Interesting Science Videos
What is an MHC Molecule?
- Human leukocyte antigen is a major histocompatibility complex present on chromosome 6 of the human genome.
- Size: 3.6 Mb approx.
- They are divided into 3 classes, telomeric class 1, centromeric class 2, and class 3 region.
- They are highly polymorphic in humans means different alleles exist in the different individuals inside a population. Thus, no two individuals can have the same type of MHC molecules, except for identical twins.
MHC Molecule History
- George snell identified murine MHC locus, H2.
- Dausset identified HLA in WBC in human chromosome.
- Baruj benacerraf identified the relevance of these molecules in the immune response.
- Three of them were awarded a joint Nobel prize in 1980 in medicine.
MHC Molecule Functions
The basic function of the MHC molecule is to digest the foreign peptide and present it to T cells, known as antigen presentation. This helps T cells to specifically recognize the foreign antigen and form antibodies against it, thus neutralizing it.
Difference between MHC class I and MHC class II molecules
| MHC class I | MHC class II |
| Present on the surface of all nucleated cells | Present on antigen-presenting cells |
| Present antigen to CD8+ cells (cytotoxic T lymphocytes) | Present antigen to CD4+ cells (T helper cells) |
| Bind to endogenous antigen | Bind to exogenous antigen |
Process of thymic selection
Thymic selection mainly relies on the recognition of self-peptide-MHC complexes, whereby weak interactions with self-peptide-MHC allow Tcell survival (positive selection); on the other hand, strong interaction induces apoptosis (negative selection).
What is Autoimmunity?
- Autoimmune disorders are a result of the loss of the ability of the cell to discriminate between self and non-self.
- This discrimination in the cell is mediated by the T-cell receptor, which recognizes the digested peptide fragment of antigen presented by the MHC molecule present in the antigen-presenting cell (APC), and the process is known as antigen presentation.
