Passive immunity is developed by antibodies that are produced outside and then introduced into the body. Passive immunity is acquired when antibodies are introduced into the body from an external source (usually through vaccines) providing a quick response to the infection.
Passive immunity is more of a form of therapy where antibodies are introduced from outside the host. They can otherwise be known as ‘loaned’ antibodies.
The loaned antibodies help prevent or fight certain infectious diseases, however, the protection offered by this form of immunity is short-lived, lasting a few weeks or months. It otherwise offered temporal protection.
For example, emergency use of immune serum, containing antibodies against snake or scorpion venoms, is a common practice for treating bite victims. This form of immune protection that is transferred between individuals is called passive immunity because the individual receiving it did not make his or her own immune response against the pathogen.
Newborn infants benefit from passive immunity to the presence of maternal antibodies in their circulation.
Passive immunity may also be used as a preventive (prophylaxis) to boost the immune potential of those with compromised immunity or who anticipate future exposure to a particular microbe.
While passive immunity can supply a quick solution, it is short-lived and limited, as the cells that produce these antibodies are not being transferred.
Interesting Science Videos
Characteristics of Passive Immunity
- Passive immunity is conferred from outside the body, so it doesn’t require exposure to an infectious agent or its antigen.
- There is no delay in the action of passive immunity which means the response to an infectious agent is immediate.
- Passive immunity is not as long-lasting as active immunity lasting a few days, weeks, or months.
- However, negatively, serum sickness can result from exposure to antisera.
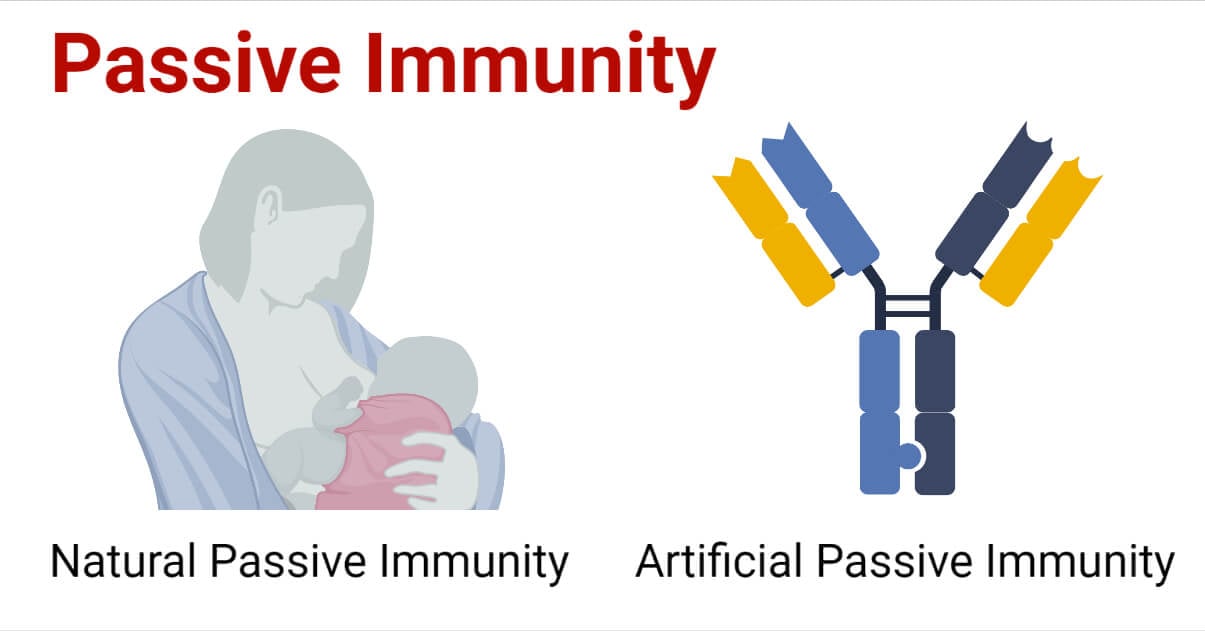
Types of Passive Immunity
A. Natural Passive Immunity
- This occurs during pregnancy when antibodies pass from maternal blood into the fetal bloodstream.
- It is observed when IgG passes from the mother to the fetus (during pregnancy), forming a basis for the prevention of neonatal tetanus in neonates by active immunization of pregnant mothers.
- This is achieved by administering the tetanus toxoid to pregnant mothers during pregnancy (first times – three doses) or during the last trimester for second-time mothers.
- This induces the production of high-level antibodies in the mother against the tetanus toxin, which is subsequently transmitted to the fetus, from the mother through the placenta.
- The antibodies then protect the neonate after birth against the risks of tetanus.
- Natural passive immunity is also observed by the passing of IgA from the mother to the newborn through breastfeeding.
