules then attach to the T-cells with the help of its T-cell receptor.
- T-cells proliferate producing a large amount of IL-2 and IFN-ƴ.
- More IFN-ƴ induces more MHC class II molecules which bind more superantigens and activates more T-cells.
- A high percentage of inflammatory cytokines stimulates the neuron receptors in the intestinal tract and causes diarrhea.
Laboratory diagnosis of Staphylococcal food poisoning
Conventional culture method
Isolation on Baird-Parker Agar gives black, shiny, circular, smooth colonies with an entire margin and a wide opaque zone around the colonies.
Bioassays
- Examining the toxin in animals or cell cultures based on the capacity of the sample to induce SFP symptoms.
- The SEA toxin dose of 2.3µg is capable of causing symptoms in animals which is considerably high amount than that involved in human food poisoning.
Molecular biology
- The gene-specific nucleotide sequence is used as a probe in the nucleic acid hybridization technique.
- By colony blot hybridization, these oligonucleotide probes target different enterotoxin genes that help in detecting and differentiating SEs.
- PCR is much faster and reliable to detect SEs by amplifying corresponding genes but are expensive and requires trained personnel.
Serologic test
- The serologic test includes the gel diffusion test and agglutination test.
- Gel diffusion test shows visible precipitation of antigen-antibody interaction.
- Agglutination uses latex particles coated with specific anti-SEs antibodies.
- Serologic tests lack specificity and sensitivity therefore they are not relevant for the detection of SEs.
Chromatography method
- Liquid chromatography-electrospray ionization mass spectrometry (LC-ESI-MS) is used for SEs detection.
- A low concentration of soluble protein food samples produces a large number of peptides to isolate the toxins from food.
Immunoassays
- Immunosensing elements are used in the detection process and a device gives an output in the form of measurable energy.
- Some of the widely used immunoassays in SEs detection are
- Colorimetric
- Fluorescence
- Chemiluminescence
- Electrochemiluminescent
- Refractive index
- Raman scattering
Treatment
- Fluid therapy and rest cure are suggested.
- Treatment with proper antibiotics may lower the symptoms but could affect adversely if the toxins are resistant.
- Therefore, the natural flora of the intestinal tract eliminates the growth of Staphylococci.
Prevention and Control
- Proper refrigeration of susceptible foods.
- Maintaining temperature between prepared and before serving food.
- Proper food handling practices.
- Prohibit food handlers with infections.
- Wear gloves, masks, apron during food preparation.
References
- Paparella, A., Serio, A., Rossi, C., Mazzarrino, G., & Chaves López, C. (2018). Food-Borne Transmission of Staphylococci. Pet-To-Man Travelling Staphylococci, 71–94.
- Bergdoll, M. S., & Wong, A. L. (2003). STAPHYLOCOCCUS | Food Poisoning. Encyclopedia of Food Sciences and Nutrition, 5556–5561.
- FEMS Microbiology Reviews, Volume 36, Issue 4, July 2012, Pages 815–836
- https://www.gov.mb.ca/health/publichealth/diseases/staphylococcal.html
- Wu, S., Duan, N., Gu, H., Hao, L., Ye, H., Gong, W., & Wang, Z. (2016). A Review of the Methods for Detection of Staphylococcus aureus Enterotoxins. Toxins, 8(7), 176.
- Schelin, J., Wallin-Carlquist, N., Thorup Cohn, M., Lindqvist, R., & Barker, G. C. (2011). The formation of Staphylococcus aureus enterotoxin in food environments and advances in risk assessment. Virulence, 2(6), 580–592.
- https://www.cdc.gov/foodsafety/diseases/staphylococcal.html
- Argudín, M. Á., Mendoza, M. C., & Rodicio, M. R. (2010). Food Poisoning and Staphylococcus aureus Enterotoxins. Toxins, 2(7), 1751–1773.
- Hu DL, Nakane A. Mechanisms of staphylococcal enterotoxin-induced emesis. Eur J Pharmacol. 2014 Jan 5;722:95-107. doi: 10.1016/j.ejphar.2013.08.050. Epub 2013 Oct 30. PMID: 24184671.
- Bhunia A.K. (2018) Staphylococcus aureus. In: Foodborne Microbial Pathogens. Food Science Text Series. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-7349-1_10
Sources
- https://www.sciencedirect.com/topics/immunology-and-microbiology/staphylococcus-schleiferi – 4%
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3153290/ – 4%
- https://www.researchgate.net/publication/304455727_A_Review_of_the_Methods_for_Detection_of_Staphylococcus_aureus_Enterotoxins – 3%
- https://sfamjournals.onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2672.2011.05076.x – 2%
- https://www.sciencedirect.com/topics/nursing-and-health-professions/bioassayINTERNET1%https://www.sciencedirect.com/science/article/pii/B9780128096710000073 – 1%
- https://www.sciencedirect.com/topics/neuroscience/emetic – 1%
- https://www.tandfonline.com/doi/pdf/10.4161/viru.2.6.18122 – 1%
- https://www.mdpi.com/2076-0817/9/12/1064/htm – 1%
- https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/enterotoxin – 1%
- https://www.foodstandards.gov.au/publications/Documents/Staphylococcus%20aureus.pdf – <1%