- Failure in differentiating between self and non-self is due to pure thymic selection of self-peptide-MHC complex and non-self-peptide-MHC complex, which is an important selection process that takes place in the thymus during T-cell maturation.
Association of MHC with the autoimmune disorder
- The mechanism of association between MHC and autoimmune disorder is not fully observed.
- The main belief thus far is that it is due to the defect in immunological tolerance, which is the ability of the cell to recognize between self and nonself antigenic peptides.
- Many diseases, including type I diabetes (TID), multiple sclerosis, rheumatoid arthritis, graves’ disease, ankylosing spondylitis, systemic lupus erythematosus, etc, are a result of loss of cell selection in the thymus.
Examples of autoimmune disorders
1. Multiple Sclerosis:
- It is a chronic inflammatory demyelinating disease
- Affect the central nervous system
- At CNS, activated T cells and macrophages cross the blood-brain barrier and target the layering of nerve cells known as myelin sheath and attack it to produce inflammation, which makes it difficult for the brain to send the signals to the body.
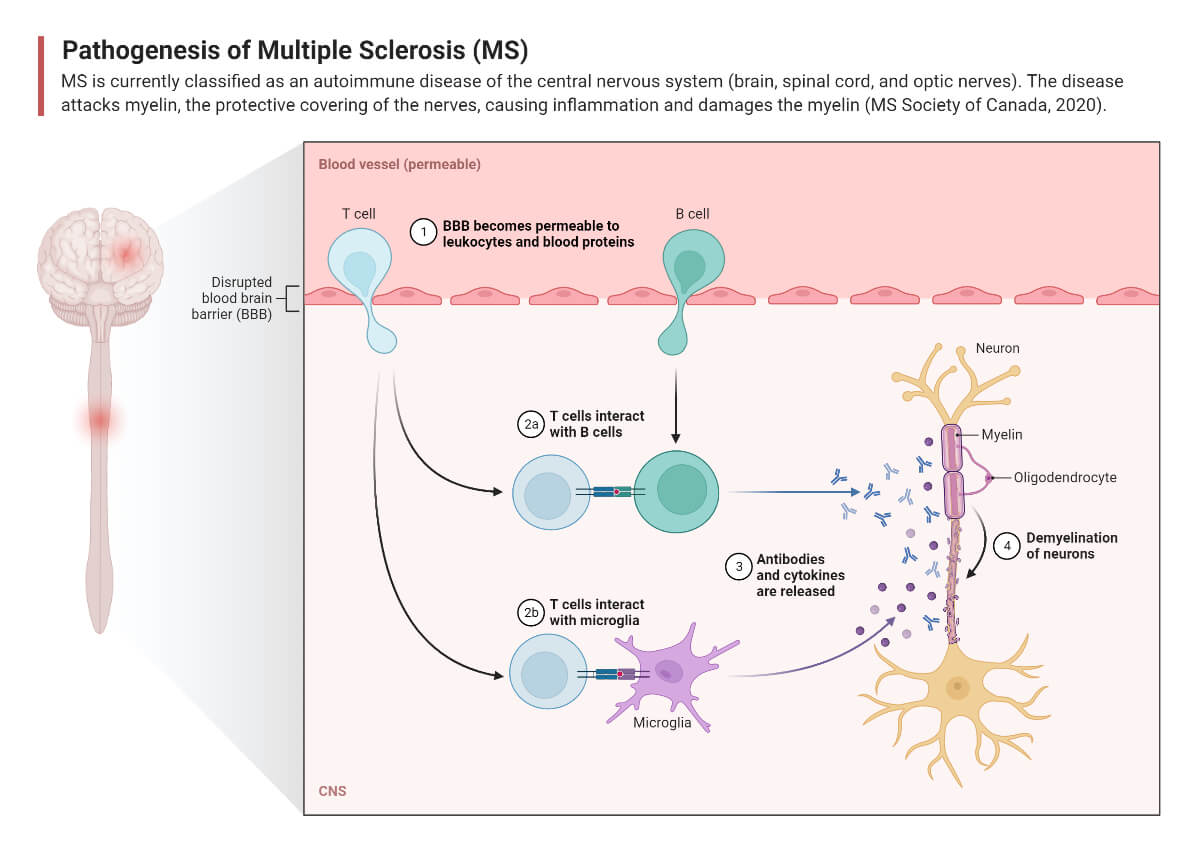
- Symptoms: depend on person to person
- Numbness or weakness in one side of the body, including hands, legs, etc
- Electric shocks like sensations while bending the neck
- Lack of coordination
- Inability to walk properly
- Blurry vision
- There is no permanent cure, although temporary treatment can be taken to treat symptoms.
2. Rheumatoid Arthritis:
- chronic systemic autoimmune disorder
- affects the lining of synovial joints
- associated with progressive disability, premature death, and socioeconomic burdens
- mainly females than males, and mainly observed in elderly people.
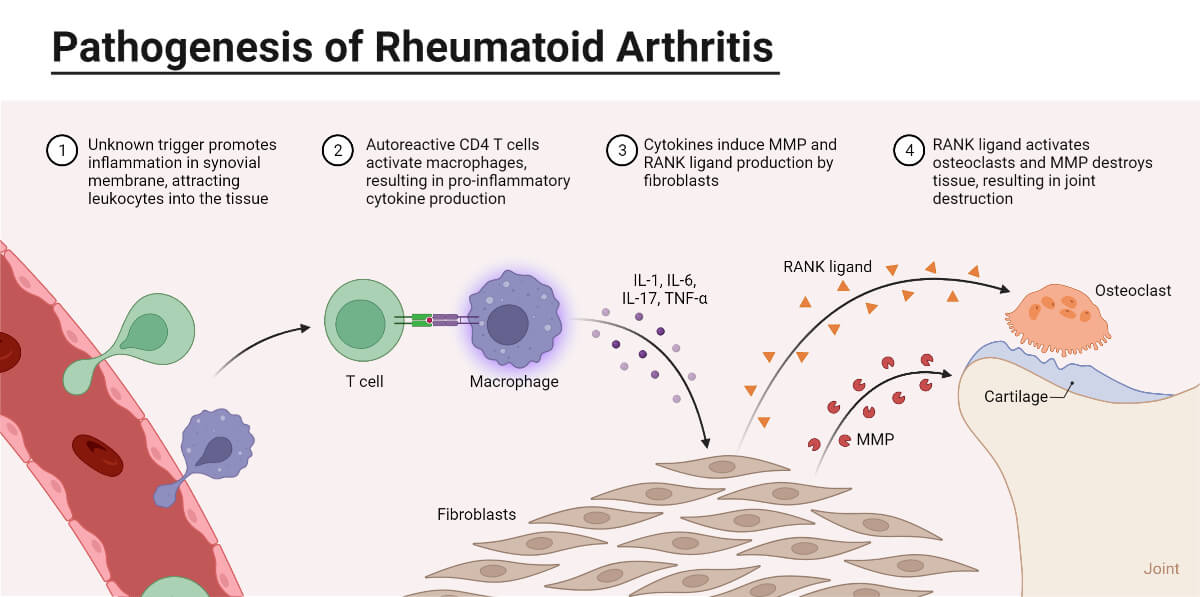
- Symptoms:
- Arthralgia (pain in joints)
- Swelling and redness in joints
- Limiting joint motion
- Weight loss
- Fever
- fatigue
- No permanent cure, but temporary treatment can help to treat symptoms
- Breastfeeding can decrease the rate of occurrence of RA in females.