B. Artificial Passive Immunity
- Artificial passive immunization is normally administered by injection.
- It is used if there has been a recent outbreak of a particular disease or as an emergency treatment for toxicity, such as tetanus.
- It is induced in an individual by administering preformed antibodies, in form of antiserum, raised against an infecting agent.
- The antibodies can be produced in animals, called “serum therapy,” although there is a high chance of anaphylactic shock because of immunity against animal serum itself. Therefore, humanized antibodies produced in vitro by cell culture are used instead, when and if available.
- Administration of these antisera makes large amounts of antibodies available in the recipient host to neutralize the action of toxins.
- The preformed antibodies against rabies and hepatitis A and B viruses, etc. given during the incubation period prevent replication of the virus, and hence alter the course of infection.
- The immediate availability of a large number of antibodies is the main advantage of passive immunity.
- However, the short lifespan of these antibodies and the possibility of hypersensitivity reaction, if antibodies prepared in other animal species are given to individuals who are hypersensitive to these animals’ globulins (e.g., serum sickness), are the two noted disadvantages of passive immunity.
Applications of Passive Immunity Today
- Patients today can be treated with antibodies when they are sick with diphtheria or cytomegalovirus.
- Antibody therapy can also be used as a preventive measure on exposure to pathogens in order to stop the development of an illness such as the Respiratory Syncytial Virus (RSV), measles, tetanus, hepatitis A and B, rabies, and Chickenpox.
- However, routine treatment with antibodies for these diseases is healthy, but it could benefit high-risk individuals especially those with immune deficiencies.
The Future of Passive Immunization
A. Monoclonal Antibodies
- Monoclonal antibody production technology is increasing, thus a pure, single type of antibodies from the single-parent cells that are targeted at a single site on a pathogen are produced. These antibodies have wide-ranging potential applications to infectious diseases and other types of diseases.
- Currently, there is only one MAb treatment is commercially available for the prevention of an infectious disease. This is a MAb preparation for the prevention of severe disease caused by RSV in high-risk infants.
- Physicians are also increasingly using MAbs to combat noninfectious diseases, such as certain types of cancer, multiple sclerosis, rheumatoid arthritis, Crohn’s disease, and cardiovascular disease.
- Scientists are researching other new technologies for producing antibodies in the laboratory, such as recombinant systems using yeast cells or viruses and systems combining human cells and mouse cells, or human DNA and mouse DNA.
B. Bioterror threats
- Passive immunization can also play a major role in a bioterrorism attack (release of an infectious biological agent), as an emergency response. The advantage of using antibodies rather than vaccines to respond to a bioterror event is that antibodies provide immediate protection, whereas vaccine protection is not immediate and in some cases may depend on a booster dose given at a later date.
- Candidates for this potential application of passive immunization include botulinum toxin, tularemia, anthrax, and plague. For most of these targets, only animal studies have been conducted, and so the use of passive immunization in potential bioterror events is still in the experimental stages.
Advantages of Passive Immunization
- Passive immunization acts quicker, producing an immune response within hours or days of the administration, unlike vaccines, which take weeks or months to produce protective immunity.
- Passive immunization also can override a deficient immune system, which is very helpful to persons that do not respond to vaccine immunizations.
Disadvantages of Passive Immunization
- Antibodies are costly to produce, however, new technologies can help produce them in the laboratory especially antibodies to infectious diseases that must be harvested from the blood of thousands of donors or even obtained from the blood of immune animals like those produced to neutralize snake venoms.
- Antibodies from animals can cause serious allergic reactions in the recipient.
- Antibodies must be administered via intravenous injection, which can be a complicated procedure and more time-consuming that the injection of a vaccine.
- The immunity conferred by passive immunization is short-lived i.e it does not lead to the formation of long-lasting memory immune cells.
References
- Kuby Immunology 5th Edition
- Microbiology and Immunology 2nd Edition by Shubash Chandra Parija
- https://www.thoughtco.com/active-immunity-and-passive-immunity-4134137
- https://www.technologynetworks.com/immunology/articles/active-vs-passive-immunity-differences-and-definition-335112
- https://www.chop.edu/centers-programs/vaccine-education-center/human-immune-system/types-immunity
- https://www.health.com/condition/infectious-diseases/active-vs-passive-immunity
- https://byjus.com/biology/difference-between-active-and-passive-immunity/
- https://med.libretexts.org/Bookshelves/Anatomy_and_Physiology/Book%3A_Anatomy_and_Physiology_(Boundless)/20%3A_Immune_System/20.7%3A_Cell-Mediated_Immune_Response/20.7C%3A_Active_and_Passive_Humoral_Immunity
- https://www.historyofvaccines.org/content/articles/passive-immunization
- https://www.cdc.gov/vaccines/vac-gen/immunity-types.htm
- https://www.biologyonline.com/dictionary/local-immunity