3. Type 1 Diabetes:
- T-cell-mediated autoimmune disease.
- destruction of pancreatic β-cells causes insulin deficiency, which leads to hyperglycemia and a tendency to ketoacidosis.
- commonly presents in childhood or adolescence; however, the disease can appear at any age.
- Patients with T1D constitute 5-10% of all people with diabetes, the remainder having type 2 diabetes, monogenic forms of diabetes, or diabetes associated with other sources of islet cell injury.
- Autoimmune cells destroy the cells in the pancreas, aka beta cells, that make insulin, and since insulin helps the sugar to enter the blood, thus sugar accumulates in the body, resulting in high blood sugar levels.
- Antibody markers of autoimmunity against β-cell include islet-cell autoantibodies, autoantibodies against insulin, glutamic acid decarboxylase (GAD), or tyrosine phosphates IA-2 and IA-2β, and ZnT8.
- Studies show links the human leukocyte antigen (HLA) genes DQA and DQB to susceptibility to the disease.
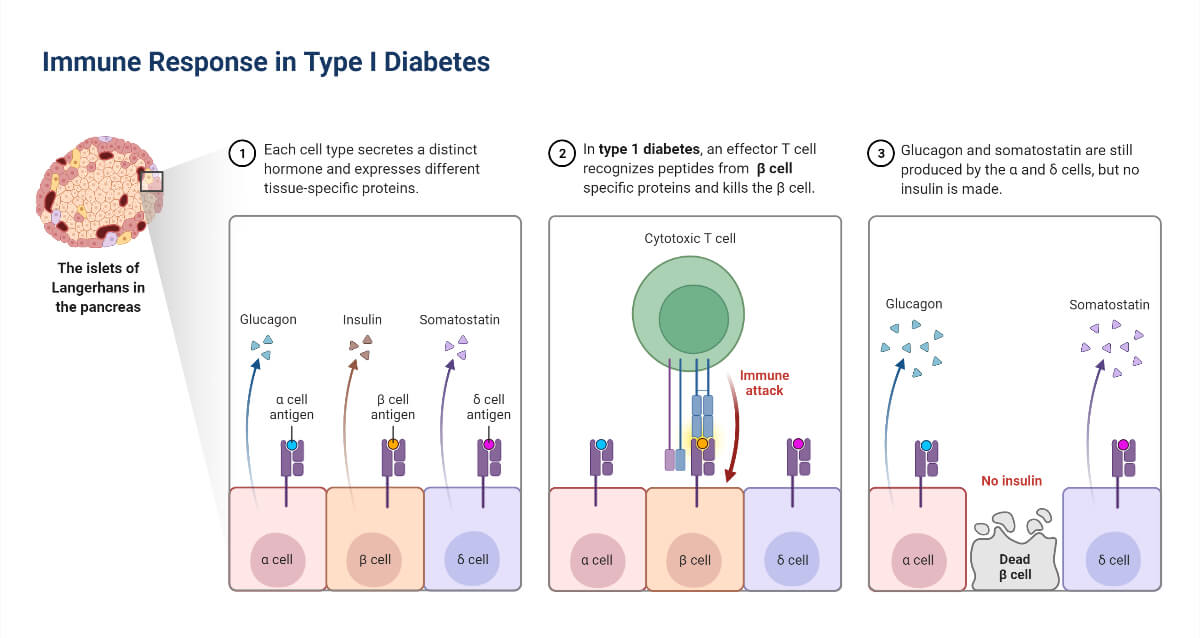
- Symptoms:
- weightloss
- Frequent urination
- Impaired vision
- Hunger attacks
4. Systemic Lupus Erythematosus:
- Systemic autoimmune disease with multiorgan inflammation
- Autoimmune antibodies form again nucleic acid and its binding proteins resulting in loss of self-tolerance.
- Innate immunity plays a key role in the formation of inflammatory cytokines that causes tissue injury and activation of autoreactive B and T cells that leads to organ injury.
- Symptoms:
- fever
- skin rashes
- pain or swelling in joints
- sun sensitivity
- oral ulcers
- heart, kidney, lungs problems
- psychosis
5. Psoriasis
- Chronic inflammatory skin disease
- Show comorbidity with another autoimmune disease such as arthritis.
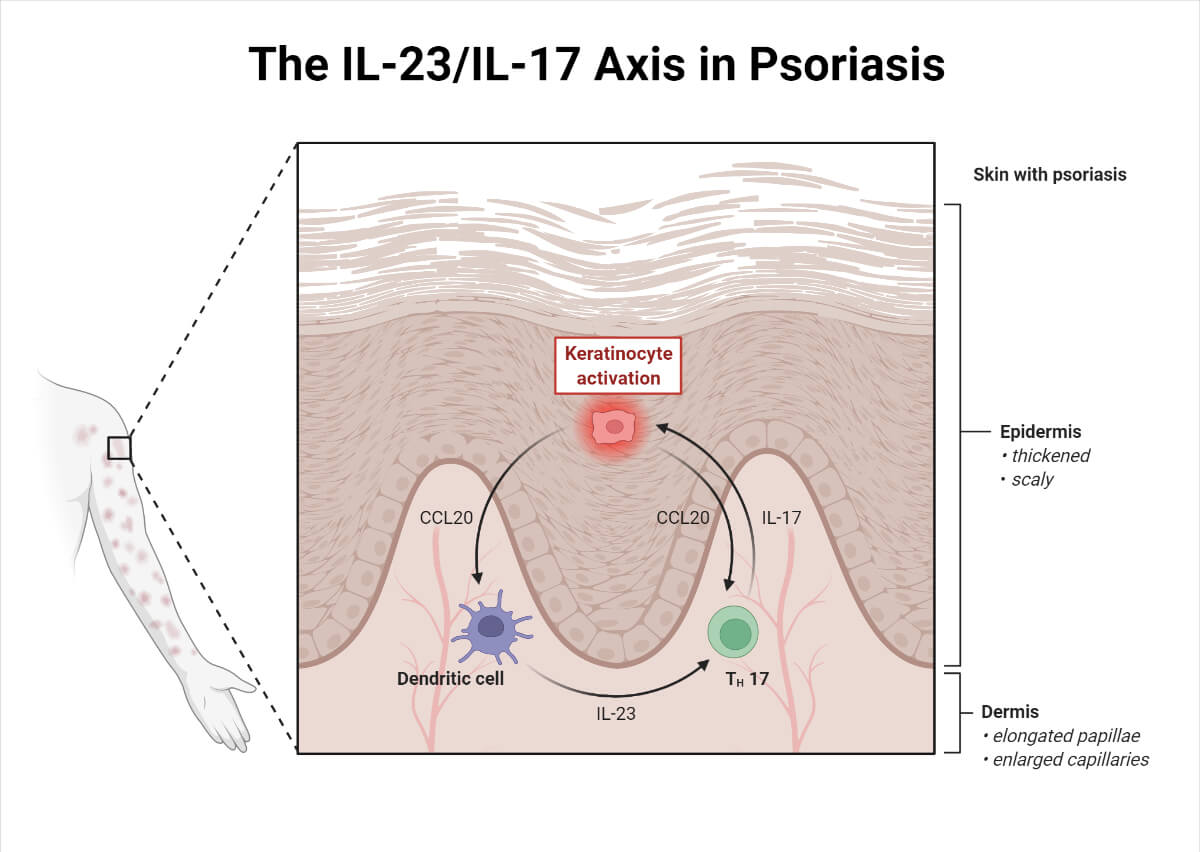
- Symptoms:
- Scaly red patches confined to a specific area
- Nails with thick pitted or ridged lining
- Stiff and swollen joints
- Bleeding in skin due to extreme dryness
- Itching
- Burning
- Painful lesions
- There is no permanent treatment available as this disease show symptoms irregularly and sometimes remain dormant in the body for years, but few medications help treat symptoms, such as methotrexate which is an immunosuppressant.
6. Dermatomytosis
- Result due to bodies defect to recognize its cell as foreign, genetic factor, cancer in older people, environmental factors, infection or any medication, etc.
- It causes muscle inflammation and rashes.
- Symptoms:
- Painful sunburn rashes
- Upper eyelid swelling
- Spots of red and purple color on knee, elbow, toes, and knuckles
- Stiffness and pain in joints
- Hair thinning with dry skin
- Red fingernails
- Weakness in muscles around the hip, back, shoulder, and neck
- Weightloss
- Tiredness
- Diagnosis can be done by blood tests, electromyogram, MRI, a biopsy of skin or muscle, etc.
- Treatment is done using immunosuppressive drugs such as azathioprine, methotrexate, tacrolimus, etc.
7. Celiac Disease
- Aka celiac sprue, nontropical sprue, and gluten-sensitive enteropathy.
- A chronic digestive autoimmune disorder that targets the small intestine due to the consumption of gluten which is naturally found in wheat, barley, etc.
- Found in approx 1% of the world’s population.
- Symptoms:
- Bloating
- Chronic diarrhea
- Constipation
- Gas
- Lactose intolerance
- Nausea and vomiting
- Pain in abdomen
- Genetic testing and biopsies of the small intestine are usually done for diagnosis
- No permanent cure
8. Inflammatory Bowel Disease: Ulcerative Colitis and Crohn’s Disease
- Chronic inflammation of the gastrointestinal tract is characterized by two diseases, i.e, Crohn’s disease and ulcerative colitis.
- Chrohn’s disease: affect any part of the GI tract, usually the small intestine, and the area of damage appears in patches. The inflammation affects all layers of the GI tract.
- Ulcerative colitis: this occurs in the large intestine and rectum, and it doesn’t appear in patches. Only affect the innermost layer of the large intestine.
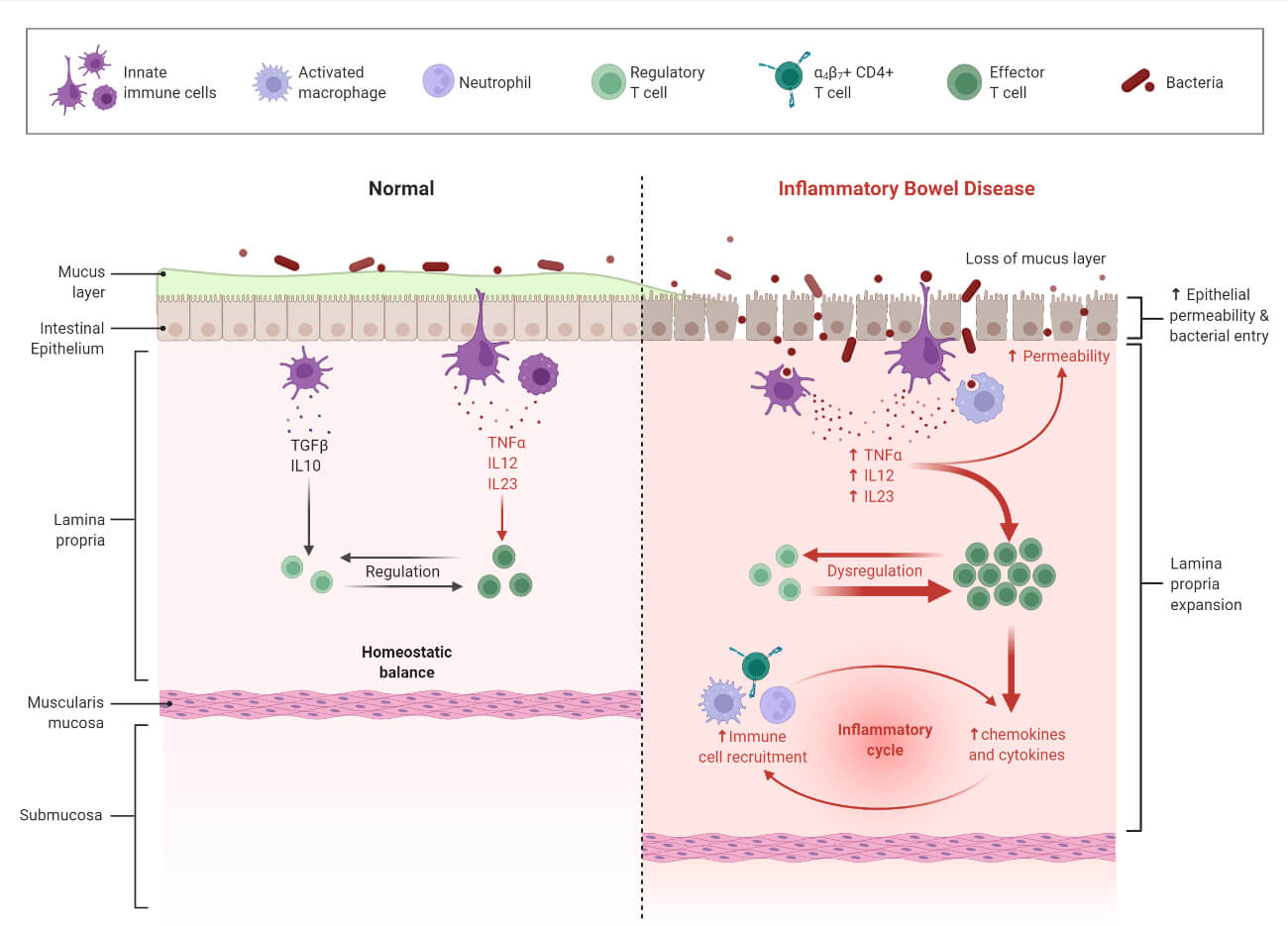
- Symptoms:
- Persistent diarrhea
- Abdominal pain
- Rectal bleeding/bloody stools
- Weight loss
- Fatigue
- The diagnosis was done by endoscopy and colonoscopy.
References
- Klug, W.S., Cummings, M.R., Spencer, C.A., et al. (2017) Essentials of Genetics. 7th Edition, Higher Education Press, Beijing, 446-464
- Fernando, M. M. A., Stevens, C. R., Walsh, E. C., De Jager, P. L., Goyette, P., Plenge, R. M., … Rioux, J. D. (2008). Defining the Role of the MHC in Autoimmunity: A Review and Pooled Analysis. PLoS Genetics, 4(4), e1000024. doi:10.1371/journal.pgen.1000024
- Klein, L., Kyewski, B., Allen, P. et al. Positive and negative selection of the T cell repertoire: what thymocytes see (and don’t see). Nat Rev Immunol 14, 377–391 (2014). https://doi.org/10.1038/nri3667
- Sticherling M. Psoriasis and autoimmunity. Autoimmun Rev. 2016 Dec;15(12):1167-1170. DOI: 10.1016/j.autrev.2016.09.004. Epub 2016 Sep 15. PMID: 27639838.
- https://www.niddk.nih.gov/health-information/digestive-diseases/celiac-disease/diagnosis
- https://www.cdc.gov/lupus/facts/detailed.html
- https://www.cdc.gov/arthritis/basics/rheumatoid-arthritis.html
- https://www.cdc.gov/diabetes/basics/what-is-type-1-diabetes.html
- https://www.nccih.nih.gov/health/multiple-sclerosis
- https://www.cdc.gov/ibd/what-is-ibd.htm
- https://www.cdc.gov/psoriasis/index.htm
